Comparison of Common Risk Factors and Comorbidities among Patients with and without Hypertension in Bangladesh
Article Information
Miah Wahiduzzaman1, AKM Shamsul Kabir2, Adib Siddiki3, Kamruzzaman Khokon4, Solaiman Hossain5, Mohiuddin Humayun Kabir Chowdhury6, Mosharul Haque7, Mohammad Morshedul Ahsan8, Paritosh Kumar Ghosh9, Abida Yasmin10
1Assistant Professor, Department of Medicine, Holy Family Red Crescent Medical College & Hospital, Dhaka
2Professor, Department of Medicine, Holy Family Red Crescent Medical College & Hospital, Dhaka
3Intern Doctor, Holy Family Red Crescent Medical College Hospital, Dhaka
4Assistant Professor, Department of Medicine, Cumilla Medical College, Cumilla
5Professor, Department of Cardiology, Enam Medical College and Hospital, Dhaka
6Associate Professor, Department of Medicine, Abdul Malek Ukil Medical College, Noakhali
7Assistant Professor, Department of Cardiology, M A G Osmani Medical College, Sylhet
8Assistant Professor, Department of Cardiology, Shaheed Ziaur Rahman Medical College Hospital, Bogura
9Assistant Professor, Department of Cardiology, Kushtia Medical college & hospital, Kushtia
10Final Year MBBS Student, Sher-e-Bangla Medical College and Hospital, Barishal
*Corresponding author: Miah Wahiduzzaman, Assistant Professor, Department of Medicine, Holy Family Red Crescent Medical College Hospital
Received: 21 February 2024; Accepted: 29 February 2024; Published: 08 April 2024
Citation: Miah Wahiduzzaman, AKM Shamsul Kabir, Adib Siddiki, Kamruzzaman Khokon, Solaiman Hossain, Mohiuddin Humayun Kabir Chowdhury, Mosharul Haque, Mohammad Morshedul Ahsan, Paritosh Kumar Ghosh, Abida Yasmin. Comparison of Common Risk Factors and Comorbidities among Patients with and without Hypertension in Bangladesh. Cardiology and Cardiovascular Medicine. 8 (2024): 124-129.
View / Download Pdf Share at FacebookAbstract
Background: Hypertension is a significant public health issue globally and particularly in low-middle-income countries like Bangladesh. This study aims to observe the prevalence of hypertension in Bangladesh and compare the risk factors and comorbidities in patients with and without hypertension. Given the increasing rates of hypertension and its complex interplay with various health conditions, understanding these relationships is crucial for effective healthcare strategies.
Methods: This retrospective observational study was conducted among 210 patients visiting an outpatient department of medicine, Holy Family Red Crescent Medical College & Hospital, Dhaka, Bangladesh. Participants were selected consecutively from those visiting for symptoms related to high blood pressure. Data on age, gender, body mass index (BMI), lifestyle factors, and comorbidities such as diabetes, obesity, and chronic kidney disease were extracted from medical records. Descriptive statistics and analytical methods were employed using SPSS software.
Result: The study found a hypertension prevalence of 32.38% among the participants. Key sociodemographic findings included a higher representation of females and a majority age group of 50-59 years. Overweight and obesity were prominent among participants. A significant association between hypertension and diabetes mellitus was observed, with 83.82% of hypertensive participants having diabetes, compared to 42.96% in the non-hypertensive group. Other comorbidities like ischemic heart disease also showed significant associations with hypertension. However, some comorbidities like chronic kidney disease and stroke did not show a significant association.
Conclusion: The study reveals a high prevalence of hypertension in the outpatient setting in Bangladesh, emphasizing the strong association with diabetes mellitus. It underscores the need for integrated healthcare approaches focusing on sociodemographic and metabolic risk factors. The findings call for targeted interventions and comprehensive healthcare strategies to manage hypertension and its related comorbidities in this population. This study contributes to the understanding of hypertension's prevalence and its interrelation with various health factors in Bangladesh.
Keywords
Hypertension; Diabetes; Risk Factors; High Blood Pressure; Cardiovascular
Hypertension articles; Diabetes articles; Risk Factors articles; High Blood Pressure articles; Cardiovascular articles
Article Details
1. Introduction
Hypertension, commonly known as high blood pressure, is a significant public health concern that affects millions of people worldwide. It is a leading risk factor for cardiovascular diseases, including heart attack, stroke, and kidney failure. The prevalence of hypertension varies globally, with a notable increase in low-middle-income countries, including Bangladesh [1]. Globally, hypertension is a growing concern, especially in low-middle-income countries [2,3]. A study conducted in Brazil found that 11% of hypertension patients had resistant hypertension, characterized by blood pressure remaining high despite taking multiple antihypertensive medications [4]. These patients were more likely to be older, less educated, and have comorbidities like diabetes and poor glomerular filtration rate [4]. In Bangladesh, the prevalence of hypertension is also alarming. A nationwide cross-sectional survey found that 27% of the adult population in Bangladesh had hypertension [5]. Interestingly, the study revealed that individuals with higher socioeconomic status (SES) were more likely to have hypertension, diabetes, and obesity [5]. This is in contrast to more affluent countries, where individuals with lower SES are generally more affected by these conditions [6]. The risk factors for hypertension are multifaceted, encompassing both modifiable and non-modifiable elements. Lifestyle factors such as obesity, physical inactivity, and dietary habits are significant contributors to hypertension [4]. A study on obesity and inflammation highlighted that obesity is not just a condition of excess weight but also a state of chronic inflammation, which in turn increases the risk of hypertension [7]. Moreover, metabolic disorders like diabetes mellitus often coexist with hypertension, complicating its management and increasing the risk of cardiovascular diseases [8]. Polycystic ovary syndrome (PCOS) is another condition that has been linked to hypertension, primarily due to the insulin resistance that affects 50%-70% of women with PCOS [9]. Comorbidities such as diabetes, obesity, and chronic kidney disease often accompany hypertension, making its management more challenging. For instance, a study on COVID-19 patients identified hypertension as an independent risk factor for death, along with other comorbidities like diabetes and chronic kidney disease [10]. Another study focusing on the Bangladeshi population found that comorbidities like diabetes mellitus, chronic obstructive pulmonary disease (COPD), and coronary heart disease (CHD) were prevalent among COVID-19 patients, many of whom also had hypertension [11]. Age and gender also play a role in the prevalence and management of hypertension. Older individuals are generally more susceptible to hypertension and its associated comorbidities [8]. Moreover, women with conditions like PCOS are at a higher risk of developing hypertension, which can lead to various cardiovascular and metabolic complications [9]. In summary, hypertension is a significant public health issue in Bangladesh, with a complex interplay of various risk factors and comorbidities. While there is abundant research on hypertension globally, there is a notable gap in comprehensive studies focusing on the Bangladeshi population. This study aims to address this gap by observing the overall prevalence of hypertension among a selected group of patients, and compare the risk factors and comorbidities between those with and without hypertension.
2. Methods
This retrospective observational study was conducted at the Outpatient Department of Medicine, Holy Family Red Crescent Medical College and Hospital, Dhaka, Bangladesh. The study duration was 1 year, from July 2022 to June 2023. During this period, relevant information of a total of 210 patients had been recorded in the database in a consecutive manner, from those who visited the Outpatient department for various symptoms of high-blood pressure. The study aimed to observe the overall prevalence of hypertension among this selected group of patients and to compare the risk factors and comorbidities between those with and without hypertension. Data were extracted from medical records, which included variables such as age, gender, body mass index (BMI), lifestyle factors like smoking and alcohol consumption, and existing comorbidities such as diabetes, obesity, and chronic kidney disease. The presence or absence of hypertension served as the dependent variable, defined as a systolic blood pressure of 130 mm Hg or higher or a diastolic blood pressure of 80 mm Hg or higher. Descriptive statistics were used to summarize the demographic and clinical characteristics of the study population. All statistical analyses were conducted using SPSS software. Ethical approval for the study was obtained from the relevant institutional review boards, and the study adhered to ethical guidelines, including the use of de-identified data to maintain patient confidentiality.
3. Results
Table 1: Distribution of participants by Sociodemographic characteristics
|
Variables |
Frequency |
Percentage (%) |
|
Age (years) |
||
|
20-29 |
6 |
2.9 |
|
30-39 |
32 |
15.2 |
|
40-49 |
53 |
25.2 |
|
50-59 |
59 |
28.1 |
|
60-69 |
39 |
18.6 |
|
70-79 |
16 |
7.6 |
|
80-89 |
5 |
2.4 |
|
Mean ± SD |
51.28±12.49 |
|
|
Range (min-max) |
(24-85) years |
|
|
Sex |
||
|
Male |
85 |
40.5 |
|
Female |
125 |
59.5 |
|
Religion |
||
|
Muslim |
201 |
95.7 |
|
Hindu |
8 |
3.8 |
|
Christian |
1 |
0.5 |
|
Education |
||
|
Illiterate |
16 |
7.6 |
|
Primary |
72 |
34.3 |
|
SSC |
50 |
23.8 |
|
HSC |
36 |
17.1 |
|
Graduate |
23 |
11 |
|
Post Graduate |
13 |
6.2 |
|
Occupation |
||
|
Business |
41 |
19.5 |
|
Housewife |
112 |
53.3 |
|
Student |
1 |
0.5 |
|
Retired |
10 |
4.8 |
|
Service |
39 |
18.6 |
|
Farmer |
7 |
3.3 |
The age distribution showed that the majority of the participants were in the age groups of 50-59 years (28.1%) and 40-49 years (25.2%). The mean age was 51.28 years with a standard deviation of 12.49, and the age range was between 24 and 85 years. In terms of gender, females constituted the majority with 59.5%, while males accounted for 40.5%. The overwhelming majority of participants were Muslim (95.7%), followed by Hindu (3.8%) and Christian (0.5%). Regarding educational background, 34.3% had completed primary education, 23.8% had completed up to SSC (Secondary School Certificate), and 17.1% up to HSC (Higher Secondary Certificate). A smaller proportion had completed graduate (11%) and post-graduate (6.2%) levels, while 7.6% were illiterate. Occupationally, the largest group was housewives, making up 53.3% of the sample. This was followed by those in business (19.5%) and service (18.6%). A smaller proportion were retired (4.8%), farmers (3.3%), and students (0.5%).
Table II: Distribution of participants by BMI interpretation
|
BMI |
Frequency |
Percentage |
|
Underweight |
6 |
2.86% |
|
Normal Weight |
69 |
32.86% |
|
Overweight |
82 |
39.05% |
|
Obesity I |
37 |
17.62% |
|
Obesity II |
12 |
5.71% |
|
Morbidly Obese |
4 |
1.90% |
The data reveals that the largest proportion of participants were overweight, accounting for 39.05% of the sample. This was followed by those with normal weight, making up 32.86%. Participants classified under Obesity I constituted 17.62%, while those under Obesity II made up 5.71%. A smaller fraction of the sample was found to be underweight (2.86%) and morbidly obese (1.90%).
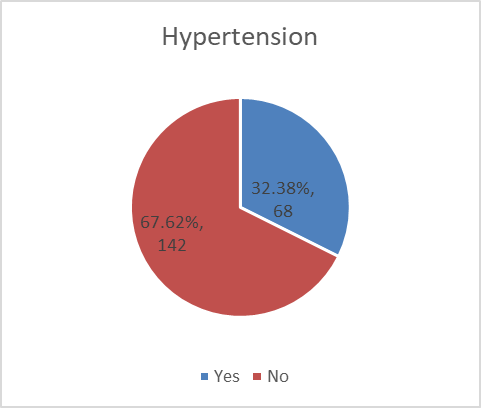
Out of the 210 participants, 68 were diagnosed with hypertension, constituting 32.38% of the sample. The remaining 142 participants, making up 67.62%, were not diagnosed with hypertension.
Table III: Distribution of lipid profile among the participants
|
Serum parameters |
Frequency |
Percentage (%) |
|
Fasting Blood Sugar |
||
|
Normal |
168 |
80.00% |
|
Above Normal |
42 |
20.00% |
|
HbA1C Levels |
||
|
Normal |
3 |
1.43% |
|
Prediabetic |
13 |
6.19% |
|
Diabetic |
128 |
60.95% |
|
Triglycerides |
||
|
Normal TG |
77 |
36.67% |
|
Borderline High TG |
37 |
17.62% |
|
High TG |
95 |
45.24% |
|
Total Cholesterol |
||
|
Normal |
114 |
54.29% |
|
Borderline High |
49 |
23.33% |
|
High |
46 |
21.90% |
|
High-Density Lipoprotein (HDL) |
||
|
Low HDL |
118 |
56.19% |
|
Normal HDL |
92 |
43.81% |
|
Low Density Lipoprotein (LDL) |
||
|
Optimal |
87 |
41.43% |
|
Borderline High |
49 |
23.33% |
|
High LDL |
74 |
35.24% |
For Fasting Blood Sugar levels, 80.00% of the participants had normal levels, while 20.00% had above-normal levels. When it comes to HbA1C levels, a significant majority (60.95%) were diabetic, 6.19% were prediabetic, and only 1.43% had normal levels. Regarding Triglycerides, 45.24% had high levels, 17.62% had borderline high levels, and 36.67% had normal levels. In terms of Total Cholesterol, 54.29% had normal levels, 23.33% had borderline high levels, and 21.90% had high levels. For High-Density Lipoprotein (HDL), 56.19% had low levels, and 43.81% had normal levels. Lastly, in the case of Low-Density Lipoprotein (LDL), 41.43% had optimal levels, 23.33% had borderline high levels, and 35.24% had high levels.
Table IV: Distribution of participants by presence of comorbidities
|
Variables |
Frequency |
Percentage (%) |
|
Positive Family History of Hypertension |
107 |
51 |
|
Diabetes Mellitus |
118 |
56.2 |
|
Chronic Kidney Disease |
1 |
0.5 |
|
Ischemic Heart Disease |
2 |
1 |
|
Stroke |
2 |
1 |
|
Fatty liver |
1 |
0.5 |
|
High BP |
2 |
1 |
|
Dyslipidemia |
19 |
9 |
|
Thyroid disease |
3 |
1.4 |
A notable 51% of participants had a positive family history of hypertension, and 56.2% had Diabetes Mellitus. Dyslipidemia was present in 9% of the sample. Other comorbidities like Chronic Kidney Disease, Ischemic Heart Disease, Stroke, Fatty Liver, High Blood Pressure, and Thyroid Disease were relatively rare, each affecting up to 1.4% of participants.
Table V: Association between presence of hypertension and existing comorbidities
|
Risk Factors |
Hypertension (n=68) |
No Hypertension (n=142) |
p-value |
||
|
n |
% |
n |
% |
||
|
Positive Family History |
40 |
58.82% |
67 |
47.18% |
0.14 |
|
Diabetes Mellitus |
57 |
83.82% |
61 |
42.96% |
<0.001 |
|
Chronic Kidney Disease |
1 |
1.47% |
0 |
0.00% |
0.324 |
|
Ischemic Heart Disease |
2 |
2.94% |
0 |
0.00% |
0.04 |
|
Stroke |
0 |
0.00% |
2 |
1.41% |
0.325 |
|
Fatty liver |
0 |
0.00% |
1 |
0.70% |
0.488 |
|
High BP |
0 |
0.00% |
2 |
1.41% |
0.325 |
|
Dyslipidemia |
6 |
8.82% |
13 |
9.15% |
0.938 |
|
Thyroid disease |
0 |
0.00% |
3 |
2.11% |
0.227 |
Diabetes Mellitus shows a significant association with hypertension, with 83.82% of hypertensive participants having diabetes compared to 42.96% in the non-hypertensive group (p-value <0.001). A positive family history of hypertension is more common in the hypertensive group (58.82%) than in the non-hypertensive group (47.18%), although the difference is not statistically significant (p-value 0.14). Ischemic Heart Disease is present in 2.94% of the hypertensive group and absent in the non-hypertensive group, with a significant p-value of 0.04. Other comorbidities like Chronic Kidney Disease, Stroke, Fatty Liver, High Blood Pressure, Dyslipidemia, and Thyroid Disease show no significant association with hypertension, as indicated by p-values greater than 0.05.
4. Discussion
The current retrospective observational study aimed to explore the prevalence of hypertension and its associated risk factors and comorbidities. The study found a hypertension prevalence of 32.38%, which is slightly higher than the national average reported in previous studies [12,13]. This discrepancy could be attributed to the specific outpatient setting, where individuals are more likely to seek medical advice for symptoms related to high blood pressure. In terms of sociodemographic characteristics, the majority of participants were females (59.5%), and the most represented age groups were 50-59 and 40-49 years. This is consistent with global trends indicating that hypertension prevalence increases with age and is often higher among females [8,14,15]. A study conducted in Bangladesh also reported similar findings, where age and BMI were strong predictors for hypertension [16]. The BMI distribution revealed that a large proportion of participants were overweight (39.05%), followed by those with normal weight (32.86%). This is particularly concerning as overweight and obesity are well-established risk factors for hypertension [7,17,18]. A study conducted among university academic staff in Bangladesh also reported a significant association between increased BMI and hypertension [19]. The lipid profile further emphasized the metabolic risk, with 20% of participants having above-normal fasting blood sugar levels and a staggering 60.95% being diabetic. These findings corroborate existing research that metabolic disorders like diabetes often coexist with hypertension, complicating its management and increasing cardiovascular risk [8,20]. The most striking finding was the significant association between hypertension and Diabetes Mellitus (p-value <0.001). A staggering 83.82% of hypertensive participants had diabetes, compared to 42.96% in the non-hypertensive group. This aligns with existing literature that diabetes is a significant risk factor for hypertension [8,21]. Interestingly, Ischemic Heart Disease also showed a significant association with hypertension (p-value 0.04), although the sample size was small.
Limitations of The Study
The study was conducted in a single hospital with a small sample size. So, the results may not represent the whole community. The retrospective design prevented the establishment of causality between risk factors and hypertension. Additionally, the study relied on medical records, which may introduce the possibility of incomplete or inaccurate data.
5. Conclusion
In conclusion, this retrospective observational study reveals a high prevalence of hypertension among patients visiting an outpatient department in Bangladesh, with a rate of 32.38%. The study further underscores the significant association between hypertension and diabetes mellitus, emphasizing the need for an integrated healthcare approach. The findings also highlight the role of various sociodemographic and metabolic risk factors, including age, BMI, and lipid profile, in the prevalence of hypertension. These insights call for targeted interventions and comprehensive healthcare strategies to manage and mitigate the risk factors and comorbidities associated with hypertension in this specific population.
Funding:
No funding sources
Conflict of interest:
None declared
Ethical approval:
The study was approved by the Institutional Ethics Committee
References
- WHO (2017).
- Sarki AM, Nduka CU, Stranges S, Kandala NB, Uthman OA. Prevalence of Hypertension in Low- and Middle-Income Countries. Med 94 (2023): e1959.
- Schutte AE, Srinivasapura Venkateshmurthy N, Mohan S, Prabhakaran D. Hypertension in Low- and Middle-Income Countries. Circ Res 128 (2021): 808-826.
- Lotufo PA, Pereira AC, Vasconcellos PS, Santos IS, Mill JG, et al. Resistant Hypertension: Risk Factors, Subclinical Atherosclerosis, and Comorbidities Among Adults—The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). The Journal of Clinical Hypertension 17 (2023): 74-80.
- Biswas T, Townsend N, Islam MS, Islam MR, Gupta RD, et al. Association between socioeconomic status and prevalence of non-communicable diseases risk factors and comorbidities in Bangladesh: findings from a nationwide cross-sectional survey. BMJ Open 9 (2023): e025538.
- Qin Z, Li C, Qi S, Zhou H, Wu J, et al. Association of socioeconomic status with hypertension prevalence and control in Nanjing: a cross-sectional study. BMC Public Health 22 (2023): 423.
- Rodríguez-Hernández H, Simental-Mendía LE, Rodríguez-Ramírez G, Reyes-Romero MA. Obesity and Inflammation: Epidemiology, Risk Factors, and Markers of Inflammation. Int J Endocrinol 2013 (2023): e678159.
- Zhang H, Wu Y, He Y, Liu X, Liu M, et al. Age-Related Risk Factors and Complications of Patients With COVID-19: A Population-Based Retrospective Study. Front Med 8 (2023).
- Sirmans SM, Pate KA. Epidemiology, diagnosis, and management of polycystic ovary syndrome. CLEP 6 (2023): 1-13.
- Ying-hao P, Yuan-yuan G, Hai-dong Z, Qiu-hua C, Xue-ran G, et al. Clinical characteristics and analysis of risk factors for disease progression of patients with SARS-CoV-2 Omicron variant infection: A retrospective study of 25207 cases in a Fangcang hospital. Front Cell Infect Microbiol 12 (2023).
- Islam MZ, Riaz BK, Islam ANMS, Khanam F, Akhter J, et al. Risk factors associated with morbidity and mortality outcomes of COVID-19 patients on the 28th day of the disease course: a retrospective cohort study in Bangladesh. Epidemiol & Infection 148 (2023): e263.
- Koly KN, Biswas T, Islam A. Increasing Prevalence of Hypertension in Bangladesh: A review. Cardiovasc J 8 (2023): 59-64.
- Rahman MM, Gilmour S, Akter S, Abe SK, Saito E, et al. Prevalence and control of hypertension in Bangladesh: a multilevel analysis of a nationwide population-based survey. J Hypertens 33 (2015): 465-472.
- Hanif AAM, Shamim AA, Hossain MM, Hasan M, Khan MSA, et al. Gender-specific prevalence and associated factors of hypertension among elderly Bangladeshi people: findings from a nationally representative cross-sectional survey. BMJ Open 11 (2023): e038326.
- Khanam R, Ahmed S, Rahman S, Kibria GMA, Syed JRR, et al. Prevalence and factors associated with hypertension among adults in rural Sylhet district of Bangladesh: a cross-sectional study. BMJ Open 9 (2019): e026722.
- Sayeed MA, Banu A, Haq JA, Khanam PA, Mahtab H, et al. Prevalence of hypertension in Bangladesh: effect of socioeconomic risk factor on difference between rural and urban community. Bangladesh Med Res Counc Bull 28 (2002): 7-18.
- Jiang SZ, Lu W, Zong XF, Ruan HY, Liu Y. Obesity and hypertension. Exp Ther Med 12 (2016): 2395-2399.
- Shariq OA, McKenzie TJ. Obesity-related hypertension: a review of pathophysiology, management, and the role of metabolic surgery. Gland Surg 9 (2020): 80-93.
- Ali N, Ahmed S, Mahmood S, Trisha AD, Mahmud F. The prevalence and factors associated with obesity and hypertension in university academic staff: a cross-sectional study in Bangladesh. Sci Rep 13 (2023): 7309.
- Sathi NJ, Islam MA, Ahmed MS, Islam SMS. Prevalence, trends and associated factors of hypertension and diabetes mellitus in Bangladesh: Evidence from BHDS 2011 and 2017-18. PLoS One 17 (2022): e0267243.
- Abu Sayeed M, Banu A, Khan AR, Hussain MZ. Prevalence of diabetes and hypertension in a rural population of Bangladesh. Diabetes Care 18 (1995): 555-558.