Comparison between two Different Doses of Hyperbaric Bupivacaine in Unilateral Spinal Anesthesia among Geriatric Patients in Hemiarthroplasty Surgery
Article Information
Sharmin Ara Begum1, Mohammad Mahabubuzzaman2, Dabasis Kumar3, Mohammad Jahid Iqbal4, Md. Humayun Kabir5, Md. Zubyeer Ali Sheikh6, Md. Shahidullah Humayun Kabir7, Md. Humayun Kabir8, Pooja Bhari9, A. K. M Shahidur Rahman10
1Assistant Professor, Department of Anaesthesiology and Intensive Care Unit ICU), Shaheed Suhrawardy Medical College Hospital, Dhaka, Bangladesh
2Anaesthesiologist, Department of Anaesthesiology and Intensive Care Unit ICU), National Institute of Traumatology and Orthopedics Rehabilitation, Dhaka, Bangladesh
3Assistant Register, Department of Anaesthesiology and Intensive Care Unit ICU), National Institute of Traumatology and Orthopedics Rehabilitation, Dhaka, Bangladesh
4Junior Consultant, Department of Anaesthesiology and Intensive Care Unit (ICU), National Institute of Traumatology and Orthopedics Rehabilitation (NITOR), Dhaka, Bangladesh
5Junior Consultant, Department of Anaesthesiology, Mugda Medical College and Hospital, Dhaka, Bangladesh
6Assistant Professor [Anaesthesiology and Critical Care Medicine (CCM)], Khulna City Medical College Hospital, Khulna, Bangladesh
7Senior Consultant, Department of Anaesthesiology and Intensive Care Unit (ICU), National Institute of Traumatology and Orthopedics Rehabilitation (NITOR), Dhaka, Bangladesh
8Assistant Professor, Department of Anaesthesiology, Rangamati Medical College, Rangamati, Bangladesh
9Clinical Register, Department of Anaesthesiology, Tribhuwan University Teaching Hospital, Kathmandu, Nepal
10Medical Officer, Department of Nephrology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
*Corresponding Author: Dr.Sharmin Ara Begum, Assistant Professor, Department of Anaesthesiology and Intensive Care Unit (ICU), Shaheed Suhrawardy Medical College Hospital, Dhaka, Bangladesh
Received:11 October2023; Accepted: 20 October2023; Published: xxxx2023
Citation:
Begum SA, Mahabubuzzaman M, Kumar D, Iqbal MJ, Kabir MH, Sheikh MZA, Kabir MSH, Kabir MH, Bhari P, Rahman AKMS. Comparison between two Different Doses of Hyperbaric Bupivacaine in Unilateral Spinal Anesthesia among Geriatric Patients in Hemiarthroplasty Surgery. Anesthesia and Critical Care 5 (2023): 44-52
View / Download Pdf Share at FacebookAbstract
Abstract Background: The advantage of unilateral spinal anaesthesia is that it provides a stronger block on the side of surgery, accelerated recovery of the nerve block with better maintenance of cardiovascular stability. Hence it could be a suitable technique for high risk geriatric patients. Objective: To compare two different doses of hyperbaric bupivacaine in unilateral spinal anaesthesia among geriatric patients in hemiarthroplasty surgery. Methods: This randomized controlled clinical trial was conducted in the Department of Anaesthesia and Intensive Care Medicine, National Institute of Traumatology and Orthopaedics Rehabilitation (NITOR), Dhaka, Bangladesh. Total 60 geriatric patients who underwent hemiarthroplasty surgery were enrolled and divided into two groups (30 patients in each group). Group A was received 10 mg hyperbaric bupivacaine plus 20 µg fentanyl and Group B was received 7.50 mg hyperbaric bupivacaine plus 20 µg fentanyl. The time onset of sensory and motor block, level of sensory and degree of motor block and the duration of sensory and motor block were assessed accordingly. Results: No significant difference was found in duration of surgery, onset of sensory and motor block on operative limb between the groups (p >0.05). The haemodynamic parameters were well maintained in group B. The time for 1st demand of analgesia, time of complete sensory and motor recovery was significantly earlier in group B (p <0.05). The higher dose had developed comparatively high peri-operative complications. Conclusion: Unilateral spinal block with a low dose of local anesthetic is safe and effective method for hemiarthroplasty surgery in geriatric patients
Keywords
Block Characteristics; Geriatric Patients; Haemodynamics; Hemiarthroplasty Surgery; Unilateral Spinal Anaesthesia
Block Characteristics articles; Geriatric Patients articles; Haemodynamics articles; Hemiarthroplasty Surgery articles; Unilateral Spinal Anaesthesia articles
Block Characteristics articles Block Characteristics Research articles Block Characteristics review articles Block Characteristics PubMed articles Block Characteristics PubMed Central articles Block Characteristics 2023 articles Block Characteristics 2024 articles Block Characteristics Scopus articles Block Characteristics impact factor journals Block Characteristics Scopus journals Block Characteristics PubMed journals Block Characteristics medical journals Block Characteristics free journals Block Characteristics best journals Block Characteristics top journals Block Characteristics free medical journals Block Characteristics famous journals Block Characteristics Google Scholar indexed journals Geriatric Patients articles Geriatric Patients Research articles Geriatric Patients review articles Geriatric Patients PubMed articles Geriatric Patients PubMed Central articles Geriatric Patients 2023 articles Geriatric Patients 2024 articles Geriatric Patients Scopus articles Geriatric Patients impact factor journals Geriatric Patients Scopus journals Geriatric Patients PubMed journals Geriatric Patients medical journals Geriatric Patients free journals Geriatric Patients best journals Geriatric Patients top journals Geriatric Patients free medical journals Geriatric Patients famous journals Geriatric Patients Google Scholar indexed journals Haemodynamics articles Haemodynamics Research articles Haemodynamics review articles Haemodynamics PubMed articles Haemodynamics PubMed Central articles Haemodynamics 2023 articles Haemodynamics 2024 articles Haemodynamics Scopus articles Haemodynamics impact factor journals Haemodynamics Scopus journals Haemodynamics PubMed journals Haemodynamics medical journals Haemodynamics free journals Haemodynamics best journals Haemodynamics top journals Haemodynamics free medical journals Haemodynamics famous journals Haemodynamics Google Scholar indexed journals Hemiarthroplasty Surgery articles Hemiarthroplasty Surgery Research articles Hemiarthroplasty Surgery review articles Hemiarthroplasty Surgery PubMed articles Hemiarthroplasty Surgery PubMed Central articles Hemiarthroplasty Surgery 2023 articles Hemiarthroplasty Surgery 2024 articles Hemiarthroplasty Surgery Scopus articles Hemiarthroplasty Surgery impact factor journals Hemiarthroplasty Surgery Scopus journals Hemiarthroplasty Surgery PubMed journals Hemiarthroplasty Surgery medical journals Hemiarthroplasty Surgery free journals Hemiarthroplasty Surgery best journals Hemiarthroplasty Surgery top journals Hemiarthroplasty Surgery free medical journals Hemiarthroplasty Surgery famous journals Hemiarthroplasty Surgery Google Scholar indexed journals Unilateral Spinal Anaesthesia articles Unilateral Spinal Anaesthesia Research articles Unilateral Spinal Anaesthesia review articles Unilateral Spinal Anaesthesia PubMed articles Unilateral Spinal Anaesthesia PubMed Central articles Unilateral Spinal Anaesthesia 2023 articles Unilateral Spinal Anaesthesia 2024 articles Unilateral Spinal Anaesthesia Scopus articles Unilateral Spinal Anaesthesia impact factor journals Unilateral Spinal Anaesthesia Scopus journals Unilateral Spinal Anaesthesia PubMed journals Unilateral Spinal Anaesthesia medical journals Unilateral Spinal Anaesthesia free journals Unilateral Spinal Anaesthesia best journals Unilateral Spinal Anaesthesia top journals Unilateral Spinal Anaesthesia free medical journals Unilateral Spinal Anaesthesia famous journals Unilateral Spinal Anaesthesia Google Scholar indexed journals anaesthesia articles anaesthesia Research articles anaesthesia review articles anaesthesia PubMed articles anaesthesia PubMed Central articles anaesthesia 2023 articles anaesthesia 2024 articles anaesthesia Scopus articles anaesthesia impact factor journals anaesthesia Scopus journals anaesthesia PubMed journals anaesthesia medical journals anaesthesia free journals anaesthesia best journals anaesthesia top journals anaesthesia free medical journals anaesthesia famous journals anaesthesia Google Scholar indexed journals National Institute of Traumatology and Orthopaedics Rehabilitation articles National Institute of Traumatology and Orthopaedics Rehabilitation Research articles National Institute of Traumatology and Orthopaedics Rehabilitation review articles National Institute of Traumatology and Orthopaedics Rehabilitation PubMed articles National Institute of Traumatology and Orthopaedics Rehabilitation PubMed Central articles National Institute of Traumatology and Orthopaedics Rehabilitation 2023 articles National Institute of Traumatology and Orthopaedics Rehabilitation 2024 articles National Institute of Traumatology and Orthopaedics Rehabilitation Scopus articles National Institute of Traumatology and Orthopaedics Rehabilitation impact factor journals National Institute of Traumatology and Orthopaedics Rehabilitation Scopus journals National Institute of Traumatology and Orthopaedics Rehabilitation PubMed journals National Institute of Traumatology and Orthopaedics Rehabilitation medical journals National Institute of Traumatology and Orthopaedics Rehabilitation free journals National Institute of Traumatology and Orthopaedics Rehabilitation best journals National Institute of Traumatology and Orthopaedics Rehabilitation top journals National Institute of Traumatology and Orthopaedics Rehabilitation free medical journals National Institute of Traumatology and Orthopaedics Rehabilitation famous journals National Institute of Traumatology and Orthopaedics Rehabilitation Google Scholar indexed journals general anaesthesia articles general anaesthesia Research articles general anaesthesia review articles general anaesthesia PubMed articles general anaesthesia PubMed Central articles general anaesthesia 2023 articles general anaesthesia 2024 articles general anaesthesia Scopus articles general anaesthesia impact factor journals general anaesthesia Scopus journals general anaesthesia PubMed journals general anaesthesia medical journals general anaesthesia free journals general anaesthesia best journals general anaesthesia top journals general anaesthesia free medical journals general anaesthesia famous journals general anaesthesia Google Scholar indexed journals spinal anaesthesia articles spinal anaesthesia Research articles spinal anaesthesia review articles spinal anaesthesia PubMed articles spinal anaesthesia PubMed Central articles spinal anaesthesia 2023 articles spinal anaesthesia 2024 articles spinal anaesthesia Scopus articles spinal anaesthesia impact factor journals spinal anaesthesia Scopus journals spinal anaesthesia PubMed journals spinal anaesthesia medical journals spinal anaesthesia free journals spinal anaesthesia best journals spinal anaesthesia top journals spinal anaesthesia free medical journals spinal anaesthesia famous journals spinal anaesthesia Google Scholar indexed journals postoperative analgesia articles postoperative analgesia Research articles postoperative analgesia review articles postoperative analgesia PubMed articles postoperative analgesia PubMed Central articles postoperative analgesia 2023 articles postoperative analgesia 2024 articles postoperative analgesia Scopus articles postoperative analgesia impact factor journals postoperative analgesia Scopus journals postoperative analgesia PubMed journals postoperative analgesia medical journals postoperative analgesia free journals postoperative analgesia best journals postoperative analgesia top journals postoperative analgesia free medical journals postoperative analgesia famous journals postoperative analgesia Google Scholar indexed journals
Article Details
- Introduction
Hemiarthroplasty due to neck of the femur fracture is a common procedure in the advanced age groups [1, 2]. The patients of geriatric age groups may have various comorbidies like- cardiac, endocrine, renal, cerebral, and respiratory tract diseases [1, 2]. Anaesthesia approach for these patients generally includes general anaesthesia (GA), conventional subarachnoid block (SAB), and epidural anaesthesia etc. Regional anaesthesia is preferred over general anaesthesia for lower limb orthopaedic surgeries and spinal anaesthesia (SA) is often a choice [3]. Spinal anaesthesia is a simple and quick technique that provides intense and reliable block, although it has risk of limited duration of action [3,]. Spinal anesthesia is a frequently applied technique with its ease of performance and high success rate in lower limb orthopedic surgeries [3-6]. However, side effects such as hypotension, bradycardia, nausea and vomiting, post puncture headache and urine retention are frequently observed in spinal anesthesia [7, 8]. Compared to conventional spinal anaesthesia, unilateral spinal anaesthesia provides denser and longer lasting block with less incidence of hypotension [4, 5]. Unilateral spinal anaesthesia is confined to one side of the body by the subarachnoid administration of hypobaric or hyperbaric solutions with the patient placed in the lateral position [9, 10]. In 1961, Tanasichuk MA et al. described a particular technique of spinal anaesthesia in patients receiving one limb orthopaedic surgery, which they named spinal hemianalgesia [11]. In practice, a conventional unilateral spinal anaesthesia technique can only result in motor block and sensory block preferential to one side [4, 5]. During recent years unilateral spinal anesthesia has been used successfully in lower limb surgeries [12-18]. It is particularly advantageous in high risk patients such as patients with ischemic heart disease (IHD), congenital cardiac diseases, pulmonary diseases and diabetes mellitus,where it produces less haemodynamic changes [12]. It has many advantages over conventional spinal anaesthesia such as lower incidence of hypotension, faster recovery and increased patient satisfaction [12, 13]. In conventional spinal anaesthesia it is not possible to limit the accompanied sympathetic block that normally exceeds the sensory block by 2-6 segments [13]. In lower limb surgery, unilateral spinal anaesthesia with less sympathetic block may be advantageous as it provides adequate analgesia and anaesthesia during orthopaedic procedures and reduces risks in comparison with conventional spinal anaesthesia [12-14]. The primary goal of the unilateral spinal anaesthesia is to only allow the particular nerve block at the surgical site [12-16]. In a lateral decubitus position; the concentration, volume and dose of local anesthetic solution that injected into the subarachnoid space may be strictly related to obtaining a concentration gradient between the dependent side and the nondependent side [17]. Therefore an optimal unilateral block can be achieved with small or reduced doses of hyperbaric or hypobaric local anesthetics [18-20]. The doses using in local anesthetics are also important factor for local anesthetic [18-20]. When considering nerve fibers as a compartment, a relative or absolute surplus of a local anesthetic is not completely fixed; if the patient’s position changes over longer periods of time, the free local anesthetics can be redistributed [21, 22]. However, bupivacaine might delay the recovery of motor functions and cause urinary retention, leading to delayed discharge of the patient [18-20]. For this reason, small doses of bupivacaine used to produce optimum unilateral spinal anesthesia become more popular day by day [18-20]. Baricity, drug volume, patient positioning, needle type, bevel direction and injection speed are some important factors that can affect the success of unilateral subarachnoid block [15, 16]. Unilateral spinal anaesthesia is preferable to bilateral spinal anaesthesia because it provides a stronger block on the surgical side and speeds up the block recovery with lower incidence of hypotension and better maintenance of cardiovascular stability [12, 13]. Hence unilateral spinal anaesthesia can be a reliable technique for high risk patients such as geriatrics patients [16]. In this background, the current study was aimed to compare the efficacy and safety of unilateral spinal anesthesia by using different doses of hyperbaric bupivacaine in geriatric patients underwent unilateral hemiarthroplasty surgery.
2. Methods
This prospective study was conducted at Department of Anaesthesia and Intensive Care Medicine, National Institute of Traumatology and Orthopedics Rehabilitation (NITOR), Dhaka, Bangladesh. A total of sixty (60) geriatric patients scheduled for unilateral hemiarthroplasty surgery were enrolled. Informed written consent was obtained from all study patients prior to enrolment. Inclusion criteria were; American Society of Anesthesiologists (ASA) score II-III, age more than 65 years of both gender. Exclusion criteria were contraindications for spinal anesthesia: skin infection at the site of regional anesthesia, patients with coagulopathies, taking anticoagulant drugs, patients having allergy to local anesthetic drugs, patients with hypo-volumia, neurologic and psychiatric disorder, spine deformity, body mass index (BMI) >35 kg/m2 and patients on chronic pain treatment.
2.1 Study population
Total sixty (60) geriatric patients (age >65 years) scheduled for unilateral hemiarthroplasty were included. Then patients were randomly allocated into two groups (group A and group B); allowing 30 patients in each group. All study patients were received unilateral spinal anesthesia in lateral position on operative side with different doses and volume of bupivacaine with fentanyl. In group A, patients were received unilateral spinal anesthesia with 10 mg (2 ml) hyperbaric bupivacaine plus 20 µg fentanyl; in group B, patients received 7.5 mg (1.5 ml) hyperbaric bupivacaine plus 20 µg fentanyl in spinal anaesthesia.
2.2 Study procedure
On arrival in operation theatre all patients were introduce an intravenous cannula (18 gauge) on contralateral forearm of the operative limb. Then patients were given intravenous infusion of 10 ml/kg of lactate Ringer solution Standard monitoring technique was used such as- non-invasive blood pressure detector, electrocardiogram, peripheral pulse oximetry etc. Arterial blood pressure (ABP) and heart rate (HR) of the patients were recorded at the end of pre-load, before inducing spinal block. All patients were placed in a lateral position on the operative side down, but the vertebral column was positioned as horizontally as possible. Under complete aseptic technique, dural puncture was performed using a midline approach at the lumber 3-4 (L3-L4) inter-space with a 25 gauge spinal Quincke needle. Both groups were received an intra-thecal injection of 0.5% bupivacaine heavy over a period of 1 ml/minute and without further aspiration maneuvers. The patients were kept in the lateral position for 10 minutes and then placed in the supine position for surgery (unilateral low dose spinal anesthesia). Hemodynamic changes were recorded every 5 minutes after spinal anesthesia, and then until the end of surgery. Hypotension [systolic blood pressure (SBP) <90 mm of Hg or 30% decrease from the baseline) were treated with additional intravenous bolus of 15 ml/kg (crystalloid solution). However, if supplementation of fluid was failed to reverse hypotension, intravenous ephedrine 5-10 mg bolus was administrated. Bradycardia [heart rate (HR) < 50 bpm] was treated with 0.2 mg of atropine intravenously as necessary. The sensory anesthesia level was evaluated by pinprick method with 22 gauge hypodermic needle along the anterior middle clavicular line of both sides. The time onset of analgesia was defined as the time onset of sensory block to maximum cephalad spread. The spreading of sensory block according to dermatomes was assessed by pinprick method up to 10 minutes after unilateral spinal anaesthesia on both side of limb. Time require for the highest level of dermatome [that is thoracic 10 (T10) level] was recorded in minutes. The onset and degree of motor block was evaluated using modified Bromage scale (0= no motor block, 1= hip blocked, 2= hip and knee blocked, 3= complete motor block). Pain was assessed from the beginning of surgery using a 10 cm visual analog scale (VAS). If the patient failed to achieve sensory block up to dermatomes level of thoracic 12 (T12) within 10 minutes after SAB, then it was considered as block failure and was excluded from this study. We also recorded side effects like- nausea, vomiting and headache. The urinary retention was recorded if the patient was unable to void spontaneously during postoperative period. Then appropriate size of bi channel Folley’s catheter was placed in urinary tract and was keep in situ.
2.3 Postoperative Analgesia
The same protocol was applied for postoperative analgesia in both groups. The postoperative pain was assessed by VAS scale. When the patient complain moderate to severe pain or the VAS score ≥4 was observed during the postoperative periods; then the increment dose of morphine was followed as 2 mg morphine IV bolus then reassessed VAS after 3 to 5 minutes, then repeat incremental dose 1 mg IV until the pain was subsided. Total amount of morphine required (mg) for pain controlled was recorded accordingly.
2.4 Statistical analysis
Statistical analysis was performed by using a windows based statistical software program Statistical Package for Social Sciences (SPSS) version- 26. All continuous variables were expressed as mean with standard deviation (mean ± SD) and all categorical variables were expressed as number (n) with percentage (%). Comparisons of normally distributed variables were performed by Student “t” test and Chi-squared (c2) testas appropriate. The p value <0.05 was accepted as a level of significance.
2.5 Ethical review committee (ERC) clearance
This study was approved by ethical review committee (ERC), National Institute of Traumatology and Orthopedics Rehabilitation (NITOR), Dhaka, Bangladesh [ERC clearance Memo No. MEU-NITOR/Academy/2022/468; date 08/02/2022].
3. Results
This study intended to compare the efficacy and safety of unilateral spinal anesthesia by using different doses of hyperbaric bupivacaine in geriatric patients underwent unilateral hemiarthroplasty surgery. Total 60 geriatric patients (age >65 years) were received unilateral subarachnoid block (SAB) with different doses of hyperbaric bupivacaine in two equally divided groups, where each group had 30 patients. It was observed that the mean age of study patients was 76.6±8.9 years in group A and that was 77.8±9.5 years in group B with majority belonged to 65-85 years. Maximum patients had ASA Class II in both groups (60 % versus 66.7%), as the patients were taken with elderly age. No significant difference was found in basic characteristics of study patients among the groups (p>0.05) (Table- 1).
Table- 1:Basic characteristics of the study patients (N= 60)
|
Basic characteristics |
Group A |
Group B |
p value |
|
|
Age (years) |
Range |
(n= 30) |
(n= 30) |
|
|
65-75 years |
10 (33.3%) |
9(30%) |
||
|
76-85 years |
11 (36.7%) |
12(40 %.) |
||
|
86-95 years |
6(20%) |
5 (16.7%) |
||
|
>96 year |
3 (10%) |
4(13.3%) |
||
|
Mean±SD |
76.6±8.9 |
77.8±9.5 |
*0.493ns |
|
|
Gender |
Male |
13 (43.3%) |
14 (46.7%) |
**0.795ns |
|
Female |
17 (56.7%) |
16(53.3%) |
||
|
ASA class |
Class II |
18 (60%) |
20 (66.7%) |
**0.592ns |
|
Class III |
12 (40%) |
10(33.3%) |
||
|
Duration of surgery (minutes) |
72.4±11.2 |
74.1±12.6 |
*0.362ns |
|
Values were expressed as Mean±SD, frequency with percentage, *Student “t” test, **Chi-squared(c2)test, ns= not significant
Considering the onset of sensory and motor block of the operative limb between two groups; the time onset of sensory block (minutes) between the groups (2.3±0.7 minutes versus 2.8±0.8 minutes) and the time onset of motor block (minutes) between the groups (3.9±1.2 minutes versus 4.5±1.4 minutes) were not significantly different between the groups (p>0.05) (Table- 2).
Table- 2: Comparison of time onset of sensory and motor block on operative limb between the groups (N= 60)
|
Operative limb |
Group A (n= 30) |
Group B (n= 30) |
p value* |
|
Onset time of complete sensory blockade (minutes) (≥T12) |
2.3±0.7 |
2.8±0.8 |
0.616ns |
|
Onset time of complete motor blockade (minutes) (Bromage score ≥3) |
3.9±1.2 |
4.5±1.4 |
0.371ns |
Values were expressed as Mean±SD, *Student “t” test, ns= not significant
On the other hand the time onset of sensory block on non-operating limb was significantly low in group A (3.7±1.4 minutes versus 5.6±1.8 minutes, p= 0.026). Similarly the time onset of motor block on non-operating limb was significantly low in group A (5.3±1.9 minutes versus 7.8±2.3 minutes, p= 0.021). Therefore, it was found that the patients receiving lower dose of bupivacaine with fentanyl had late onset of both sensory and motor block on non-operative limb (Table- 3).
Table- 3: Comparison of time onset of sensory and motor block on non-operative limb between the groups (N= 60)
|
Non-operative limb |
Group A |
Group B |
p value* |
|
(n= 30) |
(n= 30) |
||
|
Onset time of complete sensory blockade (minutes) (≥T12) |
3.7±1.4 |
5.6±1.8 |
0.026ss |
|
Onset time of complete motor blockade (minutes) ( Bromage score ≥3) |
5.3±1.9 |
7.8±2.3 |
0.021ss |
Values were expressed as Mean±SD, *Student “t” test, ss= statistically significant
When considered level of sensory block between two groups on operative limb: 16.7% patients of group A and 6.7% patients of group B was achieved at the dermatome level of thoracic 6 (T6). While sensory block of the dermatome level of T8 was considered, it was observed that 53.3% patients of group A and 23.3% patients of group B was achieved so. All patients (100%) of group A was achieved sensory block at the dermatome level of T10, but 76.7% patients of group B was achieved sensory block at the dermatome level of T10. Our targeted sensory block level on operative limb was the dermatome level of T12 for hemiarthroplasty surgery. All patients with successful SAB of the both groups in this study were achieved the sensory block at dermatome level of T12 and L1 (Table- 4).
Table- 4: Level of sensory block on operative limb between two groups (N= 60)
|
Dermatome levels |
Group A (n= 30) |
Group B (n= 30) |
|
T6 |
5(16.7%) |
2(6.7%) |
|
T8 |
16(53.3%) |
7(23.3%) |
|
T10 |
30(100%) |
23(76.7%) |
|
T12 |
30(100%) |
30(100%) |
|
L1 |
30(100%) |
30(100%) |
Considering the level of sensory block on non-operative limb: all patients (100%) of both groups were achieved sensory block at the dermatome level of L1. But, 86.7% patients of group A and 73.3% patients of group B had achieved sensory block at the dermatome level of T12 on non-operative limb. The achievement of sensory block at the dermatome level of T10 was 73.3% in group A and 43.3% in group B. Again 36.7% patients of group A and 10% patients of group B had sensory block at dermatome level of T8. None of the patient in group B had sensory block at dermatome level of T6 but 10 % patients in group A had sensory block at dermatome level of T6 on non-operative limb. The reasons of these distribution were due to we kept the patients in lateral position on operative limb, that might prevent cephalad spread of lower dose of bupivacaine on non-operative limb (Table- 5).
Table- 5: Level of sensory block on non-operative limb between two groups (N= 60)
|
Dermatome levels |
Group A (n= 30) |
Group B (n= 30) |
|
|
|
|
|
T6 |
3(10%) |
0(00.0%) |
|
T8 |
11(36.7%) |
3(10%) |
|
T10 |
22(73.3%) |
13(43.3%) |
|
T12 |
26(86.7%) |
22(73.3%) |
|
L1 |
30(100%) |
30(100%) |
The heart rate (HR) was well maintained in both groups up to 15 minutes during intra-operative period. Then reduction of HR was observed in both groups. The HR was lower in group A then that of group B up to 60 minutes during intra-operative period. That was statistically significant as p value were <0.05 at these time interval. Student t-test was performed to compare mean HR at these time interval. After 60 minutes, HR of the both groups were raised and then no significant difference was observed between the groups (p >0.05) (Figure-1).
Values are expressed as Mean±SD.* statistically significant.
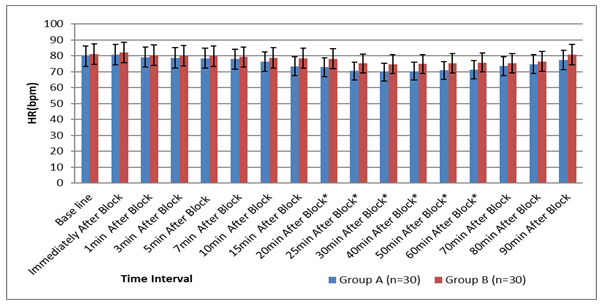
Figure 1: Heart Rate (bpm) of the patients during intra-operative period (N=60)
Regarding the mean arterial pressure (MAP); there had been a significant difference at 15th minute to 50th minute after SAB block during intra-operative period (p<0.05). The group A had lower MAP than that of group B at that period. Rest of the points of time the mean arterial pressure (MAP) difference was not statistically significant between the groups (p>0.05). That might be due to late onset of sympathetic block as the patients were kept lateral position for 10 minutes after administration of SAB (Table- 6).
Table- 6: Comparison of the mean arterial pressure (MAP) at different point of time during intra-operative period between two groups (N= 60)
|
MAP (mmHg) |
Group A |
Group B |
p value* |
|
(n= 30) |
(n= 30) |
||
|
Base line |
102.3±7.6 |
104.7±7.7 |
0.617 |
|
1 minute after block |
101.3±6.9 |
103.6±6.8 |
0.434 |
|
5 minutes after block |
96.6±5.3 |
98.3±5.8 |
0.379 |
|
10 minutes after block |
94.5±5.1 |
97.6±5.3 |
0.328 |
|
15 minutes after block |
91.7±5.6 |
96.8±5.4 |
0.007s |
|
20 minutes after block |
90.8±5.3 |
96.9±4.9 |
0.009s |
|
25 minutes after block |
91.2±5.5 |
97.3±4.8 |
0.007s |
|
30 minutes after block |
90.6±5.7 |
97.2±4.7 |
0.005s |
|
40 minutesafter block |
91.7±5.8 |
99.1±5.1 |
0.006s |
|
50 minutes after block |
94.2±6.3 |
99.7±5.6 |
0.011s |
|
60 minutes after block |
95.8±6.7 |
100.2±5.9 |
0.247 |
|
70 minutes after block |
98.7±6.5 |
102.5±6.2 |
0.365 |
|
80 minutesafter block |
100.5±6.8 |
103.2±6.7 |
0.387 |
|
90 minutes after block |
101.8±7.4 |
103.8±7.8 |
0.439 |
Values are expressed as Mean±SD,.*Student “t” test, s= statistically significant
In this study post-operative pain was treated according to operational definition. If pain not alleviated and VAS pain score ≥4, rescue medication was given as incremental until the pain was subsided (that was VAS score <4). Here injection morphine was used as rescue medication. Intravenous (IV) incremental dose of morphine 3 mg was given until the VAS pain score was <4 or pain was subsided. The time for 1st demand of analgesic was considered as patients requested for analgesia or VAS ≥4 post-operatively, which was significantly earlier in group B (97.1±5.2 minutes versus 125.5±10.3 minutes, p< 0.05). Similarly the time to complete recovery from the sensory block was significantly earlier in group B (123.7±15.4 minutes versus 154.3±18.6 minutes, p< 0.05). The time to complete recovery from the motor block was also significantly less in group B than group A (108.±8.5 minutes versus 137.2±13.7 minutes, p< 0.05). Therefore, lower dose of bupivacaine with fentanyl had earlier time for 1st demand of analgesia with less duration of both sensory and motor block (Table- 7).
Table- 7: Distribution of the study patients according to duration of analgesia and duration of motor block (N= 60)
|
Variable |
Group A |
Group B |
p value* |
|
(n= 30) |
(n= 30) |
||
|
The time for 1stdemand of analgesia (minutes) |
125.5±10.3 |
97.1±5.2 |
0.007s |
|
Time to complete recovery from the sensory block (minutes) |
154.3±18.6 |
123.7±15.4 |
0.002s |
|
Time to complete recovery from the motor block (minutes) |
137.2±13.7 |
108.±8.5 |
0.005s |
Values are expressed as Mean±SD., *Student “t” test, s= statistically significant
It was observed that, patients received SAB with higher dose of bupivacaine with fentanyl had developed high peri-operative complications like- hypotension (36.7% versus 16.7%), bradycardia (23.3% versus 10%), shivering (20% versus 6.7%) and itching (30% versus 26.7%) compared to lower dose of bupivacaine with fentanyl. That might be due to sudden effects of sympathetic block and cephalad spread of SAB during intra-operative period (Table- 8).
Table- 8: Complications of the patient’s during peri-operative periods. (N= 60)
|
Complications* |
Group A |
Group B |
p value* |
|
(n= 30) |
(n= 30) |
||
|
Hypertension |
4 (13.3%) |
6 (20%) |
0.488ns |
|
Hypotension |
11 (36.7%) |
5 (16.7%) |
0.079ns |
|
Bradycardia |
7 (23.3%) |
3 (10%) |
0.166ns |
|
Shivering |
6(20%) |
2(6.7%) |
0.278ns |
|
Itching |
9 (30%) |
8 (26.7%) |
0.775ns |
*Multiple responses, values were expressed as frequency and percentage, *Chi-squared (c2) test, ns= not significant
4. Discussion
The main objectives of unilateral spinal anesthesia are to provide analgesia and motor block in only operative site; it enhanced patient comfort and satisfaction, and it also prevents hemodynamic changes. Several factors are associated with undesirable results of unilateral spinal anesthesia including- patient position during the subarachnoid puncture, the length of time in the lateral position, the injection speed, the dose of the local anesthetic and the density of the solution used in relation to the cerebrospinal fluid (CSF) [9]. This current study comparing different doses of 0.5% hyperbaric bupivacaine that were used in geriatric patients who were underwent hemiarthroplasty surgery. A total 60 geriatric patients were equally divided into two groups: group A (30 patients) patients were received unilateral spinal anesthesia with 10 mg hyperbaric bupivacaine plus 20 µg fentanyl; group B (30 patients) patients were received 7.5 mg hyperbaric bupivacaine plus 20 µg fentanyl in spinal anaesthesia. The mean age of the study patients was 76.6±8.9 years in group A and 77.8±9.5 years in group B with majority were in 65-85 years.
The desired dermatome level of sensory block (T10 in unilateral spinal anesthesia) was obtained on operative limb that was 100% of patients in group A and 76.7% in group B. While sensory block of the dermatome level of T8 was considered, it was observed that 53.3% patients of group A and 23.3% patients of group B was achieved on the operative limb. Considering the level of sensory block (T10) on non-operative limb; 70% in group A and 43.3% in group B were achieved at that level. In accordance 36.7% patients of group A and 10% patients of group B had sensory block at dermatome level of T8. None of the patient of group B had sensory block at dermatome level of T6 but 10% patients of group A had sensory block at dermatome level of T6. We targeted sensory block at the dermatome level of T12 for hemiarthroplasty surgery on operative limb. In a previous study Zhu L, et al.observed dermatome level of sensory block was maximal level on the operative side, which was significantly higher (T9; ranged T10-T7) in comparison with those on the non-operative side (S2; rang, S2-L5) [17]. But the maximal level of sensory block on the operative side was similar to that of the non-operative side in control group (T8; ranged T10- T5) [17]. Thus, they observed no significant differences in the maximal level of sensory block between two groups on the operative sides [17]. Although in this current study a significant difference in the maximal levels of sensory block was observed between two groups on the operative limb. The previous study had dissimilarity with our study as we observed a difference with dermatomal distribution. In non-operative limb; the achievement of sensory block at dermatome level of T10 was 73.3% in group A and 43.3% in group B. While 36.7% patients of group A and 10% patients of group B had sensory block at dermatome level of T8. None of the patient of group B had sensory block at dermatome level of T6 but 10 % patients in group A had sensory block at dermatome level of T6. The reason of this distribution could be due to we kept the patients in lateral position on operative limb. That might prevent cephalad spread of lower dose of bupivacaine on non-operative limb. In this context Singh TK, et al. found that sensory levels were much higher and motor block was denser in operative limb in relation to non-operative limb [18]. They observed, unilateral spinal anesthesia was achieved in 73% patients in one group and in 75% patients of other group [18]. A successful unilateral spinal block by using hyperbaric bupivacaine was ranging between 73%-86% has been reported [19, 20]. This is due to higher anesthetic concentration achieved near the nerve roots of operative limb. When the patients were turned supine, unilateral anaesthesia decreased to 65%, and 70% in groups respectively [18]. This can be explained due to diffusion of free local anesthetic on attaining supine position [18-20]. But this portion of drug is too small to block nerve roots to a clinically significant level. In above studies, there was significant difference in spread of anesthesia between operative and contra-lateral limb [18-20]. The finding of current study was matched with related previous studies [18-20]. In this study reduction of heart rate (HR) was observed in both groups during intra-operative period. But the HR was lower in group A than that of group B up to 60 minutes during intra-operative period. That was statistically significant (p<0.05) at these time interval. The mean HR of the both group was raised after 60 minutes during intra-operative period. In accordance, Kocman BI et al. also noted that HR was reduced in both study group and control group during intra-operative period; as they compared unilateral and bilateral spinal anesthesia with hyperbaric bupivacaine 7.5 mg plus fentanyl 25 mcg in inguinal hernia repair [21]. Hembrador S and fellows showed that intra-thecal fentanyl has been associated with bradycardia, and the rate may be higher at doses of 25 mcg and above [22]. That was because of intra-thecal fentanyl might produce bradycardia [22]. In another study Ali L and colleagues observed post SAB heart rate (HR) and mean arterial pressure (MAP) at regular intervals and lowest value was recorded at different times during surgery [23]. Difference of lowest mean arterial pressure from pre-SAB value was calculated as percentage and the average fall of percentages in mean arterial pressure (MAP) from pre-SAB values was 20%-59%; they also observed the maximum decrease in HR was seen at 20 minutes after giving spinal anesthesia [23]. These findings were comparable with our findings. In this current study the time for 1st demand of analgesia was significantly earlier in group B than group A (97.1±5.2 minutes versus 125.5±10.3 minutes) (p <0.05). The time of complete recovery from the sensory block was quicker in group B (123.7±15.4 minutes) than that of group A (154.3±18.6 minutes). The time of complete recovery from the motor block was also less in group B than group A (108.±8.5 minutes versus 137.2±13.7 minutes). These differences were statistically significant (p< 0.05). Therefore, lower dose of bupivacaine with fentanyl had significant earlier time for 1st demand of analgesia with a significant less duration of both sensory and motor block. These results were supported by a couple of similar previous studies [24-28]. In this current study, patients received SAB with higher dose of bupivacaine (10 mg) with fentanyl had developed comparatively more peri-operative complication like- hypotension (36.7%), bradycardia (23.3%) and shivering (20%) compared to lower dose of bupivacaine (7.5 mg) with fentanyl. That might be due to sudden effects of sympathetic block and cephalad spread of SAB during intra-operative period. In this context one related study found that, there was no bradycardia in the unilateral group; but in the bilateral group, 5 patients had bradycardia, 6 patients had hypotension and 8 patients had nausea during peri-operative period, that was statistically significant between the groups (p<0.05) [16]. Ali L et al. observed that hypotension occurred in 15(75%) patients, bradycardia in 12(60%) patients, tachycardia in 3(15%) patients and nausea occurred in 5(25%) patients in unilateral spinal anesthesia for major lower limb surgery among patients with cardiac failure [23]. These findings were consistent with our study.The current study demonstrated that, attempting unilateral spinal block with low dose of bupivacaine (7.5 mg) in geriatric patients underwent hemiarthroplasty surgery was resulted in more intense motor block but early regression of sensory level on the operated side, with more stable haemodynamic parameters then unilateral spinal anesthesia with higher dose (10 mg) of bupivacaine. The quality of sensory and motor block during surgery was almost similar in two different doses. But low dose provides fewer side effects in geriatric patients.
5. Conclusion
Unilateral spinal anesthesia with a low dose of bupivacaine, limited volume technique induces sufficient sensory and motor block with an appropriate level of analgesia, better haemodynamic stability and fewer side effects. Therefore, unilateral spinal block with a low dose of local anesthetic is safe and effective method for hemiarthroplasty surgery in geriatric patients.
Limitation
It was a single centre study with a relatively small sample size. Moreover, this study was conducted only among the geriatric patients with ASA class- II and class- III.
Conflicts of interest
All authors declared that they have no conflicts of interest regarding this publication.
References
- Tsui BC, Wagner A, Finucane B. Regional anaesthesia in the elderly: a clinical guide. Drugs & aging. 21 (2004):895-910.
- Peters CL, Shirley B, Erickson J. The effect of a new multimodal perioperative anesthetic regimen on postoperative pain, side effects, rehabilitation, and length of hospital stay after total joint arthroplasty. The Journal of arthroplasty. 21(2006):132-138.
- Neuman MD, Silber JH, Elkassabany NM, et al. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. The Journal of the American Society of Anesthesiologists. 117(2012):72-92.
- Buettner B, Mansur A, Bauer M, et al. Unilateral spinal anesthesia: Literature review and recommendations. Der Anaesthesist. 65 (2016):847-865.
- Karpel E, Marszo?ek P, Pawlak B, et al. Effectiveness and safety of unilateral spinal anaesthesia. AnestezjolIntens Ter. 41 (2009):33-36.
- Rodgers A, Walker N, Schug S, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. Bmj. 321(2000):1493.
- Carpenter RL, Caplan RA, Brown DL, et al. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology. 76(1992):906-916.
- Jonnesco T. Remarks on general spinal analgesia. British medical journal.2(1909):1396.
- Brown S. Fractional segmental spinal anesthesia in poor risk surgical patients: report of 600 cases. The Journal of the American Society of Anesthesiologists. 13 (1952):416-428.
- Harder HJ. Unilateral lumbar spinal anesthesia with hyperbaric solutions. Der Anaesthesist. 8(1959):145-146.
- TANASICHUK MA, SCHULTZ EA, MATTHEWS JH, et al. Spinal hemianalgesia: an evaluation of a method, its applicability, and influence on the incidence of hypotension. The Journal of the American Society of Anesthesiologists. 22 (1961):74-85.
- Chohan U, Afshan G, Hoda MQ, et al. Haemodynamic effects of unilateral spinal anesthesia in high risk patients. JPMA. The Journal of the Pakistan Medical Association. 52(2002):66-69.
- Imbelloni LE, Beato L, Cordeiro JA. Unilateral spinal anesthesia with low 0.5% hyperbaric bupivacaine dose. Revistabrasileira de anestesiologia. 54 (2004):700-706.
- Kim KC, Moneta MD. Unilateral spinal anesthesia can be obtained with low dose bupivacaine. Anesthesiology. 77(1992):A803.
- Gouveia M. Spinal Hemianesthesia: Unilateral and Posterior. Austin J Anesthesia and Analgesia. 1 (2014):1003.
- Tekye SM, Alipour M. Comparison of the effects and complications of unilateral spinal anesthesia versus standard spinal anesthesia in lower-limb orthopedic surgery. RevistaBrasileira de Anestesiologia.64 (2014):173-176.
- Zhu L, Tian C, Li M, et al. The stress response and anesthetic potency of unilateral spinal anesthesia for total Hip Replacement in geriatric patients. Pakistan Journal of Pharmaceutical Sciences. 2 (2014):27.
- Singh TK, Anabarsan A, Srivastava U, et al. Unilateral spinal anaesthesia for lower limb orthopaedic surgery using low dose bupivacaine with fentanyl or clonidine: A randomised control study. Anesthesia & Clinical Research. 5(2014):1-5.
- Casati A, Fanelli G, Cappelleri G, et al. Low dose hyperbaric bupivacaine for unilateral spinal anaesthesia. Canadian journal of anaesthesia. 45 (1998):850-854.
- Kaya M, O?uz S, Aslan K, et al. A low-dose bupivacaine: a comparison of hyperbaric and hypobaric solutions for unilateral spinal anesthesia. Regional Anesthesia & Pain Medicine. 29(2004):17-22.
- Kocman BI, Krobot R, Premuzic J, et al. Comparison of unilateral and bilateral spinal anesthesia with hyperbaric bupivacaine 7.5 mg+ fentanyl 25μg for inguinal hernia repair: 8AP2–6. European Journal of Anaesthesiology| EJA. 27(2010):131.
- Hembrador S, Delgado C, Dinges E, et al. Lower, variable intr-athecal opioid doses, and the incidence of prolonged fetal heart rate decelerations after combined spinal epidural analgesia for labor: A quality improvement analysis. Romanian Journal of Anaesthesia and Intensive Care. 27(2020):27.
- Ali L, Ali M, Ali U, et al. Unilateral Spinal Anesthesia for Major Lower Limb Surgery in Patients with Cardiac Failure. Pakistan Armed Forces Medical Journal. 1(2016).
- Atef HM, El-Kasaby AM, Omera MA, et al. Optimal dose of hyperbaric bupivacaine 0.5% for unilateral spinal anesthesia during diagnostic knee arthroscopy. Local and regional anesthesia. (2010):85-91.
- Valanne JV, Korhonen AM, Jokela RM, et al. Selective spinal anesthesia: a comparison of hyperbaric bupivacaine 4 mg versus 6 mg for outpatient knee arthroscopy. Anesthesia & Analgesia. 93 (2001):1377-1379.
- Borghi B, Stagni F, Bugamelli S, et al. Unilateral spinal block for outpatient knee arthroscopy: a dose-finding study. Journal of clinical anesthesia. 15 (2003):351-356.
- Kuusniemi KS, Pihlajamäki KK, Pitkänen MT. A low dose of plain or hyperbaric bupivacaine for unilateral spinal anesthesia. Regional Anesthesia & Pain Medicine. 25(2000):605-610.
- Esmaoglu A, Boyaci A, Ersoy Ö, et al. Unilateral spinal anaesthesia with hyperbaric bupivacaine. Actaanaesthesiologicascandinavica. 42(1998):1083-1087.
