Comparative Study of Automated End Tidal Control Versus Manual Fresh Gas Flow Adjustment with Respect to Gas Usage and Delivery during Low Flow Anesthesia
Article Information
Kanika Arora1*, Adarshchandra Swami2, Padma Puppala2, Ankita Rai2
1Department of Anesthesiology, Associate Specialist, Lilavati Hospital, Mumbai, India
2Department of Anesthesiology, Fortis Hospital, Mohali, India
*Corresponding Author: Kanika Arora, Department of Anesthesiology, Associate Specialist, Lilavati Hospital, Bandra West, Mumbai India
Received: 21 May 2020; Accepted: 17 June 2020; Published: 30 June 2020
Citation: Adarshchandra Swami, Kanika Arora, Padma Puppala. Comparative Study of Automated End Tidal Control Versus Manual Fresh Gas Flow Adjustment with Respect to Gas Usage and Delivery during Low Flow Anesthesia. Anesthesia and Critical Care 2 (2020): 039-051.
View / Download Pdf Share at FacebookAbstract
Background: During low-flow manually-controlled anesthesia (MCA) the anesthetist keeps adjusting end-tidal oxygen (EtO2) and anesthetic concentrations (EtAA) constantly to ensure adequate and safe anesthesia. This study was performed to compare End Tidal Control and Manual Control of Fresh gas flow during low flow anesthesia.
Methods: Study was conducted on 84 ASA I and II patients 18-65 years age, of either sex, requiring general anesthesia for more than 2 hours. In MCA group (n = 42) target end-tidal desflurane (4%) and EtO2 concentrations (≥ 35%) were manually controlled by the anesthetist. In EtCA group (n = 42), same anesthetic machine with additional end-tidal control feature was used to reach same targets.
Results: The median desflurane consumption was 15.71 ml and 16.71 ml in ETCA and MCA respectively (p value =0.002) after one hour and 28.71ml and 32.98 ml in ETCA and MCA respectively (p value <0.001 ) after two hours. In ETCA group, median number of adjustments was 3.83 after one hour and 7 after two hours (p – value <0.001). Cost of anesthetic agent consumed after one hour in ETCA group was Rs 562.57 and MCA group was Rs 598.37 (p value<0.002) . After two hours, cost of anesthetic agent consumed in ETCA group was Rs 1008.367 and in MCA group was Rs 1173.729 (p value <0.001).
Conclusion: Automatic implementation of low flow anesthesia using end tidal control is a good system for conserving the consumption of gases and reducing the number of adjustments needed to maintain depth of anesthesia.
Keywords
Anesthesia; Anesthesia Machine; Desflurane; End Tidal Control; Low Flow Anesthesia
Anesthesia articles, Anesthesia Machine articles, Desflurane articles, End Tidal Control articles, Low Flow Anesthesia articles
Anesthesia articles Anesthesia Research articles Anesthesia review articles Anesthesia PubMed articles Anesthesia PubMed Central articles Anesthesia 2023 articles Anesthesia 2024 articles Anesthesia Scopus articles Anesthesia impact factor journals Anesthesia Scopus journals Anesthesia PubMed journals Anesthesia medical journals Anesthesia free journals Anesthesia best journals Anesthesia top journals Anesthesia free medical journals Anesthesia famous journals Anesthesia Google Scholar indexed journals Anesthesia Machine articles Anesthesia Machine Research articles Anesthesia Machine review articles Anesthesia Machine PubMed articles Anesthesia Machine PubMed Central articles Anesthesia Machine 2023 articles Anesthesia Machine 2024 articles Anesthesia Machine Scopus articles Anesthesia Machine impact factor journals Anesthesia Machine Scopus journals Anesthesia Machine PubMed journals Anesthesia Machine medical journals Anesthesia Machine free journals Anesthesia Machine best journals Anesthesia Machine top journals Anesthesia Machine free medical journals Anesthesia Machine famous journals Anesthesia Machine Google Scholar indexed journals Desflurane articles Desflurane Research articles Desflurane review articles Desflurane PubMed articles Desflurane PubMed Central articles Desflurane 2023 articles Desflurane 2024 articles Desflurane Scopus articles Desflurane impact factor journals Desflurane Scopus journals Desflurane PubMed journals Desflurane medical journals Desflurane free journals Desflurane best journals Desflurane top journals Desflurane free medical journals Desflurane famous journals Desflurane Google Scholar indexed journals End Tidal Control articles End Tidal Control Research articles End Tidal Control review articles End Tidal Control PubMed articles End Tidal Control PubMed Central articles End Tidal Control 2023 articles End Tidal Control 2024 articles End Tidal Control Scopus articles End Tidal Control impact factor journals End Tidal Control Scopus journals End Tidal Control PubMed journals End Tidal Control medical journals End Tidal Control free journals End Tidal Control best journals End Tidal Control top journals End Tidal Control free medical journals End Tidal Control famous journals End Tidal Control Google Scholar indexed journals Low Flow Anesthesia articles Low Flow Anesthesia Research articles Low Flow Anesthesia review articles Low Flow Anesthesia PubMed articles Low Flow Anesthesia PubMed Central articles Low Flow Anesthesia 2023 articles Low Flow Anesthesia 2024 articles Low Flow Anesthesia Scopus articles Low Flow Anesthesia impact factor journals Low Flow Anesthesia Scopus journals Low Flow Anesthesia PubMed journals Low Flow Anesthesia medical journals Low Flow Anesthesia free journals Low Flow Anesthesia best journals Low Flow Anesthesia top journals Low Flow Anesthesia free medical journals Low Flow Anesthesia famous journals Low Flow Anesthesia Google Scholar indexed journals End Tidal Anesthetic agent articles End Tidal Anesthetic agent Research articles End Tidal Anesthetic agent review articles End Tidal Anesthetic agent PubMed articles End Tidal Anesthetic agent PubMed Central articles End Tidal Anesthetic agent 2023 articles End Tidal Anesthetic agent 2024 articles End Tidal Anesthetic agent Scopus articles End Tidal Anesthetic agent impact factor journals End Tidal Anesthetic agent Scopus journals End Tidal Anesthetic agent PubMed journals End Tidal Anesthetic agent medical journals End Tidal Anesthetic agent free journals End Tidal Anesthetic agent best journals End Tidal Anesthetic agent top journals End Tidal Anesthetic agent free medical journals End Tidal Anesthetic agent famous journals End Tidal Anesthetic agent Google Scholar indexed journals End Tidal Oxygen articles End Tidal Oxygen Research articles End Tidal Oxygen review articles End Tidal Oxygen PubMed articles End Tidal Oxygen PubMed Central articles End Tidal Oxygen 2023 articles End Tidal Oxygen 2024 articles End Tidal Oxygen Scopus articles End Tidal Oxygen impact factor journals End Tidal Oxygen Scopus journals End Tidal Oxygen PubMed journals End Tidal Oxygen medical journals End Tidal Oxygen free journals End Tidal Oxygen best journals End Tidal Oxygen top journals End Tidal Oxygen free medical journals End Tidal Oxygen famous journals End Tidal Oxygen Google Scholar indexed journals bispectral index articles bispectral index Research articles bispectral index review articles bispectral index PubMed articles bispectral index PubMed Central articles bispectral index 2023 articles bispectral index 2024 articles bispectral index Scopus articles bispectral index impact factor journals bispectral index Scopus journals bispectral index PubMed journals bispectral index medical journals bispectral index free journals bispectral index best journals bispectral index top journals bispectral index free medical journals bispectral index famous journals bispectral index Google Scholar indexed journals Train of four articles Train of four Research articles Train of four review articles Train of four PubMed articles Train of four PubMed Central articles Train of four 2023 articles Train of four 2024 articles Train of four Scopus articles Train of four impact factor journals Train of four Scopus journals Train of four PubMed journals Train of four medical journals Train of four free journals Train of four best journals Train of four top journals Train of four free medical journals Train of four famous journals Train of four Google Scholar indexed journals
Article Details
1. Introduction
The anesthetist’s job is both art and science — a fluid blend of expertise and hard data, all aimed at tailoring the optimal anesthesia plan for each patient. Anesthetists spend valuable time checking and re-checking EtO2 (End Tidal Oxygen) and EtAA (End Tidal Anesthetic agent) values, adjusting oxygen and agent settings, re-adjusting for changes in uptake and metabolic rate, to ensure safe and effective anesthesia. Over the years, the conventional anesthesia machine has evolved into an advanced care station. The new machines use advanced electronics, software and technology to offer extensive capabilities for ventilation, monitoring, inhaled agent delivery, low-flow anesthesia and closed-loop anesthesia. They offer integrated monitoring and recording facilities and seamless integration with anesthesia information systems. It is possible to deliver tidal volumes accurately and eliminate several hazards associated with the low-pressure system and oxygen flush. However, these workstations have brought in a new set of limitations and potential drawbacks. There are differences in technology and operational principles amongst the new workstations [1]. Inhaled anesthesia can be costly, and the variable costs of gases and anesthetic agents, determined by the fresh gas flow rates and vaporizer settings, are potential targets for cost savings. Understanding factors that contribute to the costs of inhaled anesthesia and considering those factors in pharmaco-economic analyses and recommendations for use of these agents can result in cost savings [1]. Et Control is an optional gas delivery mode for the fully digital Aisys Carestation from GE Healthcare. With Et Control the clinician sets the target EtO2 and EtAA values, the system constantly monitors the patient’s EtO2 and EtAA values and automatically adjusts the gas delivery and total flow to achieve and maintain the set target values (Image 1). During low-flow manually-controlled anesthesia (MCA) the anesthetist needs to keep adjusting end-tidal oxygen (EtO2) and anesthetic concentrations (EtAA) constantly to ensure an adequate and safe anesthesia (Image 2). Recently introduced anesthetic machines can automatically maintain those variables at target values, avoiding the burden on the anesthetist [2, 3].. Intelligent in-built safeguards protect against over-delivery and underdelivery of agent and hypoxia while providing the clinician with peace of mind and total control at all times. End Tidal Control relieves the clinician of tasks that are not only tedious and time-consuming but also potentially distracting, and positively impact the overall patient care process. In manual control of fresh gas flow, the anesthetist has to manually control the amount of gas to be delivered and constantly keep observing if the target levels are achieved or not. This study is an attempt to compare End Tidal Control and Manual Control of Fresh gas flow during low flow anesthesia. End Tidal Control was evaluated in clinical practice by measuring volatile agent consumption and the need for user input. These values were compared with contemporaneous controls using manual control of fresh gas flow rates.

Image 1: End tidal control mode.

Image 2: Manual fresh gas flow mode.
2. Material and Methods
The study has been conducted in the Department of Anesthesiology and Intensive care at Fortis Hospital Mohali after an approval of the same by the Institutional Ethics Committee. An informed and written consent was obtained from all patients involved in study. A total number of 84 patients undergoing surgery under general anesthesia were included in the study and randomly divided into two groups, using computer based randomization.
Group I (n=42) - End Tidal Control
Group II (n=42) - Manual Fresh Gas flow
2.1 Study area
Multi Specialty Operation Theatre, Fortis Hospital Mohali.
2.2 Study population
The study was conducted on 84 ASA I and II patients of either sex, of age group 18-65 years posted for a surgery requiring general anesthesia of expected duration greater than 2 hours in Fortis Hospital Mohali. There were 42 patients in each group.
2.3 Sample size justification
Sample size was estimated based on previous studies. (S Singaravelu, P Barclay - British Journal of Anesthesia Page 1 of 6 2013). Our sample size came out to be 38 subjects per group at a power of 80% & confidence interval of 95 %. It was decided to include extra subjects so 42 subjects were included in each group.
2.4 Preoperative evaluation and preparation
Routine preanesthetic examination of all the patients was performed a day prior to surgery. Patients who were willing to participate in the study were informed and a written consent was taken. These patients were randomized using computer based randomization. These patients were kept nil per oral for 6 hours and a premedication of alprazolam 0.25 mg and tab ranitidine 150 mgs was given 2 hours prior to surgery according to institutional protocol.
2.5 Anesthesia technique
On the day of surgery baseline parameters of the patients, such as heart rate, systolic, diastolic, mean blood pressure and saturation were recorded in the preoperative room. Operation theatre: Electrocardiogram, noninvasive blood pressure, pulse oximeter, end tidal gas monitoring, entropy analysis/ bispectral index (BIS) and Train of four (TOF) were used as standard monitoring in all patients. Anesthesia workstation of Datex Ohmeda Aisys and multipara monitor of Phillips with BIS engine of Aspect was used for avoiding bias in calibration of different machines (Image 3,4). Before induction of anesthesia, routine check of machine including leak proof test and the monitors was performed. Injection midazolam 0.05mg/kg was given intravenously after establishing an iv cannula. Preoxygenation with 100% oxygen was done for 3 minutes. Injection Lignocaine (2%) 1 ml IV was given 30 seconds prior to propofol administration. Injection Fentanyl 2 mcg/kg and Injection propofol 2mg/kg body weight intravenously was given for induction of anesthesia. After confirming mask ventilation, Injection Rocuronium 0.6 mg/kg IV was given. Lungs were ventilated with a mixture of oxygen/air. Intubation was done using portex cuffed endotracheal tube sized 7.0-7.5 mm for female and 8.0-8.5 mm for male patients. Bilateral air entry was checked and patient were ventilated, on volume-controlled mode, anesthesia was maintained using 50% oxygen/air mixture (total gas flow 1 litre), >35% FiO2, and Desflurane. Dexmedetomidine is supplied in 2 ml ampoules of 100 μg/ml concentrations (Dexem) (Themis medicare limited), which was diluted with NaCl 0.9% to yield a total volume of 50 ml and a total concentration of 4 μg/ml. No bolus dose of dexmedetomidine was given, and the infusion was started after anesthesia induction at 0.5 μg/kg/hour.
2.6 Ventilator settings were as follows
One of the modes, either end tidal control or manual fresh gas flow, being tested in the study was chosen. When manual fresh gas flow was being used then initially concentration of Desflurane was increased to 2 MAC to achieve the desired concentration of 4% desflurane with flow rate 1litre/min and once the end tidal concentration of desflurane was achieved, keeping the flow rate at 1 litre/min the concentration of desflurane was brought down to 4 %. If end tidal control was used then the flow was set at 1 litre/min and desflurane concentration at 4 % which it achieved automatically. Tidal volume 4-7 ml/kg, respiratory rate according to EtCO2 (maintained between 30-40), peak airway pressures were monitored, end tidal gas concentration was adjusted according to entropy monitoring (40-60 BIS value). Blood pressure and heart rate were recorded every 5 minutes throughout intraoperative period. End tidal desflurane concentration was maintained and adjusted according to entropy analysis. Bispectral index monitor readings between 40 and 60 are considered to be associated with adequate depth of anesthesia. Inadequate depth of anesthesia was treated incrementally by raising the Desflurane end-tidal concentration by 0.5% until the BIS reading drops back to <60. On the other hand, BIS readings <40 was managed by dropping the desflurane end-tidal concentration by 0.5%. The aim was also to maintain arterial blood pressure within 20% of the baseline values. Mean arterial pressure increase up to >20% above the baseline, with adequate BIS readings (40-60), was treated by administering a 0.5 μg/kg intravenous bolus of fentanyl, while an arterial blood pressure drop of >20% below the baseline was treated with reduction of the end-tidal desflurane concentration by 0.5% if the BIS readings were >60, or a 3 mg of mephentermine if the BIS readings were between 40 and 60. Neuro muscular blocking agents (NMBAs) were administered according to the TOF watch. At the end of surgery, residual neuromuscular blockade was reversed using glycopyrrolate, 0.01 mg/kg IV, and neostigmine, 0.05 mg/kg IV. Patients were extubated after TOF ratio was >80% and patients started following verbal commands. Patients were shifted to postoperative area. After one hour and two hours the amount of gas used was checked and the number of interventions required in each mode to maintain a constant depth of anesthesia was noted. Results were tabulated, statistically analyzed and compared.
2.7 Statistical analysis
A statistical analysis was carried out using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, version 18.0 for Windows). Mean & medians were calculated for all quantitative variables and for measures of dispersion standard deviation, standard error or IQR were calculated. Normality of data was checked by measures of Kolmogorov Smirnov tests of normality. For normally distributed data means of 2 groups were compared using student t-test. For skewed data or for scores Mann –Whitney test were applied. Comparison of multiple time related variables within cases was done by Repeated Measure ANOVA followed by One Way ANOVA. Wilcoxon signed rank test was applied to see statistical difference between time related variables if data is skewed. All statistical analysis tests were two tailed and P value < 0.05 was taken as significant.
Image 3: Bispectral Index being used on patient.

Image 4: Monitor showing Bispectral Index reading.
3. Results
In our case control observational study, we included two comparable groups with respect to age, weight, height, BMI, laboratory values and ASA classification (table 2-4). Each group had 42 patients (table 1). Group 1 (n=42) end tidal controlled anesthesia and Group 2 (n=42) manually controlled anesthesian group. In MCA group (n = 42) target end-tidal desflurane (4%) and EtO2 concentrations (≥ 35%) were manually controlled by the anaesthetist. In EtCA group (n = 42) the same anaesthetic machine with an additional end-tidal control feature was used to reach the same targets, rendering automatic the achievement and maintenance of those targets. The amount of consumption of anaesthetic agent after one hour and after two hours was calculated by the anesthesia machine in both groups and the number of attempts made to maintain the end tidal concentration was noted. The demographic characteristics of the patients in the two groups were comparable. There was no statistical difference among the two groups with respect to age, sex, weight or height. There was no statistically significant difference in the ASA status of patients among the two groups (Table 1-3).
Baseline haemodynamics were comparable among the two groups. There was no statistically significant difference in haemodynamics during two hours after induction (Figure 1-3). Amount of agent used after 1 hour was recorded for Et control and Manual fresh gas flow. The mean gas usage for Et control group (n=42) was 15.71ml and for manual fresh gas flow group (n=42) was 16.71ml. (p- value = 0.002). Amount of agent used after 2 hour was recorded for Et control and Manual fresh gas flow.
The mean gas usage for at control group (n=42) was 28.71ml and for manual fresh gas flow group (n=42) was 32.98ml (p value <0.001) (Table 4). BIS was monitored throughout the surgery. Constant depth of anesthesia was maintained in both the groups and there was no statistically significant difference in BIS values, but continous manual adjustments were required to achieve this constant depth of anesthesia in Manual fresh gas flow mode as compared to ET control group. Number of attempts made to maintain constant level of anesthesia was compared in the two groups and there was statistically significant difference in both groups (p<0.001). There was significant decrease in number of attempts in end tidal control group patients as compared to manual control group (p=0.019) (Table 5).
Cost effectiveness was evaluated. Cost analysis was carried out on the basis of amount of agent used. The total amount of agent used was multiplied with the cost of 1 ml of Desflurane (Rs 35.8/ml as a bottle of 240 ml of Desflurane costs Rs 8600) and the results were compared (Table 6). End tidal control came out to be more cost effective as compared to manual fresh gas flow group. The savings per year by using End Tidal control mode came out to be about Rs 223088. A few episodes of hypotension were seen in our study, but they were well controlled with inj. Mephenteramine and the episodes of Bradycardia were controlled with inj Atropine. The episodes of Hypertension and Tachycardia initially were managed by adjusting BIS within 40-60 with ET control of Desflurane. If not corrected by this maneuver, then inj fentanyl 20 mcg IV was given. The number of attempts taken for changing settings to maintain constant depth of anesthesia were compared in both the groups. After 1 hour, in Et control group (n=42) mean attempts made were 3.83 and for manual fresh gas flow group (n=42) mean attempts were 13.93. (p-value 0.000). After 2 hours, in Et control group (n=42) mean attempts made were 7.00 and for manual fresh gas flow group (n=42) mean attempts were 25.24. (p-value <0.001).
|
S NO |
Group I |
Group II |
P value |
Significance |
|
Age (Years) |
43.33 ± 10.403 |
43.33 ± 11.272 |
1.000 |
NS |
|
BMI |
26.0213 ± 2.50578 |
25.6902 ± 2.78894 |
0.569 |
NS |
Table 1: Demographic profile (MEAN ± SD).
|
Sex |
Et Control |
Manual Fresh Gas flow |
|
Group |
I (n=42) |
II (n=42) |
|
Male |
19 |
12 |
|
Female |
23 |
30 |
P= (Not Significant)
Table 2: Sex distribution of the patients.
|
Group |
Et Control (n=42) |
Fresh Gas flow (n=42) |
|
ASA I |
31 |
33 |
|
ASA II |
11 |
8 |
P= (not significant)
Table 3: ASA grade distribution of the patients.
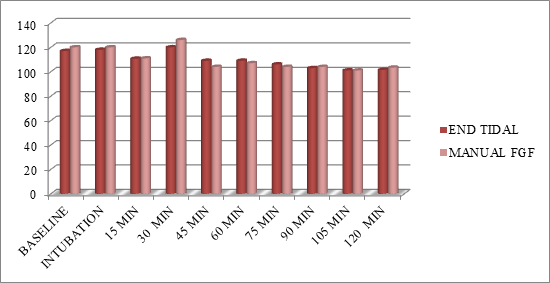
Figure 1: Comparing SBP between the two group of patients.
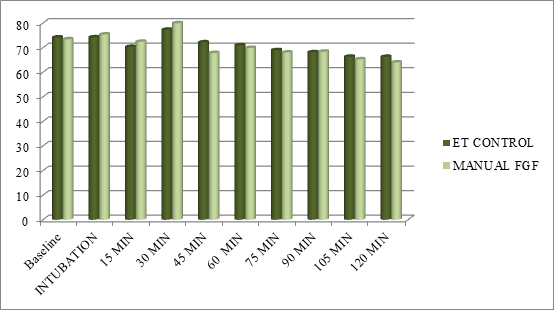
Figure 2: Comparing DBP Between the two Groups.
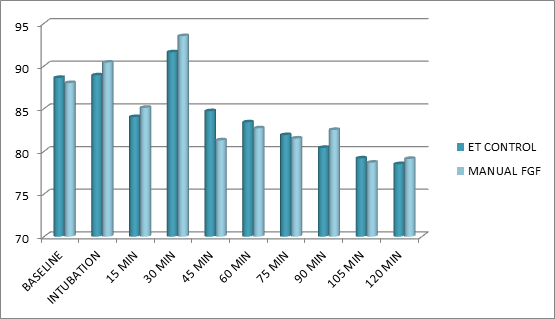
Figure 3: Comparing MAP between the two groups.
|
Et Control |
Manual Fresh Gas flow |
P – value |
|
|
Amount of agent used after 1 hour |
15.71 ML |
16.71 ML |
0.002 |
|
Amount of agent used after 2 hours |
28.71 ML |
32.98 ML |
<0.001 |
Table 4: Amount of agent used after 1 hour and 2 hours of induction.
|
Et Control |
Fresh Gas flow |
P – value |
|
|
Attempts Made (Mean) |
3.83 |
13.93 |
0.000 |
|
Attempts Made (Mean) |
7.00 |
25.24 |
<0.001 |
Table 5: Attempts taken to maintain depth of anaesthesia after 1 hour and 2 hours of induction.
|
ET CONTROL |
FRESH GAS flOW |
P – value |
|
|
Cost Of Anaesthetic Agent after 1 hour (mean) in rupees |
562.57 |
598.37 |
0.002 |
|
Cost Of Anaesthetic Agent After 2 Hours Of Surgery |
1008.367 |
1173.729 |
<0.001 |
Table 6: Cost of anaesthetic agent after 1 hour and 2 hours of induction.
4. Discussion
Anesthesia machines have come a long way in the last 100 years, the improvements being driven both by patient safety as well as functionality and economy of use. Incorporation of safety features in anesthesia machines and ensuring that a proper check of the machine is done before use on a patient ensures patient safety. Since the End tidal control mode putatively guarantees the set values of end-tidal anaesthetic gas and oxygen concentrations, as well as the fresh gas flow with minimal manual intervention, we decided to test its efficacy to maintain adequate level of anesthesia in patients. The study also looked at consumption of anaesthetic agent in ET control mode compared to manual control. S Singaravelu et al. [4] evaluated EtControl in clinical practice by measuring volatile agent consumption and the need for user input. They compared these values with contemporaneous controls using manual control of fresh gas flow rates. They concluded that automatic implementation of low-flow anesthesia using Et Control allows the user to set and maintain a desired end-tidal volatile concentration while using less volatile agent. This is consistent with the observations in our study. Lortat-Jacob, B., et al. [5] assessed the clinical benefits and economic impact of this target-controlled anesthesia compared with conventional manually controlled anesthesia. They concluded that the auto-control mode provided similar haemodynamic stability and bispectral control as did conventional manually controlled anesthesia but led to a reduction in gas and vapour consumption with a more clinically acceptable workload. Tay et al [6] hypothesized that automated control of end-tidal gases, a new feature in anesthesia machines, will consistently reduce volatile agent consumption cost and greenhouse gas emissions.
As part of the planned replacement of anesthesia machines in a tertiary hospital, they performed a prospective before and after study comparing the cost and greenhouse gas emissions of isoflurane, sevoflurane and desflurane when using manual versus automated control of end-tidal gases. They concluded that automated control of end-tidal gases increases participation in low flow anesthesia with economic and environmental benefits. This was observed in our study as well. ET control came out to be much more cost effective as compared to Manual fresh gas flow. Lucangelo et al. [2] prospectively observed eighty patients. In MCA group (n = 40) target end-tidal sevoflurane (1 %) and EtO2 concentrations (≥35 %) were manually controlled by the anaesthetist. They concluded that low-flow anesthesia delivered with an anaesthetic machine able to automatically control EtAA and EtO2 provided the same clinical stability and avoided the continuous manual adjustment of delivered sevoflurane and oxygen concentrations. Hence, the anaesthetist could dedicate more time to the patient and operating room activities. Sieber et al [7] studied the clinical use of an automatic feedback control system to adjust the end-tidal anaesthetic concentration with a low-flow method. They concluded that automatic control system showed a faster response time than the manual method only with large increasing step and was not different from manual control for decreasing steps. Automatic control of the end-tidal isoflurane concentration can be better than human control in a clinical setting, and this task could be done automatically. Cotter, S. M., et al [8] conducted an 8 week survey to determine whether the introduction of low-flow anesthesia into routine use would be acceptable to members of a representative anaesthetic department and if the consequent reduction in use of volatile anaesthetics would result in financial savings.
The hourly consumption of the volatile agents was measured during anesthesia conducted using either conventional or low fresh gas flows. Thus, they concluded that the routine use of low-flow anesthesia would therefore be acceptable and could result in annual savings of 26,870 pounds at Northwick Park Hospital. Kennedy and French [3] described data from an audit that monitored fresh gas flow rates within a single department in a New Zealand hospital and concluded that introduction of the Aisys systems with End tidal control, the mean fresh gas flow rates initially increased to 1.5 litres per minute, but dropped to 1.09 litres per minute after 12 months. We hypothesized that in Et control mode there is less use of anaesthetic agent, is more cost effective and reduces the number of adjustments needed to maintain depth of anesthesia. As per the observations and results of our study we can see that Et control mode proves to be beneficial over manual fresh gas flow mode in terms of anaesthetic agent consumption, cost effectiveness and the number of setting changes required to achieve a constant depth of anesthesia. We also observed that the effectiveness of Et control came out to be more in longer duration ssurgeries, thusproving its role in neurosurgeries, transplant surgeries and surgeries exceeding more that 1 hour duration.
Conflict of Interest
None
References
- Patil VP, Shetmahajan MG, Divatia JV. The modern integrated anesthesia workstation. Indian journal of anesthesia 57 (2013): 446.
- Lucangelo U, Garufi G, Marras E, et al. End-tidal versus manually-controlled low-flow anesthesia. Journal of clinical monitoring and computing 28 (2014): 117-121
- Kennedy RR. New technology in anesthesia: Friend or foe. Journal of clinical monitoring and computing. 28 (2014): 113-116.
- Singaravelu S, Barclay P. Automated control of end-tidal inhalation anaesthetic concentration using the GE Aisys Carestation™. British journal of anesthesia (2013): aes464.
- Lortat-Jacob B, Billard V, Buschke W, et al. Assessing the clinical or pharmaco-economical benefit of target controlled desflurane delivery in surgical patients using the Zeus® anesthesia machine*. Anesthesia 64 (2009): 1229-1235.
- Tay S, Weinberg L, Peyton P, et al. Financial and environmental costs of manual versus automated control of end-tidal gas concentrations. Anesthesia and intensive care 41 (2013): 95.
- Sieber TJ, Frei CW, Derighetti M, et al. Model-based Automatic Feedback Control Versus Human Control of End-Tidal Isoflurane Concentration Using Low-flow Anesthesia. Br J Anaesth 85 (2000): 818-825.
- Cotter SM, Petros AJ, Dore CJ, et al. Low-flow anesthesia. Anesthesia 46 (1991): 1009-1012.
- Golembiewski J. Economic considerations in the use of inhaled anesthetic agents. American Journal of Health-System Pharmacy 67 (2010): S9.
