Comparative Evaluation Between 2mm Locking and 2mm Non-Locking Miniplate System for Open Reduction and Internal Fixation of Mandibular Parasymphysis Fracture
Article Information
Dr. Rajarshi Bandyopadhyay1*, Prof. Dr. Amit Ray2, Dr. Tanmoy Ghorui1
1Assistant professor, Department Of Oral and Maxillofacial Surgery, Guru Nanak Institute of Dental Science Panihati, Kolkata, India
2Professor and Head Of The Department of Oral and Maxillofacial Surgery, Guru Nanak Institute of Dental Science and Research, Panihati, Kolkata, India
*Corresponding Author: Dr. Rajarshi Bandyopadhyay, Assistant professor, Department Of Oral and Maxillofacial Surgery, Guru Nanak Institute of Dental Science Panihati, Kolkata, India
Received: 31 March 2020; Accepted: 09 April 2020; Published: 11 May 2020
Citation: Rajarshi Bandyopadhyay, Amit Ray, Tanmoy Ghorui. Comparative Evaluation Between 2mm Locking and 2mm Non-Locking Miniplate System for Open Reduction and Internal Fixation of Mandibular Parasymphysis Fracture. Archives of Clinical and Medical Case Reports 4 (2020): 369-383.
View / Download Pdf Share at FacebookAbstract
Aims: To compare the stability, rigidity, bone healing and functional outcome of 2mm locking and 2mm non-locking miniplate system in mandibular parasymphysis fracture.
Material and method: The was conducted at dept. of oral and maxillofacial surgery, GNIDSR, Kolkata, India, from May 2016, to December, 2019, 34 patients (male 30 and female 4) were randomly divided into 2 groups. The patients underwent osteosynthesis—Group A (n=17, 15 males and 2 females) with orthomax 2-mm locking titanium miniplates(LMP) and Group B (n=17, 15 males and 2 females) with orthomax 2-mm nonlocking titanium miniplates(NLMP). The age, gender, operating time, pain and swelling, mobility, occlusion, chewing efficacy, bony healing with radiological evaluation were all reviewed. The assessment of the patients was done preoperatively and postoperative days at 1 day, 3 day, 7th day, 14th day, 1st month, 2nd month, and 3rd month using the clinical parameters, observation and radiology.
Results: A total of 34 parasymphysis fractures met the inclusion criteria. In our study, a statistically significant difference was not found in the clinical parameters such as operating time, pain, swelling, occlusion, chewing efficacy, mobility between the fracture segments and infection, hardware failure in postoperative period. A statistically significant difference was found in the CT scan evaluation with pre-op and post op fracture width and hounsfield unit in between two groups at preop and 3rd month postop days and it was also supported by OPG findings.
Conclusion: We concluded that Locking miniplates are technically not cumbersome than non-locking one – No significant increase in operating time. Use of two locking miniplates in the parasymphysis region placed on the Champy’s line of oesteosynthesis provides a better stability and oesteosynthesis at t
Keywords
Mandibular Parasymphysis Fracture, Locking miniplate, Non-locking miniplate, Hounsfield unit
Mandibular Parasymphysis Fracture articles, Locking miniplate , Non-locking miniplate articles, Hounsfield unit articles
Mandibular Parasymphysis Fracture articles Mandibular Parasymphysis Fracture Research articles Mandibular Parasymphysis Fracture review articles Mandibular Parasymphysis Fracture PubMed articles Mandibular Parasymphysis Fracture PubMed Central articles Mandibular Parasymphysis Fracture 2023 articles Mandibular Parasymphysis Fracture 2024 articles Mandibular Parasymphysis Fracture Scopus articles Mandibular Parasymphysis Fracture impact factor journals Mandibular Parasymphysis Fracture Scopus journals Mandibular Parasymphysis Fracture PubMed journals Mandibular Parasymphysis Fracture medical journals Mandibular Parasymphysis Fracture free journals Mandibular Parasymphysis Fracture best journals Mandibular Parasymphysis Fracture top journals Mandibular Parasymphysis Fracture free medical journals Mandibular Parasymphysis Fracture famous journals Mandibular Parasymphysis Fracture Google Scholar indexed journals Parasymphysis Fracture articles Parasymphysis Fracture Research articles Parasymphysis Fracture review articles Parasymphysis Fracture PubMed articles Parasymphysis Fracture PubMed Central articles Parasymphysis Fracture 2023 articles Parasymphysis Fracture 2024 articles Parasymphysis Fracture Scopus articles Parasymphysis Fracture impact factor journals Parasymphysis Fracture Scopus journals Parasymphysis Fracture PubMed journals Parasymphysis Fracture medical journals Parasymphysis Fracture free journals Parasymphysis Fracture best journals Parasymphysis Fracture top journals Parasymphysis Fracture free medical journals Parasymphysis Fracture famous journals Parasymphysis Fracture Google Scholar indexed journals Locking miniplate articles Locking miniplate Research articles Locking miniplate review articles Locking miniplate PubMed articles Locking miniplate PubMed Central articles Locking miniplate 2023 articles Locking miniplate 2024 articles Locking miniplate Scopus articles Locking miniplate impact factor journals Locking miniplate Scopus journals Locking miniplate PubMed journals Locking miniplate medical journals Locking miniplate free journals Locking miniplate best journals Locking miniplate top journals Locking miniplate free medical journals Locking miniplate famous journals Locking miniplate Google Scholar indexed journals Non-locking miniplate articles Non-locking miniplate Research articles Non-locking miniplate review articles Non-locking miniplate PubMed articles Non-locking miniplate PubMed Central articles Non-locking miniplate 2023 articles Non-locking miniplate 2024 articles Non-locking miniplate Scopus articles Non-locking miniplate impact factor journals Non-locking miniplate Scopus journals Non-locking miniplate PubMed journals Non-locking miniplate medical journals Non-locking miniplate free journals Non-locking miniplate best journals Non-locking miniplate top journals Non-locking miniplate free medical journals Non-locking miniplate famous journals Non-locking miniplate Google Scholar indexed journals Hounsfield unit articles Hounsfield unit Research articles Hounsfield unit review articles Hounsfield unit PubMed articles Hounsfield unit PubMed Central articles Hounsfield unit 2023 articles Hounsfield unit 2024 articles Hounsfield unit Scopus articles Hounsfield unit impact factor journals Hounsfield unit Scopus journals Hounsfield unit PubMed journals Hounsfield unit medical journals Hounsfield unit free journals Hounsfield unit best journals Hounsfield unit top journals Hounsfield unit free medical journals Hounsfield unit famous journals Hounsfield unit Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals oesteosynthesis articles oesteosynthesis Research articles oesteosynthesis review articles oesteosynthesis PubMed articles oesteosynthesis PubMed Central articles oesteosynthesis 2023 articles oesteosynthesis 2024 articles oesteosynthesis Scopus articles oesteosynthesis impact factor journals oesteosynthesis Scopus journals oesteosynthesis PubMed journals oesteosynthesis medical journals oesteosynthesis free journals oesteosynthesis best journals oesteosynthesis top journals oesteosynthesis free medical journals oesteosynthesis famous journals oesteosynthesis Google Scholar indexed journals CT scan articles CT scan Research articles CT scan review articles CT scan PubMed articles CT scan PubMed Central articles CT scan 2023 articles CT scan 2024 articles CT scan Scopus articles CT scan impact factor journals CT scan Scopus journals CT scan PubMed journals CT scan medical journals CT scan free journals CT scan best journals CT scan top journals CT scan free medical journals CT scan famous journals CT scan Google Scholar indexed journals Anti-neutrophil cytoplasmic antibodies articles Anti-neutrophil cytoplasmic antibodies Research articles Anti-neutrophil cytoplasmic antibodies review articles Anti-neutrophil cytoplasmic antibodies PubMed articles Anti-neutrophil cytoplasmic antibodies PubMed Central articles Anti-neutrophil cytoplasmic antibodies 2023 articles Anti-neutrophil cytoplasmic antibodies 2024 articles Anti-neutrophil cytoplasmic antibodies Scopus articles Anti-neutrophil cytoplasmic antibodies impact factor journals Anti-neutrophil cytoplasmic antibodies Scopus journals Anti-neutrophil cytoplasmic antibodies PubMed journals Anti-neutrophil cytoplasmic antibodies medical journals Anti-neutrophil cytoplasmic antibodies free journals Anti-neutrophil cytoplasmic antibodies best journals Anti-neutrophil cytoplasmic antibodies top journals Anti-neutrophil cytoplasmic antibodies free medical journals Anti-neutrophil cytoplasmic antibodies famous journals Anti-neutrophil cytoplasmic antibodies Google Scholar indexed journals Surgery articles Surgery Research articles Surgery review articles Surgery PubMed articles Surgery PubMed Central articles Surgery 2023 articles Surgery 2024 articles Surgery Scopus articles Surgery impact factor journals Surgery Scopus journals Surgery PubMed journals Surgery medical journals Surgery free journals Surgery best journals Surgery top journals Surgery free medical journals Surgery famous journals Surgery Google Scholar indexed journals
Article Details
1. Introduction
Treatment of mandibular fracture is a very common surgical procedure in oral and maxillofacial surgery. Presently the choice of treatment in most of these cases is ORIF to have the proper rigidity of fracture segments, better masticatory efficiency and faster healing. Over the last decades the management of parasymphysis fracture has changed from maxillomandibular fixation (MMF) with or without internal wire fixation to DCP, EDCP and lag screws to miniplate and microplate fixation. Research continues to focus on implant material, type of implant, method of fixation and biomechanics of plate/screw systems. The locking plate and screw system has been available for more than three decades, there has recently been renewed interest in these systems, with a growing number of clinical studies. With conventional bone plating systems, stability is achieved when the head of the screw compresses the fixation plate to the bone. The plate must be perfectly adapted to the underlying bone to prevent alterations in the alignment of the segments and changes in the occlusal relationship.
The locking system uses a screw that locks not only to the bone but also to the bone plate. This is accomplished by having a screw with a double thread. One thread will engage the bone and another will engage a threaded area of the bone plate. The result is a locking plate system that in effect provides a mini internal fixator [1]. Other theoretical proposed advantages of the locking plate/screw systems over conventional plates and screws include less screw loosening, greater stability across the fracture site, less precision required in plate adaptation because of the ‘internal/external fixator’, and less alteration in osseous or occlusal relationship upon screw tightening. The main disadvantage of the locking system is cost and minor additions to the instrumentation required [1].
2. Material and Method
The study group comprised of 34 patients with fractures of mandibular symphysis or parasymphysis region who reported to the department of Oral and Maxillofacial Surgery of our institution. The study was granted approval by the institutional review board and the institutional ethical committee.
Inclusion criteria:
- Patient was selected not below than 18 yrs. of age.
- Simple and compound fracture of symphysis and parasymphysis
Exclusion criteria:
- Medically compromised patient was excluded from the study
- Poly trauma and comminuted fracture
- Debilitated patients who cannot bear a surgical stress.
- Edentulous patients.
All 34 patients are randomly assigned in two several groups.
Group A: 17 fractures are treated with 2 mm locking mini plate system according to the principles of Champy’s lines of osteosynthesis and zones of compression and tension.
Group B: 17 fractures are treated with 2mm non-locking mini plate system according to the principles of Champy’s lines of osteosynthesis and zones of compression and tension.
Inter-maxillary fixation was done with the help of arch-bar & tie wire. In group A after reduction of fracture segments the 2-mm locking plate (one or two depending upon site) was adapted over the fracture site. The drill guide was locked with the plate holes and drilling with 1.2 mm drill-bits was done under copious irrigation. Fixation of the reduced bony segment was performed with the screws inserted perpendicular to the plate surface. The surgical wound was sutured in layers using vicryl suture material and the skin layer with prolene suture material. Patients in group B were treated by the same procedure by using 2 mm non-locking plates and drill guide was not needed in the procedure. In all groups of patients intermaxillary fixation were kept only for per-operative procedure, after that it was removed. After completion of surgery all patients of both groups were kept on a standard drug regimen.
Various pre-operative, intra-operative and post-operative recordings were registered for comparison in between two plating system:
a. Measurement of total operating time2and time of it’s 5 several stages:
- Incision to exposure.
- Exposure to reduction with bone holding clamps (excluding IMF time).
- Adaptation of 2 plates iv) 1st drill to last placement of screws v) Time of closure.
b. Pain [3]: Pain was measured by the Verbal Rating Score (VRS) and Pain Relief Scale (PRS)on pre-operative and post-operative (1st, 2nd, 3rd, 7th, 14th, 30th, 60th, 90th ) days.
c. Swelling [4]: It was measured on preop, and post-operative 3rd , 7th , 14th , 30th , 60th, 90th days on the basis of linear measurement.
d. Mobility of the fracture segment [5]: Mobility of the fractured fragments was checked pre-operatively, post op 14th day, post op 30th day, post op 90th day.
e. Occlusion [5-7]: Occlusion was checked by direct observer preoperatively and 14th day, 2month and 3 month postoperatively.
f. Self-Evaluation of chewing: Ability to chew normal diet was evaluated preoperatively and 2nd and 3rd post op months by patients on its own. (Unable to chew=1, soft diet= 2, normal diet but on one side=3, normal diet=4)D6.
g. Ct scan evaluation done in preoperatively and 3rd month postoperatively (Figure 1-3):
- Width of the fracture line in measured at the buccal and lingual cortex, in the superior and inferior border of the mandible (axial section) and also at the superior and inferior border (Coronal section).
- Hounsfield unit of bone is also measured in coronal and axial sections at the superior border (buccal and lingual cortex), inferior border (buccal and lingual cortex) &medullary bone to see the bony healing.
h. OPG evaluation [8]: We used Grey scale measurement to evaluate bony healing from OPG. Four lead foil was placed one over another to obtain 5 shades wedge and these wedge were being graded numerically. Grade 1 to grade 5 was obtained by this procedure (Figure 4 and 5) and it was being compared with the radiolucency present in the fracture line preoperatively as well as 3 month postoperatively.
i. Postoperative complications [5, 7, 9-11]: Soft tissue infection and bone infections were noticed postoperatively at 1st month, 2nd month and 3rd month in both the groups. Hardware hazard and plate exposure were checked in 3rd month postoperatively in both the groups. The parameters, thus recorded, are subjected to statistical evaluation, to evaluate the effectiveness of locking and non-locking titanium miniplating system in ORIF of mandibular fracture.
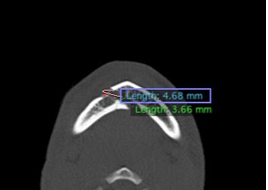
Figure 1: Preoperative fracture width measurements(axial section).
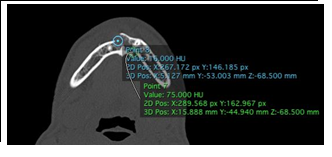
Figure 2: Preop HFU measurement (axial section).
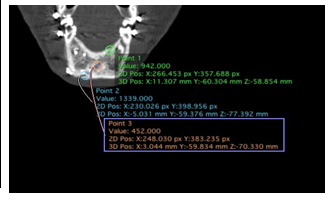
Figure 3: Post op HFU measurement (coronal section).

Figure 4: Wedge made by 4 lead foils.

Figure 5: Gray scale standardization.
3. Results
34 patients (30 males & 4 females) with simple or compound parasymphysis fractures were divided into Group A and Group B and treated with locking and non-locking miniplating system. Total operating time for both the groups do not show any significant changes (t-test 1.10; p 0.28) and as it is divided into 5 separate steps, t-test also remain insignificant with in two groups;
- Incision to exposure- t-test 0.61; 0.54
- Exposure to reduction- t-test 0.39;p 0.69
- Adaptation of plates t-test 1.29;p 0.21
- 1st drill to last placement of screws t-test 1.47 ;p 0.15
- Time of closure. t-test 0.49; p 0.62.
Corrected chi-square test showed that there was significant association between VRS in Group A and Group B in preoperative days. There was significant reduction in pain from 14th days postoperatively in both groups. (Group A Chi-square=85.30; p<0.001 & Group B: chi-square=68.30; p<0.001). Absence of pain from 1st month was also noticed. In respect to Pain Relief Scale t-test showed no significant differences within Group A and Group B in different time interval. (p>0.05) t-test showed no significant differences in respect to swelling in between two groups in different time interval (p>0.05). Test of proportion showed that proportion patients with Mobility of Facture Parasymphysis and Body decreased significantly in both the groups after surgery (Z=3.03; p<0.001).
Test of proportion showed that proportion patients with molar occlusion decreased significantly in both the groups after surgery (Z=6.68; p<0.001). Test of proportion showed that proportion patients with canine occlusion decreased significantly in both the groups after surgery (Z=4.26; p<0.001). As per chi-square test there were no significant association in patterns of self-evaluation of chewing of the patients of the two groups (p>0.05). Thus, the patterns of self-evaluation of chewing of the patients of the two groups were more or less similar. At 2nd month only 3 patients of Group-A and 4 patients of Group-B required Soft diet. At 3rd months only 1 patient of Group-B required Soft diet and all the patients of Group-A were with normal diet.
In the superior border of the mandible over the fracture line in coronal CT section t test showing significant difference preoperatively within Group A and Group B. The width of the fracture at the superior border is higher in Group A (t-test 2.98; p<0.01) but at the 3rd month postoperative period there were no significant differences within both the groups (t-test 0.26; p>0.05). In case of HFU evaluation at the superior border, the t-test also showed similar result.
In the Inferior border of the mandible over the fracture line in coronal CT section t test showed no significant differences of fracture width at the inferior border (coronal section) within Group A and Group B preoperatively as well as 3rd month postoperatively (p>0.05) but t-test showed the mean fracture width at the inferior border (coronal section) of the patients of Group A decreased significantly at 3rd month as compared to before surgery (t test – 4.12; p<0.01). In Group B it had also decreased but it is not statistically significant (t test- 2.12; p>0.05).In case of HFU measurement t- test showed significant difference in preoperatively within Group A and Group B. The HFU over the fracture line at the inferior border is significantly lower in Group A (p<0.001). At the 3rd month postoperative period there were no significant differences within both the groups.(p>0.05).In Group A HFU increased significantly at 3rd month as compared to preop (t-test 6.24;p<0.01) whereas in group B it increased but not significant(t-test2.12; p>0.05). The HFU over the fracture line at medullary bone is significantly lower in Group A than Group B (t-test 3.18; p<0.001).At the 3rd month In Group A the mean HFU over the fracture line at the medullary bone is significantly higher than Group B(t-test 2.48; p<0.01).
In axial section of the CT scan at the superior border in both buccal and lingual cortex t-test showed the mean of fracture width over the superior border in the buccal cortex as well as lingual cortex of the patients of Group A decreased significantly at 3rd month as compared to before surgery (p<0.01) but in Group B it was not significantly decreasing (p>0.05).
|
Superior Border# width: Buccal Cortex (axial) |
Preop |
3rd Month postop |
PREOP VS POSTOP |
PREOP VS POSTOP |
|||
|
A |
B |
A |
B |
A |
B |
||
|
Mean ± sd |
2.53 ± 1.89 |
1.73 ± 1.22 |
0.15 ± 0.25 |
0.48 ± 0.68 |
|||
|
Median |
2.14 |
1.39 |
0.00 |
0.00 |
|||
|
t-test |
2.26 |
1.42 |
5.61 |
1.97 |
|||
|
p-value |
<0.01* |
>0.05 |
<0.01* |
>0.05 |
|||
|
Superior Border#width: lingual Cortex (axial) |
Preop |
3rd Month postop |
PREOP VS POSTOP |
PREOP VS POSTOP |
||
|
A |
B |
A |
B |
A |
B |
|
|
Mean ± sd |
2.56 ± 1.44 |
1.14 ± 0.86 |
0.80 ± 0.60 |
0.60 ± 0.66 |
||
|
Median |
2.26 |
1.27 |
0.95 |
0.44 |
||
|
t-test |
2.12 |
0.79 |
3.34 |
1.56 |
||
|
p-value |
<0.01* |
>0.05 |
<0.01* |
>0.05 |
||
Table 1: Superior Border fracture width comparison pre-operatively and post-operatively in parasymphysis fracture of both groups.
HFU measurement at the superior border at both cortex and medullary bone signifies some difference in between both groups preoperatively and postoperatively. At the superior border buccal cortex, pre-op HFU of Group A was significantly lower than that of Group B (t=2.54; p<0.01). At 3rd month the mean HFU of Group A was lower than that of Group B but it was not significant (t=1.22; p>0.05). Almost similar result is also found in lingual cortex (pre-op Group A vs Group B: t-test 6.19; p<0.01.post-op Group A vs Group B: t-test 2.12; p>0.05) and medullary bone (pre-op Group A vs Group B: t-test 6.19; p<0.01.post-op Group A vs Group B: t-test 1.84; p>0.05).
The values as measured in the superior border similarly it was also measured at the inferior border of the mandible over the fracture line. t- test showed no significant difference in preoperatively within Group A and Group B at the fracture width on the buccal cortex of the inferior border as well as in 3rd month postoperative ct scan (p>0.05).But within the groups t-test showed the mean of fracture width over the inferior border in the buccal cortex of the patients of both the groups decreased significantly at 3rd month as compared to before surgery (p<0.01).
|
Inferior Border#width: buccal Cortex |
Preop |
3rd Month postop |
PREOP VS POSTOP |
PREOP VS POSTOP |
||
|
A |
B |
A |
B |
A |
B |
|
|
Mean ± sd |
1.87 ± 1.37 |
1.04 ± 0.58 |
0.24 ± 0.41 |
0.16 ± 0.30 |
||
|
Median |
1.22 |
1.11 |
0.00 |
0.00 |
||
|
t-test |
1.98 |
0.73 |
3.31 |
2.98 |
||
|
p-value |
>0.05 |
>0.05 |
<0.01* |
<0.01* |
||
Almost similar result was also shown in the measurement of the fracture width at the lingual cortex.
|
Inferior Border#width: lingual Cortex |
Preop |
3rd Month postop |
PREOP VS POSTOP |
PREOP VS POSTOP |
||
|
A |
B |
A |
B |
A |
B |
|
|
Mean ± sd |
2.19 ± 1.34 |
1.00 ± 0.82 |
0.64 ± 0.75 |
0.32 ± 0.62 |
||
|
Median |
2.05 |
1.11 |
0.56 |
0.00 |
||
|
t-test |
2.78 |
0.98 |
3.98 |
2.54 |
||
|
p-value |
0.61 |
0.86 |
<0.01* |
>0.05 |
||
Table 2: Inferior Border fracture width comparison pre-operatively and post-operatively in parasymphysis fracture of both groups.
HFU at the fracture line over the inferior border also showed same pattern like the fracture width at the buccal cortex (pre-op Group A vs Group B: t-test 2.44 ; p>0.05.post-op Group A vs Group B: t-test 1.22; p>0.05), lingual cortex ( pre-op Group A vs Group B: t-test 3.17; p<0.01.post-op Group A vs Group B: t-test 0.93; p>0.05) and medullary bone (pre-op Group A vs Group B: t-test 2.98; p>0.05.post-op Group A vs Group B: t-test 1.24; p>0.05). Corrected chi-square test showed that there was significant association with opg evaluation by gray scale (Grading system) in parasymphysis and body fracture and time interval (Chi-square=45.70; p<0.0001). Improvements of the patients of Group-A was significantly better than that of the patients of Group-B.
No Cases of soft or hard tissue infection found and no cases of hardwire hazard or plate exposure reported up to 90th postoperative day.
4. Discussion
The use of internal fixation in Oral and Maxillofacial Surgery has become widely utilized treatment protocol. Miniplate oesteosynthesis is a standard method for surgical treatment of mandibular fractures since 1980’s. Miniplates provide functionally stable fixation unlike rigid fixation that prevent micro motion of bony fragment under function. Functionally stable fixation applies to internal fixator that allows bone alignment and permit healing during function [12]. Now in the recent era, the development of locking miniplates (LMP) have theoretical advantage over the conventional or non-locking miniplates (NLMP) and those are described in the review of this present study. LMP utilize double threaded screws, which lock to the bone and the plate, creating mini-internal fixator. This results in a more rigid construction with less distortion of fracture [7, 12, 13].
Various studies and meta-analysis were published in last 3 decades regarding the controversy of locking miniplate vs non-locking miniplate but more of them have talked about the biomechanical functions, technical applications, histological compatibility and some clinical findings also, very little focus was given upon the radiological evaluation till date.
The aims and objectives of this study was to evaluate the efficiency of locking miniplates keeping in mind about the mandibular parasymphysis fracture, it’s complications and oesteosynthesis. Operating time has immense influence in the postoperative outcomes after any surgery. Regarding these two methods of fixation there are conflicting views in literatures in respect to operating time. Sebastian Sauerbier et al. in their study found decreased operative time in locking miniplate system in their study. The human mandible shows an uneven surface, adapting conventional miniplates to the contours of the bone can compensate for such incongruities [2]. Repeated bending may cause material fatigue and create predetermined breaking points [2]. Moreover, inaccurate adaptation of conventional plates causes displacement of the mobile bony fragments when the screws are tightened and can decrease primary stability. In contrast, the fixator-principle allows the mobile fragments of the bone to stay in the reduced position when tightening the screws, even if the plate is not precisely adapted. Therefore, exact plate adaptation is no longer necessary which should shorten operation times [2]. This was also supported by Ellis [12]. In contrast to this V. Singh et al. [7] stated that plate bending might be less precise with locking system but screw placement was not because of the use of drill guide to make more centralized hole for proper engage of the screw threads. Two years later Kumar et al. [3] opined that exact plate adaptation for locking plates is no longer necessary which should shorten operation times. Champy’s mini plate required higher time because these are linear plates and two plates are required for fixation at parasymphysis or symphysis region. Since the plate did not have to be as precisely adapted to the underlying bone and indeed did not have to be compressed against the bone for stability, the bending of plates was simplified [3].
Keeping this controversy in literature in mind, in this present study we evaluated the times taken for each steps of surgery. This was done so as to detect any bias regarding incision to exposure of fracture site which could depend on the amount of overlying soft tissues, the difficulty experienced at the reduction of the fracture segments - both of which are variables. It was seen that in the present study there was no significant differences between the groups as far as the time taken from incision to exposure and reduction were compared. On critically evaluating the time taken for fixation of the fractures either with LMP or NLMP, no significant variation existed which indicates that the time taken in LMP for a basic adaptation and specific drilling of holes so as to attain a lock did not result in prolonged operating time. This is in accordance with some of the above-mentioned studies probably because the time taken for adaptation of locking plates were less which in turn makes up for the time lost in using drill guides when compared to the precise adaptation required for NLMP.
The postoperative pain and swelling in the present study exhibited a definite pattern which was in accordance with any surgical procedures. When both the groups were evaluated there was no significant difference with two types of fixation in all the fracture sites. The pattern of increase and decrease of pain and swelling were similar to other studies in respect to fixation of mandibular fractures. This indicates that pain and swelling did not depend on the method of fixation [3-5, 14]. Kumar et al. [3] compared 20 patients from each group and it showed no such changes in postoperative pain in between two plating system group and it is also in accordance to this study. Agarwal et al. [14] in their study “Prospective randomized clinical trial comparing bite force in 2mm locking plates versus 2 mm standard plates in treatment of mandibular fracture” showed significant increase in swelling up to 1st week and 3rd week and then it had been reduced at 6 week and 3rd month but they also did not find any differences in two categories of plating system which is in accordance with this study.
Mobility of the fracture segments denotes the stages of soft callus formation and conversion of the same; keeping this in mind mobility of fracture segment in the parasymphysis and body region were measured in this study. The present study showed mobility of the fracture segments at the 14th day after ORIF in case of one patient in NLMP. Except this no other patients from both the groups showed any mobility of fracture segment at 14th Postoperative day. Vasistha et al. [5] in their study regarding two miniplate system at the parasymphysis region found that there was no mobility of fracture segment at the parasymphysis region at 3rd month postoperatively which is in accordance with this study.
The success of achieving occlusion and restoration of primary functions are heavily linked with the reduction of the fracture segments and internal fixation. Saikrishna et al. and V. Singh et al. [6, 7]. Analyzing the result, it was found that occlusal discrepancy were corrected in both the groups after 14 days of ORIF. When self-evaluation of chewing was documented it was noted that the patients from both the groups were able to have normal diet at the 3rd month postop except 1 patient who was in soft diet. To correct the early occlusal disharmony V. Singh et al used MMF at early postoperative days. Shasik et al [11], did the same study and also used guiding elastics upto 14 days to correct any occlusal disharmony in early postoperative days as we did in our setup also.
When both the groups were compared, no statistical significance found in between these two groups was achieved. While Nayak et al. reported occlusal discrepancy in 8% and 28% of their patients treated with locking plate and non-locking plate respectively. According to above-mentioned authors, reason for this might be that the inaccurate adaptation of conventional miniplates causes displacement of mobile bony fragments when the screws are tightened and thus can decrease primary stability resulting in occlusal discrepancy; in contrast, locking plate principle allows the mobile fragments of bone to stay in reduced position, even if plate is not precisely adapted and findings of this study revealed that even a single miniplate is enough to meet the criteria of anterior mandibular fixation in terms of occlusal harmony [5].
Analysing the results after ct and opg evaluation it was seen that both the method of fixation provided significant bony healing at the 3rd month postop. However critical evaluation of the results elicited some interesting results –
- The width of the fracture at the superior border in the buccal as well as at the lingual cortex were significantly more in LMP at preop while at the 3rd post op month there was no difference in both the cortices.
- The same pattern was observed when HFU was evaluated between the groups at the superior border.
- No difference in the width of the fracture at the inferior border in both the groups at both time periods.
- However the HFU at the inferior border there were no significant differences between the groups at 3rd month postop, even though preoperatively there was a significantly less HFU in LMP.
- When the HFU of the medullary bone were analysed it was observed that even though it was significantly lesser in LMP at the preop phase, it was significantly higher in the postop phase.
This finding suggests that a stability following reduction and fixation was much better in LMP due to which the rate of progression of bony healing was much higher. On review of literature it was seen that no consensus has yet been achieved. There are published studies showing increased stability after ORIF done by LMP.
According to Haug et al. [1] the stability of conventional bone plating systems is achieved when the head of the screw compresses the fixation plate to the bone as the screw is tightened. Invariably over a period of time, the cortex of bone adjacent to the plate will resorb. If the plate is not contoured precisely and is not in intimate contact with the bone or if the host is compromised (medically or nutritionally), the ‘‘race’’ between fracture healing and cortex resorption will be lost and will result in unstable fixation. And on the other hand just a year later Gutwald et al. [20] stated that the problem addressed by Haug et al had been overcome by the development of a screw which locks not only to the bone but to the bone plate i.e. locking plate/screw system. This was accomplished by having a screw with a double thread. One thread would engage the bone; another engage a threaded area of the bone plate. The result is a locking plate system which in effect provides a mini-internal fixation. Since the plate locks to the screw rather than gaining its rigidity by being compressed against the bone, it also avoided the cortical necrosis which is sometimes seen under a plate which is compressed against the bone. The locking design in the plate prevents screw migration out of bone by maintaining screw plate integrity, creating a more rigid system and potentially improved plate performance [1, 12, 15]. V. Singh et al. [7] concluded that the locking mini plates gives the advantage of greater stability than non locking miniplates which is in accordance to our study.
Agarwal et al. [14] in his study measured occlusal load at different time intervals at the incisor region and concluded that the use of locking miniplates plate in mandibular fracture was efficacious enough to bear the masticatory loads during osteosynthesis of the fracture which in turn supports the increase in stability in LMP system. According to Kumar et al. [16] the theory of the locking screw plate system is that the integration of screw and plate will allow for more rigidity in the plating system. Ellis and Graham also supported this and they recommended no MMF postoperatively. Kumar also stated that due to this advantage of locking plates help in early restoration of function also.
About two years later B.R Chrcanovic [15] in his meta-analysis pointed that if the non-locking implant is not perfectly moulded to the anatomy of the subjacent bone, primary loss of reduction occurs because of the traction of the screw on the bone needed for securing it to the Plate. Without this intimate contact, tightening of the screws will draw the bone segments towards the plate, resulting in alterations in the position of the osseous segments and the occlusal relationship. Moreover, that secondary loss of reduction is also more frequent in non-locking systems, as the resulting loading forces and micro-movements may lead to loosening of the screws and instability. In both cases the consequence tends to be malocclusion. In the locking system, as the screws are tightened, they ‘lock’ to the plate, thus stabilizing the segments without the need to compress the bone to the plate. Here theoretically, the stability should be more in case of locking plates.
NLMP mainly stabilizes the fracture segments by frictional lock of the screws with the bone and on the other hand LMP acts a single unit which comprises with bone, plate and screws from this point of view theoretically LMP provides more stability under 3 types of forces as described (Ellis III and Graham; 2002); practically this is being reflected in this present study. In contradiction, Kumar et al. [16] did not find any significant differences in between two groups regarding stability. This is also supported by Shaik et al. [11].
However among the recent studies, in the year 2016, Vashistha et al. [5] compared two plating system in 40 patients, 20 patients in each group and concluded that even single LMP in the interforaminal fracture provide equal good stability and early restoration of function in comparison with 2 conventional miniplate fixation.
In present study, however, it was found that LMP executed a better healing of fracture site. Review of literature reveals that in vivo healing of fracture sites were mainly assessed by either clinical examination or conventional radiographs. Very few studies are available in the literature where CT scans were done for evaluation of bony healing [17, 18]. Thus, method of postop parameters to critically evaluate bony healing is still lacking in literatures. Definite conclusion can’t be reached due to the fact, that the sample size was small and more importantly the fractures were not classified according to the type of displacement and evaluated accordingly.
Postoperative complications like soft tissue and bone infections were found at 1st, 2nd and 3rd month and no hardwire hazards and plate exposure were observed at 3rd month. According to Gutwald and Ellis loosening of screw and plates are considered to be one of the main risk of increased infection rates which is quite often encountered with nonlocking system theoretically [12, 19], but not found in locking system because it acts as a single unit with the bone after fixation [20]. Sauebier et al. [2] in his study found good results from the locking 2.0 system with only 1.9% of major complications and loosening of only one screw, discovered during plate removal. Provided the locking 2.0 plates are inserted correctly, risk of screw loosening is minimal. In conventional systems with similar dimensions, fixation is provided by the screw thread inserted into the bone, creating a friction lock between the plate and the bone which is essential to achieve stability after the reduction. Torsional forces between the bony fragments may lead to a loss of this friction lock and result in reduced primary stability. According to Kumar et al. [3] in their study regarding comparative evaluation in between two planning system there was no such significant complication rate found in between two plating system which is in accordance to this study. B. R. Chrcanovic [15] in his meta-analysis did not find any significant difference regarding the complication rate in between two plating system which is in accordance to this study. Vasistha et al. [5] did not find any difference regarding loosening of screw and plate exposure or fractures in between both the plating system placed in the parasymphysis region which is also in accordance to our study.
5. Conclusion
We concluded that Locking miniplates are technically not cumbersome than non-locking one – No significant increase in operating time. Use of two locking miniplates in the parasymphysis region placed on the Champy’s line of oesteosynthesis provides a better stability and oesteosynthesis at the 3 months postoperative period than non-locking. Due to the diverse variation in biomechanics of mandibular parasymphysis fractures based on various classification and number of fractures a more detailed study with a large number of a sample size along with the objective assessment of the degree of displacement should be included in a study to assess the viability or efficacy of locking miniplates as a treatment option for mandibular fractures.
References
- Richard H Haug, Street Goltz. Does plate adaptation affect stability? A biochemical comparison of locking and non-locking plates. American Association of Oral and Maxillofacial Surgeon 60 (2002): 1319-1326.
- Sebastian Sauerbier, Jana Kuenz, Silke Hauptmann, et al. Clinical aspects of a 2.0-mm locking plate system for mandibular fracture surgery. Journal of Cranio-Maxillo-facial Surgery (2010): 1-4.
- Kumar I, Bajaj A. Comparative evaluation of 2.0-mm locking plate system vs. 2.0-mm nonlocking plate system for mandibular fractures—a retrospective study. Oral Maxillofac Surg 17 (2013): 287-291.
- Arjun Sungh KV, Arunkumar. Standard 3D Titanium Miniplate Versus Locking 3D Miniplate in Fracture of Mandible: A Prospective Comparative Study: Journal of Maxillofacial and Oral Surgery 15 (2015).
- Arpit Vashistha, Manpreet Singh, Manoj Chaudhary, et al. Comparison of 2 mm single locking miniplates versus 2 mm two non-locking miniplates in symphysis and parasymphysis fracture of mandible. JOBCR 7 (2017): 42-48.
- Saikrishna D, Shetty SK, Marimallappa TR. A comparison between 2.0-mm standard and 2.0-mm locking miniplates in the management of mandibular fractures. J Maxillofac Oral Surg 8 (2009): 145-149.
- Singh V, Kumar I, Bhagol A. Comparative evaluation of 2.0-mm locking plate system vs 2.0-mm nonlocking plate system for mandibular fracture: a prospective randomized study. Int J Oral Maxillofac Surg 40 (2011): 372-377.
- Marthinus J Kotze, Kurt-W Bütow, Steve A Olorunju, et al. A comparison of mandibular and maxillary alveolar osteogenesis over six weeks: a radiological examination. Head & Face Medicine 14 (2014): 10-50.
- Jain MK, Sankar K, Ramesh C, et al. Management of mandibular interforaminal fractures using 3 dimensional locking and standard titanium miniplates-a compara- tive preliminary report of 10 cases. J Craniomaxillofac Surg 40 (2012): e475-e478.
- Pavan Kumar B, Jeevan Kumar KA, Venkatesh V, et al. Study of Efficacy and the Comparison Between 2.0 mm Locking Plating System and 2.0 mm Standard Plating System in Mandibular Fractures J. Maxillofac. Oral JOMS. Surg 14 (2015): 799-807.
- Mahaboob Shaik T, Subba Raju N, Koteswara Rao, et al. Effectiveness of 2.0 mm Standard and 2.0 mm Locking Miniplates in Management of Mandibular Fractures: A Clinical Comparative Study. Journal of Maxillofacial and Oral Surgery 13 (2014): 47-52.
- Edward Ellis III, John Graham. Use of a 2.0-mm Locking Plate/Screw System for Mandibular Fracture Surgery J Oral Maxillofac Surg 60 (2002): 642-645.
- Ribeiro-Junior PD, Magro-Filho O, Shastri KA, et al. In vitro evaluation of conventional and locking miniplate/screw systems for the treatment of mandibular angle fractures. Int. J. Oral Maxillofac. Surg 39 (2010): 1109-1114.
- Agarwal M, Mohammad S, Singh RK, et al. Prospective randomized clinical trial comparing bite force in 2-mm locking plates versus 2-mm standard plates in treatment of mandibular fractures. J Oral Maxillofac Surg 69 (2011): 1995-2000.
- Chrcanovic BR. Locking versus non-locking plate fixation in the management of mandibular fractures: a meta-analysis. Int. J. Oral Maxillofac. Surg 43 (2014): 1243-1250.
- Kumar I, Singh V, Bhagol A, et al. Supplemental maxillomandibular fixation with miniplate osteosynthesis-required or not? Oral Maxillofac Surg 15 (2011): 27-30.
- White SC, Pharaoh MJ. Oral radiology: Principles and Interpretation, 6th Edition, ISBN: 978-0-323-04983-2.
- Nathan R Hendrickson, Perry J Pickhardt, Alejandro Munoz del Rio, et al. Bone Mineral Density T-Scores Derived from CT Attenuation Numbers (Hounsfield Units): Clinical Utility and Correlation with Dual-energy X-ray Absorptiometry. Iowa Orthop J 38 (2018): 25-31.
- Gutwald R. Biomechanical stability of an internal mini fixation system in maxillofacial oesteosynthesis . J Med Bio Eng Comp 37 (1999): 280-281.
- Gutwald R, Alpert B, Schmelzeisen R. Principle and stability of locking plates. Keio J Med 52 (2003): 21-24.
