Community Based Non Communicable Disease Services as a Predictor of Improved Quality of Life of People Living with HIV in Uganda: A Randomized Controlled Trial
Article Information
Christopher Ddamulira*, Norman Nsereko, Miph Musoke, Frank Pio Kiyingi
School of Post Graduate Studies and Research, Nkumba University, Entebbe, Uganda
*Corresponding Author: Christopher Ddamulira, School of Post Graduate Studies and Research, Nkumba University, and P.O. Box 237, Entebbe, Uganda
Received: 22 September 2020; Accepted: 01 October 2020; Published: 13 October 2020
Citation:
Christopher Ddamulira, Norman Nsereko, Miph Musoke, Frank Pio Kiyingi. Community Based Non Communicable Disease Services as a Predictor of Improved Quality of Life of People Living with HIV in Uganda: A Randomized Controlled Trial. Journal of Environmental Science and Public Health 4 (2020): 304-317.
View / Download Pdf Share at FacebookAbstract
A comprehensive and culturally applicable community based Non Communicable Diseases (NCD) services package was implemented with an aim to test the effectiveness of the community based NCD services on the quality of life (QoL) of people with HIV. The Randomized Controlled Trial (RCT) was conducted to compare the effectiveness of the community based NCD services as intervention. The control group received the usual HIV services in the community. Participants were randomly allocated to receive weekly and monthly intervention sessions using the standard care in the community ARV drug distribution points. Paired and independent t-tests were performed to compare changes in the QoL scores at the baseline and the endline. Between November and December 2018, 1076 individuals were screened, of whom 438 were randomly assigned to either the intervention or control group in the ratio of 1:1. The post intervention results revealed that the community based NCD services were effective and improved the QoL in all the three domains; the physical, environmental and social relationship domains. The QoL was higher at endline across all domains in the treatment group compared to the control group, the mean differences were statistically significant (p = 0.000 < 0.05). Thus, the community based NCD services were efficacious in improving QoL of HIV infected people. Findings could be utilized at regular community service settings for its sustainability and long-term effect. The intervention created improved understanding of HIV and NCD integration health promotion strategies and community support systems activities by the VHT, ART expert clients and the community volunteers.
Keywords
Community, Non Communicable Diseases, Services, Quality of Life, HIV, People Living with HIV, Uganda
Community articles; Non Communicable Diseases articles; Services articles; Quality of Life articles; HIV articles; People Living with HIV articles; Uganda
Community articles Community Research articles Community review articles Community PubMed articles Community PubMed Central articles Community 2023 articles Community 2024 articles Community Scopus articles Community impact factor journals Community Scopus journals Community PubMed journals Community medical journals Community free journals Community best journals Community top journals Community free medical journals Community famous journals Community Google Scholar indexed journals Non Communicable Diseases articles Non Communicable Diseases Research articles Non Communicable Diseases review articles Non Communicable Diseases PubMed articles Non Communicable Diseases PubMed Central articles Non Communicable Diseases 2023 articles Non Communicable Diseases 2024 articles Non Communicable Diseases Scopus articles Non Communicable Diseases impact factor journals Non Communicable Diseases Scopus journals Non Communicable Diseases PubMed journals Non Communicable Diseases medical journals Non Communicable Diseases free journals Non Communicable Diseases best journals Non Communicable Diseases top journals Non Communicable Diseases free medical journals Non Communicable Diseases famous journals Non Communicable Diseases Google Scholar indexed journals Quality of Life articles Quality of Life Research articles Quality of Life review articles Quality of Life PubMed articles Quality of Life PubMed Central articles Quality of Life 2023 articles Quality of Life 2024 articles Quality of Life Scopus articles Quality of Life impact factor journals Quality of Life Scopus journals Quality of Life PubMed journals Quality of Life medical journals Quality of Life free journals Quality of Life best journals Quality of Life top journals Quality of Life free medical journals Quality of Life famous journals Quality of Life Google Scholar indexed journals HIV articles HIV Research articles HIV review articles HIV PubMed articles HIV PubMed Central articles HIV 2023 articles HIV 2024 articles HIV Scopus articles HIV impact factor journals HIV Scopus journals HIV PubMed journals HIV medical journals HIV free journals HIV best journals HIV top journals HIV free medical journals HIV famous journals HIV Google Scholar indexed journals People Living with HIV articles People Living with HIV Research articles People Living with HIV review articles People Living with HIV PubMed articles People Living with HIV PubMed Central articles People Living with HIV 2023 articles People Living with HIV 2024 articles People Living with HIV Scopus articles People Living with HIV impact factor journals People Living with HIV Scopus journals People Living with HIV PubMed journals People Living with HIV medical journals People Living with HIV free journals People Living with HIV best journals People Living with HIV top journals People Living with HIV free medical journals People Living with HIV famous journals People Living with HIV Google Scholar indexed journals NCD articles NCD Research articles NCD review articles NCD PubMed articles NCD PubMed Central articles NCD 2023 articles NCD 2024 articles NCD Scopus articles NCD impact factor journals NCD Scopus journals NCD PubMed journals NCD medical journals NCD free journals NCD best journals NCD top journals NCD free medical journals NCD famous journals NCD Google Scholar indexed journals drug articles drug Research articles drug review articles drug PubMed articles drug PubMed Central articles drug 2023 articles drug 2024 articles drug Scopus articles drug impact factor journals drug Scopus journals drug PubMed journals drug medical journals drug free journals drug best journals drug top journals drug free medical journals drug famous journals drug Google Scholar indexed journals Disease articles Disease Research articles Disease review articles Disease PubMed articles Disease PubMed Central articles Disease 2023 articles Disease 2024 articles Disease Scopus articles Disease impact factor journals Disease Scopus journals Disease PubMed journals Disease medical journals Disease free journals Disease best journals Disease top journals Disease free medical journals Disease famous journals Disease Google Scholar indexed journals
Article Details
1. Introduction
There was an indication in 2012 that Non-Communicable Diseases (NCDs) were responsible for 38 million (68%) of the world’s 56 million deaths [1]. Almost three quarters of all NCD (28 million) and the majority of premature deaths (82%) occur in low and middle income countries mainly in Asia and Sub-Saharan African (SSA) countries [1] . Yet, the published evidence showed that, the current community service delivery models of ART according to Grismund [2] “do not include the integrated community management and prevention of Diabetes Mellitus(DM) and hypertension as co-morbidities in SSA” (pg. 4). The lack of the NCD services affects the prevention programmes for the co-morbidities among the HIV patients receiving Anti-Retroviral Therapy (ART) in the communities.
Globally, deaths from NCDs are projected to reach 52 million by 2030 [3]. The deaths related to hypertension and diabetes among HIV patients on Antiretroviral Therapy (ART) increased due to scale up of the treatment and aging with HIV [4]. Most deaths occurred among HIV people with Hypertension (HT) and Diabetes Mellitus (DM) conditions that needs daily medication and or to make life style changes to ensure they can live as well as possible with their condition [1]. Therefore, the individual and family support systems are important in reducing the burden of HIV and NCDs.
Sub-Saharan Africa has undergone epidemiological transitions that included an epidemic of Non-Communicable Diseases (NCDs) with an estimated prevalence of hypertension of 26.5% and 12.6% for Diabetes Mellitus in South, Central and East African regions [5, 6]. The prevalence of hypertension and diabetes among adult people living with HIV (PLHIV) in Uganda is increasing with an estimated prevalence of hypertension of 20.9% and 10.4% for diabetes [7, 5]. Thus, understanding the strategies for early detection and treatment would be important for improving health services and the quality of life of HIV patients.
Uganda like other sub-Saharan African countries now faces the double burden of HIV and Non-Communicable Diseases due to the profound effects HIV, ART and the growing population of people aging with HIV [ 8, 7]. With a prevalence of hypertension and Diabetes Mellitus of 28.7% and 20.9% respectively among HIV patients on ART in Uganda [7], the country has approximately two hundred fifty thousand people with a double burden of HIV and NCD. The Ministry of Health [9] recognized that Non-communicable diseases (NCDs) and their risk factors were increasing in Uganda among patients with HIV on Anti-Retroviral Therapy (ART).
As the patients enrolled on Anti-Retroviral Therapy (ART) to improve their survival, the risks of NCDs were reported to have increased with patient’s duration on anti-retroviral therapy and chronological age [4]. Therefore, People Living with HIV (PLHIV) on ART represents a group in which prevention, screening and treatment strategies using community approach offers substantial benefits to reduce Diabetes Mellitus (DM) and hypertension co-morbidities among patients [10]. This calls for a community intervention for the early screening of NCD’s among PLHIV on ART in order to reduce morbidity and mortality that could rise as result of co-burden of HIV and NCD’s, mainly DM and hypertension.
The design of service delivery models for PLHIV must also address co-morbidities and co-infections [11]. With an aging population of PLHIV and a burgeoning epidemic of chronic diseases, services must incorporate treatment and prevention for non-communicable diseases. The scale up of ART for people living with HIV in low- and middle-income countries has been associated with huge individual benefits and rising life expectancies [12, 13]. However, the expanded access to ART has also resulted in a new global health challenge, namely, increased co-morbidity of Non-Communicable Diseases in those living and aging with HIV on ART [14, 15].
The health and improved QoL gains made against HIV and AIDS are now under threat from hypertension and diabetes problems which are increasingly prevalent and documented among the HIV positive [16]. For example, according to Triant et al. [17], DM and hypertension diseases emerged as the leading cause of morbidity and mortality in HIV infected persons on Anti-Retroviral Therapy (ART) in developed country settings. According to Kavishe et al. [18], there is a high prevalence of NCD risk factors and unrecognized and untreated hypertension represent major problem in Uganda. The high prevalence of Diabetes Mellitus (DM) and other preventable NCDs provides an opportunity for prevention.
It is well established that Hypertension and Diabetes Mellitus all have direct and indirect relationships with HIV and ART. Similarly, certain ART drugs contribute to NCDs complications through hypercholesterolemia, increased abdominal fat and the metabolic syndrome [14]. People living with HIV, whether they have been initiated on ART or not, there is chronic activation of the innate immune system with excessive production of inflammatory cytokines and mediators that in turn are associated with an increased risk of atherosclerosis, coronary artery inflammation and all-cause mortality [19, 20]. Therefore, the integrated community based HIV and NCD services are important in the monitoring and prevention of the ART related drug toxicities among patients in the community at an earlier opportunity, if implemented by the Ministry of Health (MOH).
In Uganda, major efforts are needed to strengthen health services for the prevention, early detection and treatment of chronic diseases [18]. There are many lessons from the HIV experience that are applicable to the NCD movement. These lessons included shifting tasks between cadres of Health Care Workers (HCW) that include the expert ART clients, VHTs and the community volunteers, to develop robust clinical monitoring and evaluation programs that provide patient-centered care and medication adherence support to patients [21].
The Non-Communicable Diseases such as DM and hypertension have been integrated into routine HIV services at all government health facilities at facility level [22]. However, integration of NCD services are still lacking in the Community Drug Distribution Points [22]. Furthermore, the existing strategies for integration of HIV services in the community with other diseases in Uganda have focused mainly on tuberculosis (TB), malaria, reproductive health and other sexually transmitted infections [22]. Non-communicable diseases such as hypertension, diabetes mellitus, cancer have not received the attention they disserve for prevention and management in the communities [23], Hence, this called for the development of innovative integrated care model that incorporates the NCDs component in the routine community HIV care, management and prevention, which is lacking in all community models where expert clients are utilized as lay health workers for service delivery.
Furthermore, 70% of the patients on ART in Uganda, receive ARVs from the community drug distribution points among the various clinics for the non-government organizations and public health facilities [24]. Therefore, integrating the NCD intervention within the current ART service structures was necessary in the Uganda to improve the quality of life of PLHIV with NCDs. Secondly, in the rural areas, the long distance to clinics can be a barrier to the access and adherence of patients on ART with NCDs in the District especially if the services are only centered at the public health facilities [24].
Quality of Life (QoL) of people living with HIV increased due to the availability of ART and access to early HIV diagnosis [25]. People living with HIV in Uganda and other Sub-Saharan African countries enjoyed the same life expectancy and QoL as the general population [26]. The transformation of HIV into a chronic condition through the immunological effectiveness of the treatment, health-related quality of life (HRQoL) became an important focus for HIV care [27]. Therefore, ART as treatment in the studies reviewed improved the physical quality of life of patients.
People Living with HIV (PLHIV) have endured the HIV and AIDS epidemic for decades, studies have been carried out to examine the effects of the disease on the quality of life (QoL) of people affected by the disease [28]. Consequently, the expansion of ART treatment and the decline in opportunistic infections resulted into increased survival rates and disease chronicity [29]. Antiretroviral Therapy (ART) and aging with HIV are risk factors associated with Non Communicable Diseases (NCDs) that affects the quality of life of patients [29]. Thus, according to Gaspar et al. [30] , understanding the effects of community based NCD services and the QoL among patients has become one of the main objectives of HIV and AIDS research.
Chronicity of AIDS was a landmark in improving the living conditions of people living with PLHIV [31]. The increase in the time of living with HIV allowed infected individuals a greater possibility of acceptance, adaptation and conformation with the disease, and thus, it was important to analyze strategies to improve the QoL of PLHIV [32]. The analysis of the community based NCD services as predictor of quality of life, informed policies and procedures to improve the physical health, enviromemental wellbeing and social relationship quality of life.
With the increase QoL as result of ART, people started to have a longer survival, which allowed the aging of PLHIV [25], thus, of the 36.7 million people living in 2015 with HIV and AIDS, 5.8 million were 50 years or older [28]. However, the likelihood of a longer life is not always related to good quality of life due to co-burden of diseases related to NCDs, such as hypertension and Diabetes Mellitus [31]. The quality of life can be affected by several factors, such as level of education, age, gender, individual life styles, marital status and health services utilization [33]. Therefore, designing health services related to NCD services may impact the physical health, environmental wellbeing and social relationship domains of the quality of life.
The pursuit for QoL does not only end with the extension of the years of life, taking into account the meaning of living with HIV and NCDs, which can characterize the problems associated with the multi-comorbidities and lack of adequate health services in resource limited settings, which may compromise the physical well-being, environmental well-being and social relationships quality of life of individuals living with HIV and NCDs, especially those aged 40 or over [31].
The existing evidence indicated that there was burden of Non Communicable Diseases (NCDs) among HIV patients on the Anti-Retroviral Therapy in Uganda [7, 5]. Therefore, it is necessary to note that the community based NCD services as a precursor and effective pointer to improved quality of life of patients receiving ART services in the communities [34]. Thus, the study intended to examine the effectiveness of the community based NCD services and quality of life of people living with HIV.
2. Materials and Methods
The study used a randomized controlled trial design to determine the effectiveness of community based NCD services on the quality of life of people with NCDs living with HIV. The study was guided by the Consolidated Standards of Reporting Trials (CONSORT) guidelines as shown in (Figure 1) [35].
The study was conducted in Wakiso District located in central Uganda, sample size was determined using Chan [36] method for designing experimental research using randomized controlled trial for detecting a significance difference in the group that received NCD services (Intention to Treat) and the control group that received treatment as usual (TAU). The number of subjects per group for a two-sided significance level, using 5% and a power of 95% and effect size of 0.3 was determined.
A total of 438 HIV patients with NCDs (Diabetes or Hypertension) receiving the chronic care from the Community Drug Distribution Points (CDDP’s) in Wakiso District were enrolled in the study randomly in the in a 1:1 ratio between the treatment (219) and the control groups (219). The unit of analysis was at individual level. Formally consent was sought from all eligible HIV participants aged 18 years and above receiving ART services in the communities.
The intervention group received information on NCD risk factors, health promotion and risk reduction, early detection and screening of NCD risk factors, referral for the treatment of hypertension and diabetes, ART treatment, behavioral change counselling, social support, treatment adherence, routine monitoring for blood pressure, blood sugars, viral load tests and referral for rehabilitation and psychosocial support with the aim of improving the quality of life.
Data was collected using standardized WHO Quality of Life (QoL) structured questionnaire [37] at baseline and endline after 12 months of the intervention. In the intervention group, community based NCD services were provided every month in the respective sub counties at the CDDPs or during the group meetings of the clients. The intervention and control participants were separated by a distance of at least 40 kilometers from one another, to try minimize contamination. Participant flow is shown in (Figure 1) below. The data was analyzed using SPSS Version 20 to generate descriptive and inferential statistics.
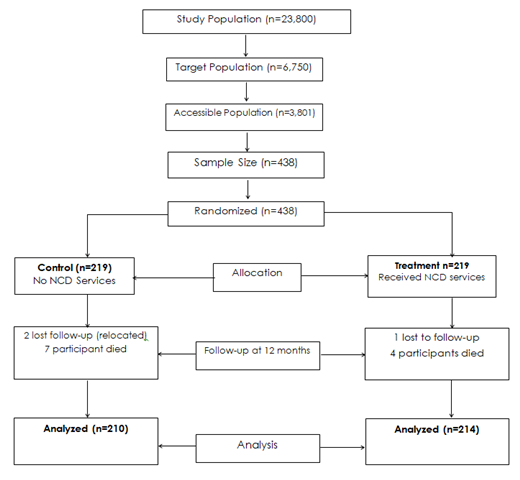
Figure 1: Consolidated Standard Reporting for Randomized Control Trial (RCT); Source [35].
3. Results of the Study
3.1 Baseline results of the study
|
Demographics |
Treatment N(%) |
Control N(%) |
χ2 |
P-value |
||
|
Gender |
||||||
|
|
Male |
97(44.3) |
78(35.6) |
3.435 |
0.064 |
|
|
|
Female |
122(55.7) |
141(64.4) |
- |
- |
|
|
Age |
||||||
|
|
Less than 40 years |
3(1.4) |
3(1.4) |
- |
1.000 |
|
|
|
40 years and above |
216(98.6) |
216(98.6) |
- |
- |
|
|
Education Level |
||||||
|
|
|
158(72.1) |
168(76.7) |
1.200 |
0.273 |
|
|
|
Secondary and above |
61(27.9) |
51(23.3) |
- |
- |
|
|
Marital Status |
||||||
|
|
Married |
126(57.5) |
139(63.5) |
1.615 |
0.204 |
|
|
|
Unmarried |
93(42.5) |
80(36.5) |
- |
- |
|
|
a Comparison between treatment and comparison groups |
||||||
**Significant at 5% level; Source: Primary data, 2019.
Table 1: Patients demographic characteristics.
The majority of the respondents were female, 55.7% in the treatment and 64.4% in the control group. The majority of the respondents were 40 years and above both in the treatment and the control group (98.6% respectively). According to the level of education, majority of the respondents in both the control and treatment were below the secondary level, 72.1% in the treatment and 76.7 in the control group. The findings showed that the majority of the respondents were married both in the treatment and control groups (57.5% and 63.5% respectively). The socio- demographic characteristics of the respondents did not significant vary at baseline both in the control and the intervention group. All the variables were statistically not significant (p> 0.005). Therefore, there was homogenicity in terms of the individual characteristics of the respondents before the implementation of the community based NCD services within the treatment group.
3.2 End of intervention results of the study
In the study, there was a significant mean differences (p < 0.05) in the rating scores by the general quality of life (1.80), physical health (1.43), environmental domain (1.66) and, social relationship (1.60) after the implementation of the community based NCD services. In summary, the mean general quality of life within the intervention group was higher in the endline (4.21) compared to the baseline (2.41) which difference was statistically significant (p = 0.000 < 0.05).
|
Variables |
Mean (n = 433) |
Mean difference |
tα |
p-value |
|
|
Intervention group |
|||||
|
Baseline |
Endline |
||||
|
General quality of life |
2.41 |
4.21 |
1.8 |
25.9 |
0.000* |
|
Physical health |
2.49 |
3.92 |
1.43 |
23.34 |
0.000* |
|
Environmental domain |
2.11 |
3.77 |
1.66 |
26.08 |
0.000* |
|
Social relationship |
2.21 |
3.81 |
1.60 |
26.1 |
0.000* |
Mean Range Scale: 1.00-1.79= Very Poor, 1.80-2.59= Poor, 2.60-3.39= Fair, 3.40-4.19=Good, 4.20-5.00= Very Good; *Significant at p < 0.05; Source: Primary data, 2019.
Table 2: Paired t-test results for quality of life for the intervention group at baseline and endline.
It implied that when the study participants adopted the community based NCD messages from the VHTs, expert clients and the community volunteers, they experienced an improvement in the overall quality of life. This means that the NCD services had the efficacy in improving the QoL of the study participants. Therefore, the services could be generalised and implemented in other settings for the prevention and control of the NCDs among the people living with HIV and AIDS.
|
Variables |
Mean (n = 429) |
Mean difference |
tα |
p-value |
|
|
Control group |
|||||
|
Baseline |
Endline |
||||
|
General quality of life |
2.43 |
2.46 |
0.03 |
0.49 |
0.829 |
|
Physical health |
2.5 |
2.53 |
0.03 |
1.26 |
0.847 |
|
Environmental domain |
2.11 |
2.15 |
0.04 |
0.82 |
0.950 |
|
Social relationship |
2.23 |
2.23 |
0.00 |
0.82 |
0.845 |
Mean Range Scale: 1.00-1.79= Very Poor, 1.80-2.59= Poor, 2.60-3.39= Fair, 3.40-4.19= Good, 4.20-5.00= Very Good; * Highly significant at p < 0.05; Source: Primary data, 2019.
Table 3: Paired t-test results for quality of life (QoL) for the control group at baseline and endline.
In the study, there was no significant mean differences (p=>0.05) in the rating scores by the general quality of life (0.03), physical health (0.03), environmental domain (0.04) and, social relationship (0.00). Note that in the control group, there was no provision of community based NCD services. This means that if NCD services were implemented, would have improved the QoL of people in the control group. The implication of the findings indicates that, if the NCD services are not provided to the HIV patients with NCDs, their QoL would be compromised.
|
Domain |
Treatment |
Control Mean Difference |
tα |
p-value |
|
General Quality of Life |
4.21 |
2.46 1.75 |
21.82 |
0.000* |
|
Physical Health Domain |
3.92 |
2.53 1.39 |
18.22 |
0.000* |
|
Environmental Domain |
3.77 |
2.15 1.62 |
21.48 |
0.000* |
|
Social Relationship |
3.81 |
2.23 1.58 |
20.98 |
0.000* |
Mean Range Scale: 1.00-1.79= Very Poor, 1.80-2.59= Poor, 2.60-3.39= Fair, 3.40-4.19= Good, 4.20-5.00= Very Good, * Significant at p < 0.05; Source: Primary data, 2019.
Table 4: Independent t-test for the mean scores for the quality of life between the control and the intervention groups at endline.
The findings in Table 4, indicated a highly significant change in all the 4 sub-variables considered as a measure of the quality of life people with NCD living with HIV when the control and intervention groups were compared at the endline. In the study, there was a significant mean differences (p < 0.05) in the rating scores by the general quality of life (1.75), physical health (1.39), environmental domain (1.62) and, social relationship (1.58). The findings indicted that the participants in the intervention group improved the general QoL after the implementation of the community based NCD services compared to those in the control group, were there was no improvement in the QoL.
It implied that when the study participants in the intervention group adopted the community based NCD messages from the VHTs, expert clients and the community volunteers, they experienced an improvement in the overall quality of life. This means that the NCD services had the efficacy in improving the QoL of the study participants. Therefore, generalising and implementing the community based NCD services in other settings would be important in improving the quality of life of people with HIV living with NCDs.
4. Discussion
The significant change in the quality of life after the implementation of the community based NCD services implies that when the study participants adopted the messages from the VHTs, expert clients and the community volunteers through health promotion, community support systems and following the appointments for the monitoring scheduled visits for the blood sugar tests, Viral load and CD4 tests, blood pressure measurements etc.; they experienced an improvement in their general quality of life including the physical health , environmental and social relationship domains. For instance, there was a significant improvement in the mean general quality of life of (4.21) in the treatment group compared to the control group (2.15) at endline, which difference was statistically significant (p = 0.000 < 0.05).
It could be argued that the improvement in QoL was due the use of recommended VHTs, expert clients and community volunteers in passing on key messages on NCD risk factors, health promotion and risk reduction, early detection and screening of NCD risk factors, referral for the treatment of hypertension and diabetes, ART treatment, behavioral change counselling, social support, treatment adherence, routine monitoring for blood pressure, blood sugars, viral load tests and referral for rehabilitation and psychosocial support improved the patients practices on the HIV and NCD prevention and management. Therefore, the general improvement in the quality of life of people with NCDs living with HIV that participated in the trial. The improvement in the quality of life across all the domains in this study was due to the adoption the community based NCD services.
Therefore, the results of the study were consistent with earlier findings by UNAIDS [38] and Grimsrud [2], that coming up with integrated package to address HIV and NCD diseases in the community would improve the prevention and management of the co-morbidities, hence improving the overall quality of life of life people with NCD living with HIV. Bhatta and Liabsuetrakul [39] argued that the implementation of community integrated HIV-NCD interventions that included; the utilization of health promotion strategies, community support structures and patients monitoring systems on patients receiving ART from the communities improved the overall quality of life of people living with HIV and AIDS in Napel. Furthermore, the empowerment intervention using health promotional activities with the support of the community systems structures was efficacious in improving Quality of life of HIV infected people in Nepal [39]. Hence, such interventions for NCD services would be integrated in the routine services for HIV in the communities for improving the quality of life of people with HIV living with NCDs.
Similarly, the cohort study by Decroo et al. [40] on the effect of community support structures using community ART groups on retention-in-care among patients on ART in Tete Province, Mozambique. It was found out that the retention in care and better clinical outcomes were among patients in community ART groups compared to those who were receiving individual care from the facilities. The study confirms that patient-driven community HIV and NCD’s distribution groups through community support groups using lay cadres, such as; VHTs, expert clients and community volunteers would result into higher retention and better patient’s quality of life among patients who are on ART with NCDS in the communities were the Randomized Controlled Trial (RCT) was carried out.
Although the concept of integrated HIV-NCD intervention has been widely accepted in the hospitals in Uganda and in many western countries [41], there was no confirmation yet that the same level of success could be achieved if it is implemented by the lay health care workers in the communities like VHT, expert ART clients and Community volunteers. Hence, the novel findings by the trial have proved that the VHT, expert clients and community volunteers if trained, could actually work in the communities with the support and supervision of the professional health care workers to reduce the burden of NCDs among patients receiving chronic HIV care in the communities.
Training of the community volunteers in the NCD prevention and management skills as part of the routine package in home based care would improve preventive measures at the community and family level. Hence, improvement in the quality of life of patients with HIV and NCDs. It is now accepted that Human Resource for Health (HRH) is not only a strategic capital, but also the most important resource for the performance of the health system, the shortage of health workers has gravely implicated the quality delivere [42,43]. The World health Organization (WHO) has argued that the 4.3 million health workers shortage has brought to the attention of policy makers, the unequal distribution of health workers in places where there is critical need of health care, while scholars also believe that this shortage is a cause of heavy workload to those left behind who have to cover work for the required numbers to match the population [44, 42]. Hence, the findings have demonstrated that the VHTs, expert clients and community volunteers especially those who know how to read and write could be trained in the basic health promotion activities and skills for working with communities and become a part of the critical human resources for counselling and referral of patients to the health facilities. Hence, there is need to integrate the community NCD services package in the current VHT policy and strategy for the Ministry of Health (MOH).
Based on the findings of independent and paired t –test analyses, where all the sub variable of the quality of life of people with NCD living with HIV showed significant mean differences between the control and intervention at endline (p < 0.05). The null hypothesis was rejected and alternative accepted. Hence, according to data generated in the study, the quality of life among people with NCD living with HIV and AIDS significantly increased after the intervention of Non-Communicable Diseases (NCD) services. The study had a limitation that assessing the quality of life (QoL) was based on the patient’s perception using the WHO QoL instrument rather than the use of biomedical tests to determine the changes in the individual patients QoL.
5. Conclusion
In conclusion, rigorously designed intervention indicated that the community based NCD services (health promotion, community support systems and patient monitoring systems) increased QoL of HIV infected people receiving chronic care from the communities. Furthermore, it could be useful to reduce stigma and increase their social support network. Findings could be utilized at regular community service settings for its sustainability and long-term effect.
6. Recommendation
The study recommended, the Government through the Ministry of Health (MOH) to review and adopt the transformed community based HIV and NCD services in the national guidelines for management of HIV in the communities using the differentiated models.
Acknowledgements
The authors wish to thank School of Post Graduate Studies and Research, Nkumba University, Entebbe, Uganda for the support given in the research and write up of the manuscript. They also wish to thank Wakiso District for allowing the patients and the health workers to be used in data collection. Their continued support in empowering communities for healthier lives is highly appreciated.
Conflict of Interest
The authors declare no conflict of interest. The sponsors and supporters had no role in the design, implementation, interpretation, or writing of the study.
References
- World Health Organization. The global status report on non-communicable diseases. Geneva: World Health Organization (2015).
- Grimsrud A, Barnabas RV, Ehrenkranz P, et al. Evidence for scale up: the differentiated care research agenda. Journal of the International AIDS Society 20 (2017).
- World Health Organization. The global status report on non-communicable diseases. Geneva: World Health Organization (2016).
- Peck RN, Shedafa R, Kalluvya S, et al. Hypertension, kidney disease, HIV and antiretroviral therapy among Tanzanian adults: a cross-sectional study. BMC medicine 12 (2014): 125.
- Bahendeka S, Wesonga R, Mutungi G, et al. Prevalence and correlates of diabetes mellitus in Uganda: a population-based national survey. Tropical Medicine & International Health 21 (2016): 405-416.
- Oni T, McGrath N, BeLue R, et al. Chronic diseases and multi-morbidity-a conceptual modification to the WHO ICCC model for countries in health transition. BMC public health 14 (2014): 575-589.
- Kalyesubula R, Kayongo A, Semitala FC, et al. Trends and level of control of hypertension among adults attending an ambulatory HIV clinic in Kampala, Uganda: a retrospective study. BMJ global health 1 (2016): e000055.
- Temu F, Leonhardt M, Carter J, et al. Integration of non-communicable diseases in health care: tackling the double burden of disease in African settings. The Pan African Medical Journal 18 (2014).
- Ministry of Health. National antiretroviral treatment and care guidelines for adults and children. Kampala:Ministry of Health (2005).
- Hyle EP, Naidoo K, Su AE, et al. HIV, Tuberculosis, and Non-Communicable Diseases: What is known about the costs, effects, and cost-effectiveness of integrated care? Journal of acquired immune deficiency syndromes 67 (2014):
- Khabala KB, Edwards JK, Baruani B, et al. Medication Adherence Clubs: a potential solution to managing large numbers of stable patients with multiple chronic diseases in informal settlements. Tropical Medicine & International Health 20 (2015): 1265-1270.
- Wandeler G, Johnson L, Egger M. Trends in life expectancy of HIV-positive adults on antiretroviral therapy across the globe: comparisons with general population. Current Opinion in HIV and AIDS 11 (2016): 492-500.
- Johnson LF, Mossong J, Dorrington RE, et al. Life expectancies of South African adults starting antiretroviral treatment: collaborative analysis of cohort studies. PLoS medicine 10 (2013): e1001418.
- Narayan KV, Miotti PG, Anand NP, et al. HIV and non-communicable disease comorbidities in the era of antiretroviral therapy: a vital agenda for research in low-and middle-income country settings. Journal of Acquired Immuno-Deficiency Syndrome 7 (2014): 67-79.
- Levitt NS, Peer N, Steyn K, et al. Increased risk of dysglycaemia in South Africans with HIV; especially those on protease inhibitors. Diabetes research and clinical practice 119 (2011): 41-47.
- Guaraldi G, Orlando G, Zona S, et al. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clinical Infectious Diseases 53 (2011): 1120-1126.
- Triant VA, Lee H, Hadigan C, et al. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. The Journal of Clinical Endocrinology and Metabolism 92 (2007): 2506-2512.
- Kavishe B, Biraro S, Baisley K, et al. High prevalence of hypertension and of risk factors for non-communicable diseases (NCDs): a population based cross-sectional survey of NCDS and HIV infection in Northwestern Tanzania and Southern Uganda. BMC Medicine 13 (2015): 126.
- Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet 382 (2013): 1525±1533.
- Rajasuriar R, Khoury G, Kamarulzaman A, et al. Persistent immune activation in chronic HIV infection: do any interventions work? AIDS (London, England) 27 (2013): 1199.
- Rabkin M, El-Sadr WM. Why reinvent the wheel? Leveraging the lessons of HIV scale-up to confront non-communicable diseases. Global Public Health 6 (2011): 247-256.
- Ministry of Health. Uganda Population HIV Impact Assessment (UPHIA)Report. Kampala: Ministry of Health (2017).
- Abrahams-Gessel S, Denman CA, Gaziano TA, et al. Challenges facing successful scaling up of effective screening for cardiovascular disease by community health workers in Mexico and South Africa: Policy implications. Health systems and policy research 3 (2016): 13-15.
- Ministry of Health. Uganda Clinical Guidelines for National Guidelines for Management of Common Conditions. Kampala:Ministry of Health (2016).
- Nideröst S, Imhof C. Aging with HIV in the era of antiretroviral treatment: living conditions and the quality of life of people aged above 50 living with HIV/AIDS in Switzerland. Gerontology and Geriatric Medicine 2 (2016): 2333721416636300.
- Wu AW. Quality of life assessment comes of age in the era of highly active antiretroviral therapy. Aids 14 (2000): 1449-1451.
- Mills E J, Bakanda C, Birungi J, et al. Life expectancy of persons receiving combination antiretroviral therapy in low-income countries: a cohort analysis from Uganda. Annals of internal medicine 155 (2011): 209-216.
- Joint United Nations Programme on HIV/AIDS. Global AIDS update. Geneva: UNAIDS (2014).
- Domingues CSB, Waldman EA. Causes of death among people living with AIDS in the pre-and post-HAART eras in the city of São Paulo, Brazil. PLoS One 9 (2014): e114661.
- Gaspar J, Reis RK, Pereira FMV, et al. Quality of life in women with HIV/AIDS in a municipality in the State of São Paulo. Revista da Escola de Enfermagem da USP 45 (2011): 230-236.
- Oliveira FBM, Queiroz AAFLN, Sousa ÁFLD, et al. Sexual orientation and quality of life of people living with HIV/Aids. Revista Brasileira de Enfermagem 70 (2017): 1004-1010.
- De Sousa JCF, de Oliveira AC, Leadebal ODCP, et al. Quality of Life Evaluation of Elderly People Living with HIV/AIDS According to HAT-QoL. International Archives of Medicine 9 (2016).
- Ferreira B E, Oliveira IM, Paniago AMM. Quality of life of people living with HIV/AIDS and its relationship with CD4+ lymphocytes, viral load and time of diagnosis. Revista Brasileira de Epidemiologia 15 (2012): 75-84.
- Zhou T, Guan H, Yao J, et al. The quality of life in Chinese population with chronic non-communicable diseases according to EQ-5D-3L: a systematic review. Quality of Life Research 27 (2018): 2799-2814.
- Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Bmj 355 (2016):
- Chan YH. Randomized controlled trials (RCTs)-sample size: the magic number?. Singapore medical journal 44 (2003): 172-174.
- World Health Organization. Advancing cross-cultural research on quality of life: observations drawn from the WHOQOL development. Quality of Life research 11 (2002): 135-144.
- Joint United Nations Programme on HIV/AIDS. Global AIDS update. Geneva: UNAIDS (2017).
- Bhatta DN, Liabsuetrakul T. Efficacy of a Social Self-Value Empowerment Intervention to Improve Quality of Life of HIV Infected People Receiving Antiretroviral Treatment in Nepal: A Randomized Controlled Trial. AIDS and Behavior 21 (2017): 1620-1631.
- Decroo T, Telfer B, Dores CD, et al. Effect of Community ART Groups on retention-in-care among patients on ART in Tete Province, Mozambique: a cohort study. BMJ Open 7 (2017): e016800.
- Wageman R. The meaning of interdependence. Groups at work: Theory and research (2001): 197-217.
- Fulton BD, Scheffler RM, Sparkes SP, et al. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Human resources for health 9 (2011): 1.
- World Health Organization. Task shifting: rational redistribution of tasks among health workforce teams: global recommendations and guidelines (2007).
- Peters DH. Improving health service delivery in developing countries: from evidence to action. World Bank Publications (2009).
