Cochlear Implant Magnet Dislocation Caused by 1.5T MRI: Case Series Study
Article Information
Kento Koda MD1,2, Akinori Kashio MD, PhD1*, Tsukasa Uranaka MD1, Yujiro Hoshi MD1, Shigeo Takenouchi MD1, Yu Matsumoto MD, PhD1, Shinichi Iwasaki MD, PhD3, Tatsuya Yamasoba MD, PhD1
1Department of Otolaryngology and Head and Neck Surgery, The University of Tokyo, Tokyo, Japan
2Department of Otolaryngology and Head and Neck Surgery, Takeda General Hospital Aizuwakamatsu, Fukushima, Japan
3Department of Otolaryngology and Head and Neck Surgery, Nagoya City University, Nagoya, Japan
*Corresponding Author: Dr. Akinori Kashio, Department of Otolaryngology and Head and Neck Surgery, The University of Tokyo, Tokyo, Japan
Received: 03 August 2020; Accepted: 14 August 2020; Published: 14 September 2020
Citation: Kento Koda, Akinori Kashio, Tsukasa Uranaka, Yujiro Hoshi, Shigeo Takenouchi, Yu Matsumoto, Shinichi Iwasaki, Tatsuya Yamasoba. Cochlear Implant Magnet Dislocation Caused by 1.5T MRI: Case Series Study. Archives of Clinical and Medical Case Reports 4 (2020): 883-889.
View / Download Pdf Share at FacebookAbstract
Magnet dislocation (MD) is a serious concern for cochlear implant users. The frequency of magnetic resonance imaging (MRI) examination is much higher in Japan than in other countries, which may be a major problem for cochlear implant users. Here, we report two cases in which 1.5T MRI caused severe pain and MD of the cochlear implant. Both patients received cochlear implants manufactured by Cochlear Ltd., which are compatible with 1.5T MRI. Both patients experienced MD; in one case, manual fixation was attempted. Radiography revealed that the magnet seemed to be successfully fixed; however, ultrasonic echo indicated dislocation, and the magnet was finally fixed surgically. In the other case, the cochlear implant was surgically replaced because the original implant had a cracked silicon bed. Ultrasonic echo was a useful tool for visualizing the precise location of the magnet. Even when a magnet is successfully repositioned by manual fixation, the possibility that the silicon bed is also seriously damaged remains. Surgical fixation of the magnet is recommended to investigate whether or not the silicon bed is damaged, especially for patients who need to undergo repeat MRI examinations for follow-up.
Keywords
Magnet dislocation; Cochlear implant; Magnetic resonance imaging; Ultrasonic echo; Three-dimensional computed tomography
Magnet dislocation articles, Cochlear implant articles, Magnetic resonance imaging articles, Ultrasonic echo articles, Three-dimensional computed tomography articles
Magnet dislocation articles Magnet dislocation Research articles Magnet dislocation review articles Magnet dislocation PubMed articles Magnet dislocation PubMed Central articles Magnet dislocation 2023 articles Magnet dislocation 2024 articles Magnet dislocation Scopus articles Magnet dislocation impact factor journals Magnet dislocation Scopus journals Magnet dislocation PubMed journals Magnet dislocation medical journals Magnet dislocation free journals Magnet dislocation best journals Magnet dislocation top journals Magnet dislocation free medical journals Magnet dislocation famous journals Magnet dislocation Google Scholar indexed journals Cochlear implant articles Cochlear implant Research articles Cochlear implant review articles Cochlear implant PubMed articles Cochlear implant PubMed Central articles Cochlear implant 2023 articles Cochlear implant 2024 articles Cochlear implant Scopus articles Cochlear implant impact factor journals Cochlear implant Scopus journals Cochlear implant PubMed journals Cochlear implant medical journals Cochlear implant free journals Cochlear implant best journals Cochlear implant top journals Cochlear implant free medical journals Cochlear implant famous journals Cochlear implant Google Scholar indexed journals Magnetic resonance imaging articles Magnetic resonance imaging Research articles Magnetic resonance imaging review articles Magnetic resonance imaging PubMed articles Magnetic resonance imaging PubMed Central articles Magnetic resonance imaging 2023 articles Magnetic resonance imaging 2024 articles Magnetic resonance imaging Scopus articles Magnetic resonance imaging impact factor journals Magnetic resonance imaging Scopus journals Magnetic resonance imaging PubMed journals Magnetic resonance imaging medical journals Magnetic resonance imaging free journals Magnetic resonance imaging best journals Magnetic resonance imaging top journals Magnetic resonance imaging free medical journals Magnetic resonance imaging famous journals Magnetic resonance imaging Google Scholar indexed journals imaging articles imaging Research articles imaging review articles imaging PubMed articles imaging PubMed Central articles imaging 2023 articles imaging 2024 articles imaging Scopus articles imaging impact factor journals imaging Scopus journals imaging PubMed journals imaging medical journals imaging free journals imaging best journals imaging top journals imaging free medical journals imaging famous journals imaging Google Scholar indexed journals Ultrasonic echo articles Ultrasonic echo Research articles Ultrasonic echo review articles Ultrasonic echo PubMed articles Ultrasonic echo PubMed Central articles Ultrasonic echo 2023 articles Ultrasonic echo 2024 articles Ultrasonic echo Scopus articles Ultrasonic echo impact factor journals Ultrasonic echo Scopus journals Ultrasonic echo PubMed journals Ultrasonic echo medical journals Ultrasonic echo free journals Ultrasonic echo best journals Ultrasonic echo top journals Ultrasonic echo free medical journals Ultrasonic echo famous journals Ultrasonic echo Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals laparoscopy articles laparoscopy Research articles laparoscopy review articles laparoscopy PubMed articles laparoscopy PubMed Central articles laparoscopy 2023 articles laparoscopy 2024 articles laparoscopy Scopus articles laparoscopy impact factor journals laparoscopy Scopus journals laparoscopy PubMed journals laparoscopy medical journals laparoscopy free journals laparoscopy best journals laparoscopy top journals laparoscopy free medical journals laparoscopy famous journals laparoscopy Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Three-dimensional computed tomography articles Three-dimensional computed tomography Research articles Three-dimensional computed tomography review articles Three-dimensional computed tomography PubMed articles Three-dimensional computed tomography PubMed Central articles Three-dimensional computed tomography 2023 articles Three-dimensional computed tomography 2024 articles Three-dimensional computed tomography Scopus articles Three-dimensional computed tomography impact factor journals Three-dimensional computed tomography Scopus journals Three-dimensional computed tomography PubMed journals Three-dimensional computed tomography medical journals Three-dimensional computed tomography free journals Three-dimensional computed tomography best journals Three-dimensional computed tomography top journals Three-dimensional computed tomography free medical journals Three-dimensional computed tomography famous journals Three-dimensional computed tomography Google Scholar indexed journals tomography articles tomography Research articles tomography review articles tomography PubMed articles tomography PubMed Central articles tomography 2023 articles tomography 2024 articles tomography Scopus articles tomography impact factor journals tomography Scopus journals tomography PubMed journals tomography medical journals tomography free journals tomography best journals tomography top journals tomography free medical journals tomography famous journals tomography Google Scholar indexed journals
Article Details
1. Introduction
Cochlear implant (CI) is one of the most successfully used implant devices and is provided to patients with profound or severe sensorineural hearing loss. Patients with CI were previously unable to undergo magnetic resonance imaging (MRI) examination. However, recent improvements in CI technology have made it possible for CI users to undergo MRI, although guidelines for MRI vary depending on the CI manufacturers. Currently, patients with CI are allowed to undergo examination with 1.5T MRI, but complications associated with MRI, such as pain, discomfort, and dislocation of the magnet, have been reported [1]. Magnet dislocation (MD) after MRI, whose risk was reported approximately 6.5% [2], can cause pain, swelling, and sound-processor connection failure. Moreover, leaving a dislocated magnet may cause the magnet to break through the skin [3] and cause an infection [4], resulting in implant removal [5]. Therefore, early detection of MD and subsequent repositioning of the magnet is required. When the magnet is partially dislocated, manual repositioning without skin incision may be attempted. When the magnet is completely dislocated or when manual fixation of the magnet has failed, surgical repositioning is required.
Here, we present two CI cases of partial MD that occurred following the examination using 1.5T MRI. In the first case, the magnet appeared to be properly repositioned manually. However, ultrasonic examination (UE) after repositioning revealed that the magnet remained dislocated and surgical repositioning was conducted. In the second case, a surgical procedure was performed upon the patient’s request. During the surgery, the repositioning of the magnet was easy, but we found large cracks in the silicon bed. Therefore, surgical re-implantation was conducted.
2. Case Reports
2.1 Case 1
A 76-year-old man with profound bilateral sensorineural hearing loss underwent right cochlear implantation in 2017, and CI522 (produced by Cochlear Ltd. based in Australia) was successfully implanted. One and a half years after the surgery, he underwent endoscopic laminectomy for cervical spondylotic myelopathy. Four days postoperatively, a cervical 1.5T MRI was performed to follow-up on the surgery. The MRI examination was performed with the patient wearing a head bandage. Cochlear Ltd. provided the instruction that a splint should be placed over the magnet, with an elasticized compression bandage wrapped around the head at least twice. Although we did not use the splint, the elasticized compression bandage was wrapped more than twice to prevent MD of the CI. Immediately after MRI examination, however, he complained of pain and swelling in the right temporal region where the CI was implanted. Additionally, the speech processor coil could not connect to the implant. Head radiography revealed partial dislocation of the CI magnet. Initially, manual repositioning without skin incision was attempted to return the magnet to its proper place. After manual fixation, the pain and swelling reduced. The magnet appeared to be at the proper position in a second head radiograph, and the patient could wear the implant. However, remaining dislocation of the magnet was suspected with UE (Figure 1).
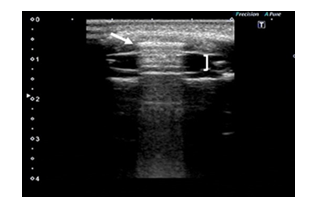
Figure 1: The magnet (arrowhead) was not within, but on the silicon bed (bracket).
High resolution computed tomography (CT) with 3D reconstruction confirmed that the magnet was still dislocated. Five days after the MRI examination, we surgically repositioned the magnet with a half circumferential skin incision around the receiver (Figure 2).
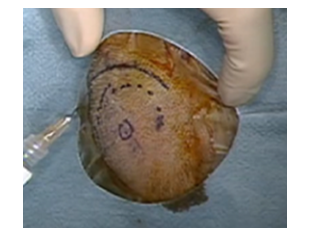
Figure 2: The surgical procedure was planned around the upper half of the silicon bed in case 1.
No cracks in the silicon bed were detected, and some effort was needed to reposition the magnet due to the tight silicon spacing. Postoperatively, the pain and swelling disappeared and the patient started using the CI 20 days after surgery.
2.2 Case 2
A 6-year-old boy with bilateral cochlear implants (Right: CI24RE, Left: CI422, produced by Cochlear Ltd. based in Australia) owing to congenital sensorineural hearing loss because of GJB2 gene mutation, experienced Fanconi anemia. A 1.5T MRI was conducted to rule out central nervous system lesions such as malformation. In this case, we had followed the manufacturer recommendations [2]. Before the MRI, the CI was fixed with elastic bandages and a splint (cardboard) to prevent MD. The MRI was conducted in the seated position. During the MRI, the patient woke up and the examination was terminated. The day after the MRI, the patient’s family noticed swelling around the right CI. Radiography was performed and partial MD was detected (Figure 3).
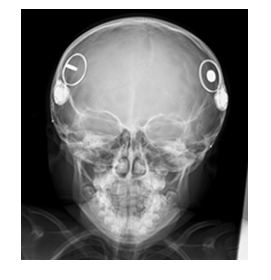
Figure 3: The right magnet was rotated 90°.
Manual repositioning was suggested as an initial treatment option, but surgical replacement of the magnet was performed, as requested by the patient’s family, to check for damage to the implant. A post-auricular incision along the existing skin incision (Figure 4) was chosen while preparing for CI replacement. During the surgical procedure, the magnet was easily returned to the correct location.
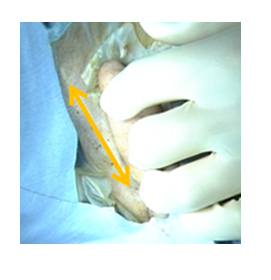
Figure 4: A post-auricular incision along the existing skin incision was selected.
However, careful inspection revealed a crack of the silicon. As MRI needs to be performed frequently in the future for follow-up on the Fanconi anemia, we decided to replace the implant with a new device. After removing the original implant, we discovered that the silicon bed behind the magnet was completely cracked.
3. Discussion
Here we report two cases of MD caused by 1.5T MRI. In the first case, the magnet appeared to be successfully repositioned according to local findings and X-ray imaging after manual repositioning; however, UE revealed that the magnet remained displaced. The magnet was surgically repositioned, but it was not easily returned to the silicon bed. In the second case, a surgical procedure was initially performed, and the magnet was easily repositioned, but careful inspection revealed that the silicon bed was cracked. Hassepass et al. [6] reported that 1.23% of CI recipients who underwent MRI needed surgery to remove or replace magnets and that approximately half of them had been using appropriate head bandages during the 1.5T MRI.
Cochlear Ltd. provides a guideline for performing MRI and supplies a bandage and splint kit for MRI examinations. They advise that the splint should be placed over the magnet, with an elasticized compression bandage wrapped around the head at least twice. In the first case, the Cochlear Ltd. guidelines were not fully followed [2] as the splint was not used. However, in the second case, although we did not use the bandage and splint kit provided by the manufacture, we did place a splint in the correct location and the bandage was rapped more than twice. These indicate that, even when using the appropriate head bandage protection method, the risk of MD and the necessity of the MRI should be carefully discussed with patients and their family before examination.
MD has mostly been detected with radiography [7, 8]. When the magnet is displaced far from the receiver or when the magnet direction is not parallel to the receiver, MD can be easily diagnosed. In our first case, the magnet was almost perpendicular to the receiver after MRI examination, making diagnosis of MD easily with radiography. After manual repositioning, the magnet was oriented parallel to and just outside the receiver, thereby appearing properly repositioned on subsequent X-ray imaging. A decrease in pain and reduction in swelling was also suggestive of the magnet returning to the correct position. In this situation, UE showed the depth relation between the magnet and the receiver, which clearly indicated the failure of the manual repositioning. This indicates that there is a possibility of misdiagnosis of MD with X-ray imaging alone. High resolution CT, especially with 3D reconstruction, can confirm precise magnet location. Indeed, we could see the dislocated magnet just outside the receiver using 3D-CT. Considering the cost and time effectiveness and necessity of radiation exposure, however, initial screening using UE is more practical.
The second case suggested that when a magnet is easily repositioned by manual fixation, there remains a possibility that the silicon bed is seriously damaged. In this case, we suspected that the silicon bed was damaged because the magnet was repositioned too easily into the silicon bed during the surgery compared to the other case. Since the magnet should be tightly imbedded in the silicon bed, the edge of the silicon bed is usually hard. Therefore, effort is required to return the magnet to the bed. There are several reports [9,10] in which the magnet was successfully repositioned using manual fixation methods. However, this second case indicates a possibility that in many of these cases, the magnet may be able to be repositioned due to a crack in the silicon bed. In fact, a case of minor head trauma has been reported to develop recurrence of MD, in which the damage to the silicon bed was found during the second surgery [11]. Therefore, surgical repositioning is recommended with a careful checkup of the silicon bed to identify its possible damage. If manual repositioning is selected, information on the possible recurrence of MD by physical impact near the implant should be given to the patient, along with careful follow-up. Moreover, in these settings, it is important to consider the skin incision line so that a repositioning operation can always be switched to a replacement operation.
4. Conclusion
We encountered two CI patients with MD caused by exposure to 1.5T MRI. Even when the magnet appears to be replaced in the correct location after manual fixation upon X-ray imaging, there still remains a risk of MD above the silicon bed. UE can be useful for determining the dislocation of the magnet. Surgical exploration of the implant is recommended to investigate whether the silicon bed is damaged, especially in patients who need to undergo repeated MRI examinations. Additionally, when planning the incision, it is better to keep in mind the need for future replacement surgeries for the cochlear implant instead of using the incision recommended by the manufacturer.
5. Disclosure Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Grupe G, Wagner J, Hofmann S, et al. Prevalence and complications of MRI scans of cochlear implant patients: English version. HNO 65 (2017): 35-40.
- Srinivasan R, So CW, Amin N, et al. A review of the safety of MRI in cochlear implant patients with retained magnets. Clin Radiol 74 (2019): 972.e9-972.e16.
- Hassepass F, Stabenau V, Arndt S, et al. Magnet dislocation: an increasing and serious complication following MRI in patients with cochlear implants. Rofo 186 (2014): 680-685.
- Cunningham III CD, Slattery III WH, Luxford WM. Postoperative infection in cochlear implant patients. Otolaryngol Head Neck Surg 131 (2004): 109-114.
- Skrivan J, Drevinek P. A case report of a cochlear implant infection - A reason to explant the device? Cochlear Implants Int 17 (2016): 246-249.
- Hassepass F, Stabenau V, Maier W, et al. Revision surgery due to magnet dislocation in cochlear implant patients: an emerging complication. Otol Neurotol 35 (2014): 29-34.
- Leong WJC, Yuen HW. Dislocation of cochlear implant magnet during 1.5 Tesla magnetic resonance imaging despite head bandaging, and its repositioning using an endoscopic approach. J Laryngol Otol 132 (2018): 943-945.
- Wilkinson EP, Dogru S, Meyer TA, et al. Case report: Cochlear implant magnet migration. Laryngoscope 114 (2004): 2009-2011.
- Sasamori K, Hiraumi H, Shimamoto K, et al. A case of magnet displacement in a cochlear implant detected after MRI corrected by a non-invasive approach. Pract Otorhino-laryngol 110 (2017): 241-244.
- Di Nardo W, Giannantonio S, Schinaia L, et al. Noninvasive management of cochlear implant’s inner magnet displacement after magnetic resonance. Laryngoscope 123 (2013): 783-786.
- Mickelson JI, Kozak F. Magnet dislodgement in cochlear implantation: correction utilizing a lasso technique. Int J Pediatr Otorhinolaryngol 72 (2008): 1071-1076.
