Clinicopathological Characteristics of Colorectal Cancer: A Retrospective Study in Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
Article Information
Mohammad Zillur Rahman1*, Saumitra Chakravarty2, Mohammad Shukur Ali3, Mohammad Abir Hasan Siddique Rahi4, Syeda Rumman Aktar Siddiqui5
1Professor and Chairman, Department of Pathology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Shahbag, Dhaka, Bangladesh.
2Assistant Professor, Department of Pathology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
3Professor, Department of English, University of Development Alternative (UODA), Dhaka, Bangladesh
4Research Assistant, Department of Pathology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
5Associate Professor, Department of Biochemistry, Chittagong Medical College, Chattogram, Bangladesh.
*Corresponding author:Mohammad Zillur Rahman, MBBS, M Phil (Pathology), PhD, Professor and Chairman, Department of Pathology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Shahbag, Dhaka, Bangladesh
Received: March 27, 2024; Accepted: April 08, 2024; Published: April 25, 2024
Citation: Mohammad Zillur Rahman, Saumitra Chakravarty, Mohammad Shukur Ali, Mohammad Abir Hasan Siddique Rahi, Syeda Rumman Aktar Siddiqui. Clinicopathological Characteristics of Colorectal Cancer: A Retrospective Study in Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh. Journal of Cancer Science and Clinical Therapeutics 8 (2024): 106-111.
View / Download Pdf Share at FacebookAbstract
Introduction: Colorectal cancer (CRC) is a major health issue and ranks as the third most frequently diagnosed and second most deadly cancer globally. Colorectal cancer (CRC) accounted for around 9.4% of cancer-related deaths worldwide in 2020. The prevalence of CRC exhibits significant variation, with elevated rates observed in North America, Australia, and Northern and Western Europe. Patients in the South Asian population commonly exhibit colorectal cancer (CRC) at a younger age and typically at an advanced stage. CRC is not widely prevalent in the Indian subcontinent. The prevalence of colorectal cancer in India was determined to be 4.2 and 3.2 per one hundred thousand individuals for males and females, respectively. The precise prevalence of colorectal cancer in Bangladesh remains unknown. This article aimed to identify the clinicopathological characteristics of colorectal cancer in Bangladeshi patients, regardless of age and gender.
Methods: This retrospective study was conducted at the Department of Pathology in Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh between October 2023 and March 2024. The study involved analyzing data from 293 patients with excised colorectal cancer. Statistical software (SPSS version 23.0) was used to analyze the data.
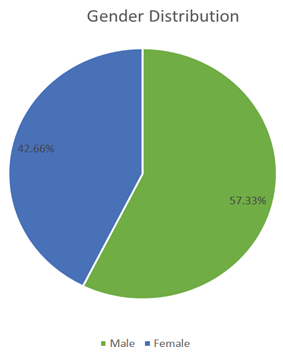
Results: A series of 293 excised cases of colorectal carcinoma irrespective of age and sex were enrolled in this study. The mean age of the patients was 48.39±14.61 years.Most cases (168, 57.33%) were males. Ascending colon was the most frequent (87, 29.69%) site of the growth of colorectal carcinoma. Most common morphological pattern was exophytic (130, 44.36%).The most frequent histologic type of colorectal carcinoma was found to be adenocarcinoma NOS 238(81.22%). The most frequent histological grade was marked as low grade (243, 82.93%). Among the stages of pT, the most frequent stage was identified as pT3 (180, 61.43%) and among pN, the most frequent stage was found to be pN0 (164, 55.9%).
Conclusion: Most of the colorectal carcinoma was observed in the middle and old aged people. The male dominance was found in the incidence of colorectal carcinoma. Adenocarcinoma NOS was the most frequent histpathological type of colorectal carcinoma among the study patients. Colorectal carcinoma involved in ascending colon in majority of the cases. Most of the cases were diagnosed at an advanced tumor (pT) stage.
Keywords
<p>Clinicopathological, Colorectal carcinoma, Tumor, Adenocarcinoma.</p>
Clinicopathological articles; Colorectal carcinoma articles; Tumor articles; Adenocarcinoma articles.
Article Details
Introduction
Colorectal cancer (CRC) is a major global health concern. It ranks as the world's third most commonly diagnosed and second leading cause of cancer death [1]. Globally, CRC caused an estimated 9.4% of cancer-related deaths in 2020 [2]. Incidence varies significantly across regions. North America, Australia, and Northern and Western Europe have higher rates [3-5]. In contrast, patients in South Asia tend to be diagnosed at a younger age and often at a later stage [6-7]. CRC is considered relatively uncommon in the Indian subcontinent. Studies in India report an incidence of 4.2 and 3.2 per hundred thousand for males and females, respectively [8]. While data on Bangladesh is limited, CRC is reportedly more frequent and occurs in middle-aged and older adults, with a slightly higher prevalence in males [9]. The global burden is projected to more than double by 2035, with the most significant rise in less developed countries [10]. CRC arises from abnormal cell growth in the colon or rectum. Three main types exist: sporadic, hereditary, and colitis-associated. Risk factors include environmental and genetic influences, as well as chronic inflammatory bowel diseases like ulcerative colitis and Crohn's disease [11, 12]. Diet, lifestyle, family history, and chronic inflammation all contribute. Screening average- risk individuals is the most effective strategy to reduce CRC deaths [13]. Many European countries, Canada, and specific regions in North and South America, Asia, and Oceania have implemented population-based screening programs [14]. These programs target specific age groups and geographical areas. Microsimulation modelling in the United States suggests screening programs have led to a decline in CRC morbidity and mortality [15].Population-based screening aims to detect hidden diseases in average-risk individuals, enabling early intervention and reducing individual and community risk [16]. CRC is a suitable target for screening due to its prevalence and the belief that it develops through a gradual process called the adenoma-carcinoma sequence [17]. While the exact timeframe for an adenoma to progress to CRC is unknown, evidence suggests it takes at least ten years [18]. This extended window allows for detection through screening and potential curative treatment. Additionally, removing colorectal adenomas can prevent CRC entirely [19]. Earlier detection also translates to a better chance of survival [20]. Understanding the clinicopathological characteristics of CRC in Bangladeshi patients is crucial for developing effective preventive measures based on current knowledge. However, limited data exists in this area. This study aimed to address this gap by investigating the clinicopathological features of CRC in Bangladeshi patients regardless of age and sex.
Materials and Methods
This study employed a retrospective cross-sectional design at the Department of Pathology, Bangabandhu Sheikh Mujib Medical University (BSMMU) in Dhaka, Bangladesh.
The data collection period spanned from October 2023 to March 2024. Consecutive sampling technique was used to enrol 293 patients with excised colorectal carcinoma, regardless of age or sex. Tumor classification followed the World Health Organization (WHO) Classification of Digestive System Tumors [14]. Grading utilized the Canadian Cancer Society's (CCS) two-tiered system [15]. Staging adhered to the American Cancer Society's TNM Classification of Colorectal Carcinoma (2020 edition) [16]. Data collection involved using an Excel spread sheet from the BSMMU Pathology Department registry. The collected data underwent meticulous organization, editing, and coding for computer entry. The analysis employed the Statistical Package for Social Sciences (SPSS) software, version 23.0. Descriptive statistics were used to present the findings in tables and charts.
Results
Table 1: Demographic characteristics of the study patients (n=293).
|
Frequency |
Percent |
|
|
Age(years) |
||
|
<20 |
3 |
1 |
|
21-40 |
88 |
30 |
|
41-60 |
136 |
46 |
|
61-80 |
64 |
21 |
|
>81 |
2 |
0.7 |
|
Total |
293 |
100 |
|
Mean age(years) |
48.39±14.61 |
|
|
Median |
50 |
|
|
Mode |
51 |
|
|
Sex |
||
|
Male |
168 |
57.33 |
|
Female |
125 |
42.66 |
|
Total |
293 |
100 |
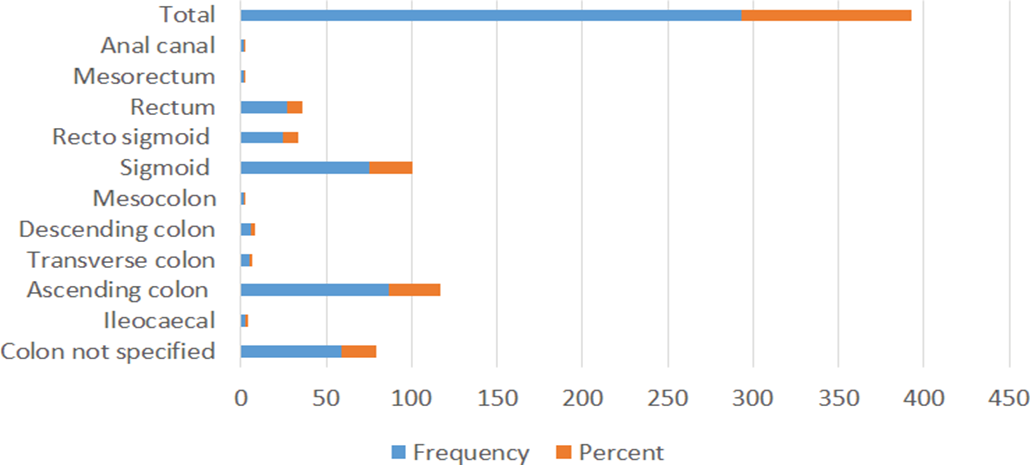
Figure 2 shows the site distribution of the growth of colorectal carcinoma with the study patients. The most frequent site of the growth of the colorectal carcinoma was observed at ascending colon in 87(29.69%) patients followed sigmoid colon in 75(25.59%), colon not specified in 59(20.`13%), rectum region in 27(9.21%), recto sigmoid in 25(8.53%), descending colon in 6(2.04%) ,transverse colon in 5(1.7o%),Ileocaecal region in 3(1.02%), mesorectum in 2(0.70%) and anal canal in only 2(0.70%).
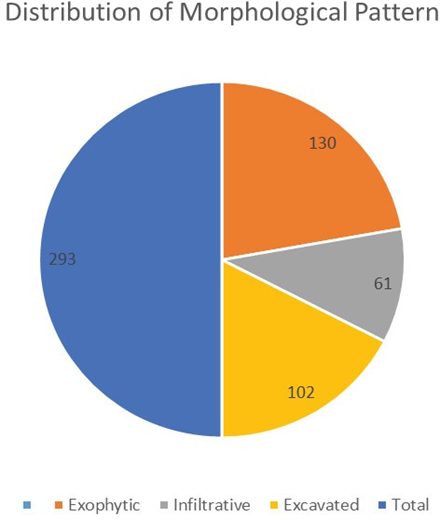
Figure 3 shows the distribution of configuration of tumour of colorectal carcinoma. The most frequent configuration of tumour was observed to be exophytic in 130 (44.36%) patients followed excavated in 102(34.81%), and infiltrative in 61(20.81).
Table 2 shows the distribution of histologic type of colorectal carcinoma with the study patients. The most frequent histologic type of colorectal carcinoma was adenocarcinoma NOS found in 238(81.22%) patients followed mucinous adenocarcinoma 53(18.08%), papillary adenocarcinoma in only 2(0.70%).
Table 3 shows the grade distribution of observed colorectal carcinoma. The most frequent grade of colorectal carcinoma was observed low grade in 243(82.93%) and 50(17.06%) cases were high grade.
Table 4 shows the distribution of stages of colorectal carcinoma of the study patients. Among the pT stages, the most frequent stage was observed pT3 180(61.43%) followed pT2 77(26.3%), pT4 23(7.84%), pT1 13(4.4%).
and among the stages pN, the most dominant stage was
pN1,57(19.5%) and followed pN2, 38(13%), pN2b,,15(5.1%), pN1b,4(1.4),pN1a,1(0.3%) and pN1c,0(0%).
Table 5 shows the distribution of lymph node involvement of colorectal carcinoma. The most frequent lymph node involvement was found N2b, 15 (5.1%), followed N2a 9(3.1%), N1b 4(1.4%) and N1a 1(0.3%).
Table 2: Distribution of histologic type of colorectal carcinoma (n=293).
|
Histologic type of colorectal carcinoma |
Frequency |
Percent |
|
Adenocarcinoma NOS |
238 |
81.22 |
|
Mucinous Adenocarcinoma |
53 |
18.08 |
|
Papillary Adenocarcinoma |
2 |
0.7 |
|
Total |
293 |
100 |
Table 3: Grade distribution of observed colorectal carcinoma (n=293)
|
Histologic Grade of Colorectal carcinoma |
Frequency |
Percent |
|
Low grade |
243 |
82.93 |
|
High grade |
50 |
17.06 |
|
Total |
293 |
100 |
Table 4: Distribution of stages of colorectal carcinoma (n=293)
|
Stages |
N(%) |
Stages |
N(%) |
|
T |
N |
||
|
pTx |
0(0) |
pNx |
5(1.7) |
|
pT0 |
0(0) |
pN0 |
164(55.9) |
|
pTis |
0(0%) |
pN1 |
57(19.5) |
|
pT1 |
13(4.4) |
pN1a |
1(0.3) |
|
pT2 |
77(26.3) |
pN1b |
4(1.4) |
|
pT3 |
180(61.43) |
pN1c |
0(0) |
|
pT4 |
23(7.84) |
pN2 |
38(13) |
|
pN2a |
9(3.1) |
||
|
pN2b |
15(5.1) |
||
|
Total |
293(100) |
293(100) |
Table 5: Distribution of lymph node involvement of colorectal carcinoma (n=293).
|
Lymph node involvement |
Frequency |
Percent |
|
N1a |
1 |
0.3 |
|
N1b |
4 |
1.4 |
|
N2a |
9 |
3.1 |
|
N2b |
15 |
5.1 |
|
Total |
29 |
9.9 |
Discussion
This retrospective study at Bangabandhu Sheikh Mujib Medical University (BSMMU) investigated the clinicopathological characteristics of colorectal cancer (CRC) in 293 patients. The average patient age was 48.4 years, with the highest incidence (46%) occurring in the 41-60 age group. These findings suggest a higher prevalence in middle and older adults, similar to a study in Indonesia[21] with a mean age of 53.2 years. However, our study observed a higher proportion of cases under 50 years old (compared to 38.1% in the Indonesian study). This difference might be due to variations in lifestyle, diet, or environmental factors between the populations. Males were more likely to be diagnosed with CRC (57.3%) compared to females. This could be associated with smoking, alcohol consumption, or a more Westernized lifestyle among males. These findings are consistent with a study in Iran [22] that reported 50.9% male patients. The most frequent tumor locations were the ascending colon (29.7%) and sigmoid colon (25.6%). This distribution differs from a study in Bangladesh [23] which found the rectum to be the most common site (36.7%), followed by the sigmoid colon (33.3%). These variations highlight the need for further research on geographical disparities in CRC presentation. Exophytic (44.4%) was the most common tumor configuration, followed by excavated (34.8%) and infiltrative (20.8%). Adenocarcinoma NOS (81.2%) was the predominant histological type, followed by mucinous adenocarcinoma (18.1%). These findings partially align with a study in Poland [24] where exophytic tumors comprised 50% and adenocarcinoma NOS constituted 87% of cases. Low-grade tumors (82.9%) were more prevalent than high-grade tumors (17.1%). Similarly, stage pT3 (61.4%) was the most common tumor stage, followed by pN0 (55.9%) for lymph node involvement. These findings differ somewhat from previous studies [25, 26] which reported higher proportions of high-grade tumors and advanced stages. Further investigation is needed to understand these variations. In conclusion, this study provides valuable insights into the clinicopathological characteristics of CRC in Bangladeshi patients. However, considering the global burden of CRC, a comprehensive strategy is crucial to raise awareness and reduce CRC mortality in Bangladesh.
Limitations of the study
This study was conducted in a single centre with a limited consecutive sampling technique. Therefore, the results of this study may not reflect the representative scenario of the whole country. Hence a multi-centre study may be conducted across the country with an adequate sample size
Conclusion
This study found colorectal cancer (CRC) to be more frequent in middle-aged and older adults. Males were also diagnosed with CRC more often than females. Adenocarcinoma NOS was the most common histological type, and the ascending colon was the most frequent tumor location. Additionally, a majority of cases were diagnosed at an advanced tumor (t) stage.
Recommendations
Necessary policies should be adopted to promote awareness about the growth of colorectal cancer especially among the adult population to promote colorectal health care at an early stage, screening program, affordable treatment and better prognosis.
Conflict of interest:
None declared
Funding:
Self
References
- Cancer (2021).
- Ferlay J, Ervik M, Lam F, et Global Cancer Observatory: Cancer Today (2021).
- Aljebreen Clinico-Pathological Patterns of Colorectal Cancer in Saudi Arabia: Younger with an Advanced Stage Presentation. Saudi J Gastroenterology 33 (2007): 84-87
- Hamilton SR. Carcinoma of the colon and rectum. In: Hamilton SR and Aaltonen LA, editors. Pathology and Genetics of Tumour of the Digestive System. France: IARC press (2000): 103-142.
- Jemal A, Bray F, Center MM, et Global cancer statistics. CA Cancer J Clin 61 (2011): 69-90.
- Ahmed S, Banerjea A, Hands RE, et Microarray profiling of colorectal cancer in Bangladeshi patients. Colorectal Dis 7 (2005): 571-575.
- Moore MA, Ariyaratne Y, Badar F, et Cancer epidemiology in South Asia-past, present and future. Asian Pac J Cancer Prev 11 (2009): 49-66.
- Afroza A, Hasan S, Rukunuzzaman M, et al. Carcinoma- Rectum in an 11 Years old Boy. Mymensingh Med J 16 (2007): 70-72.
- Rosai Gastrointestinal tract. In: Rosai J, editors. Ackerman's Surgical Pathology, 9 th ed. USA: Mosby company (2004): 776-825.
- Papamichael D, Audisio A, Glimelius B, et al. Treatment of colorectal cancer in older patients: International Society of Geriatric Oncology (SIOG) consensus recommendations 2013. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol 26 (2015): 463-476.
- Triantafillidis K, Nasioulas G, Kosmidis PA. Colorectal cancer and inflammatory bowel disease: Epidemiology, risk factors, mechanisms of carcinogenesis and prevention strategies. Anticancer Res 29 (2009): 2727-2737.
- Edwards B K, Ward E, Kohler B A, et Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 116 (2010): 544-573.
- Jemal A, Bray F, Center MM, et Global cancer statistics. CA Cancer J Clin 61 (2011): 69-90.
- Ahmed S, Banerjea A, Hands RE, et Microarray profiling of colorectal cancer in Bangladeshi patients. Colorectal Dis 7 (2005): 571-575.
- Edwards B.K, Ward E, Kohler B.A, et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 116 (2010): 544-573.
- Wilson M, Jungner Y G. Principles and practice of mass screening for disease. Bol. Oficina Sanit. Panam 65 (1968): 281-393.
- Morson B The evolution of colorectal carcinoma. Clin. Radiol 35 (1984): 425-431.
- Winawer S J, Fletcher R H, Miller L, et al. Colorectal cancer screening: Clinical guidelines and Gastroenterology 112 (1997): 594-642.
- Winawer S J, Zauber A G, Ho M N, et Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N. Engl. J. Med 329 (1993): 1977-1981.
- Ciccolallo L, Capocaccia R, Coleman M P, et Survival differences between European and US patients with colorectal cancer: Role of stage at diagnosis and surgery. Gut 54 (2005): 268-273.
- Rahadiani N, Habiburrahman M, Abdullah M, et Analysing 11 years of incidence trends, clinicopathological characteristics, and forecasts of colorectal cancer in young and old patients: a retrospective cross-sectional study in an Indonesian national referral hospitalBMJOpen 12 (2022): e060839.
- F Hajmanoochehri et al. Clinicopathological features of colon adenocarcinoma in qazvin, Iran: A 16 Year Study. Asian Pacific Journal of Cancer Prevention 15 (2014): 951-955.
- Mahamud MM, Wahed F, Ferdous J, et Clinicopathological Assessment of Colorectal Carcinoma in Mymensingh Medical College Hospital, Bangladesh. Mymensingh Med J 26 (2017): 892-899.
- Kolos M, Wasaznik-Jedras A, and Nasierowska- Guttmejer A. Original paper Can the histological type of colorectal cancer determine the carcinogenesis pathway? Polish Journal of Pathology 66 (2015): 109-120.
- Connell WR, Talbot IC, Harpaz N, et Clinicopathological characteristics of colorectal carcinoma complicating ulcerative colitis. Gut 35 (1994): 1419-1423.
- Anssari S, Elhaitmy Y, Amaadour L, et Comparison of clinicopathological and survival features of right and left colon cancers: Experience of the Medical Oncology Department of Fez. Journal of Cancer Therapy 14 (2023): 291-298.