Clinical Study on Reconstruction of Soft Tissue Defects of the Digits by Volar Flaps
Article Information
Su-Ryon Ryang*, Myong-Guk Jang, Kuk-Chol Kim, Song-Gun Ri
Pyongyang Medical College, KIM IL SUNG University, Pyongyang, Democratic People’s Republic of Korea
*Corresponding Author: Su-Ryon Ryang, Pyongyang Medical College, KIM IL SUNG University,Pyongyang, Democratic People’s Republic of Korea
Received: 11 November 2019; Accepted: 06 January 2020; Published: 27 January 2020
Citation: Su-Ryon Ryang, Myong-Guk Jang, Kuk-Chol Kim, Song-Gun. Clinical study on reconstruction of soft tissue defects of the digits by volar flaps. Journal of Orthopaedics and Sports Medicine 2 (2020): 10-17.
View / Download Pdf Share at FacebookAbstract
Background: Soft tissue deficiency in the upper limb is a common presentation following trauma, burns infection and tumor removal. Soft tissue coverage of the hand is a challenging problem for reconstructive surgeons to manage. The ideal flap for volar defects on the digits should provide glabrous skin, maintain length, and supple enough to allow unimpeded motion of the joints. Local flaps are the common choice in the management of injury. However, the development of microsurgery and clinical practice have greatly boosted the application of different flaps for finger pulp reconstruction with excellent results, especially when local flaps are unsuitable or impossible for the coverage of pulp defects. We newly describe our experience of the use of the transfer of glabrous skins based on the radialis indicis artery and common palmar digital artery for digital (volar) reconstruction.
Methods: Between 2010 and 2014, we used this flaps to reconstruct digital pulp defects in 13 patients with mean age of 33.6 years (range 21-55 years). The dimension of the flaps ranged from 1.8 cm × 2.6 cm to 1.6 cm × 3 .7 cm. The indications for surgery included amputation, severe pulp space infection, crush injury and salvage of failed local flap. The donor site was closed with skin graft directly in all cases.
Results: There were no flap failures. All wounds healed with good functional outcomes with ideal tissue match, minimal donor site morbidity and return of protective sensation despite no neurorrhaphy performed.
Conclusion: Volar flaps has many advantages, approaching ideal replacement for the volar tissues of the fingers, excellent tissue match, minimal donor site morbidity, non-sacrifice of a major vessel, can be made ‘sensory’, neurotises well. We believe that volar flaps is a very reliable and useful option in the armory of the reconstructive
Keywords
Soft tissue defect; Volar flaps; Digit
Soft tissue articles Soft tissue Research articles Soft tissue review articles Soft tissue PubMed articles Soft tissue PubMed Central articles Soft tissue 2023 articles Soft tissue 2024 articles Soft tissue Scopus articles Soft tissue impact factor journals Soft tissue Scopus journals Soft tissue PubMed journals Soft tissue medical journals Soft tissue free journals Soft tissue best journals Soft tissue top journals Soft tissue free medical journals Soft tissue famous journals Soft tissue Google Scholar indexed journals Finger pulp articles Finger pulp Research articles Finger pulp review articles Finger pulp PubMed articles Finger pulp PubMed Central articles Finger pulp 2023 articles Finger pulp 2024 articles Finger pulp Scopus articles Finger pulp impact factor journals Finger pulp Scopus journals Finger pulp PubMed journals Finger pulp medical journals Finger pulp free journals Finger pulp best journals Finger pulp top journals Finger pulp free medical journals Finger pulp famous journals Finger pulp Google Scholar indexed journals Hand injuries articles Hand injuries Research articles Hand injuries review articles Hand injuries PubMed articles Hand injuries PubMed Central articles Hand injuries 2023 articles Hand injuries 2024 articles Hand injuries Scopus articles Hand injuries impact factor journals Hand injuries Scopus journals Hand injuries PubMed journals Hand injuries medical journals Hand injuries free journals Hand injuries best journals Hand injuries top journals Hand injuries free medical journals Hand injuries famous journals Hand injuries Google Scholar indexed journals Skin grafts articles Skin grafts Research articles Skin grafts review articles Skin grafts PubMed articles Skin grafts PubMed Central articles Skin grafts 2023 articles Skin grafts 2024 articles Skin grafts Scopus articles Skin grafts impact factor journals Skin grafts Scopus journals Skin grafts PubMed journals Skin grafts medical journals Skin grafts free journals Skin grafts best journals Skin grafts top journals Skin grafts free medical journals Skin grafts famous journals Skin grafts Google Scholar indexed journals Joints articles Joints Research articles Joints review articles Joints PubMed articles Joints PubMed Central articles Joints 2023 articles Joints 2024 articles Joints Scopus articles Joints impact factor journals Joints Scopus journals Joints PubMed journals Joints medical journals Joints free journals Joints best journals Joints top journals Joints free medical journals Joints famous journals Joints Google Scholar indexed journals Tendon articles Tendon Research articles Tendon review articles Tendon PubMed articles Tendon PubMed Central articles Tendon 2023 articles Tendon 2024 articles Tendon Scopus articles Tendon impact factor journals Tendon Scopus journals Tendon PubMed journals Tendon medical journals Tendon free journals Tendon best journals Tendon top journals Tendon free medical journals Tendon famous journals Tendon Google Scholar indexed journals Hatchet flap articles Hatchet flap Research articles Hatchet flap review articles Hatchet flap PubMed articles Hatchet flap PubMed Central articles Hatchet flap 2023 articles Hatchet flap 2024 articles Hatchet flap Scopus articles Hatchet flap impact factor journals Hatchet flap Scopus journals Hatchet flap PubMed journals Hatchet flap medical journals Hatchet flap free journals Hatchet flap best journals Hatchet flap top journals Hatchet flap free medical journals Hatchet flap famous journals Hatchet flap Google Scholar indexed journals Foot articles Foot Research articles Foot review articles Foot PubMed articles Foot PubMed Central articles Foot 2023 articles Foot 2024 articles Foot Scopus articles Foot impact factor journals Foot Scopus journals Foot PubMed journals Foot medical journals Foot free journals Foot best journals Foot top journals Foot free medical journals Foot famous journals Foot Google Scholar indexed journals Radialis indicis artery articles Radialis indicis artery Research articles Radialis indicis artery review articles Radialis indicis artery PubMed articles Radialis indicis artery PubMed Central articles Radialis indicis artery 2023 articles Radialis indicis artery 2024 articles Radialis indicis artery Scopus articles Radialis indicis artery impact factor journals Radialis indicis artery Scopus journals Radialis indicis artery PubMed journals Radialis indicis artery medical journals Radialis indicis artery free journals Radialis indicis artery best journals Radialis indicis artery top journals Radialis indicis artery free medical journals Radialis indicis artery famous journals Radialis indicis artery Google Scholar indexed journals Surgery articles Surgery Research articles Surgery review articles Surgery PubMed articles Surgery PubMed Central articles Surgery 2023 articles Surgery 2024 articles Surgery Scopus articles Surgery impact factor journals Surgery Scopus journals Surgery PubMed journals Surgery medical journals Surgery free journals Surgery best journals Surgery top journals Surgery free medical journals Surgery famous journals Surgery Google Scholar indexed journals Pedicle flaps articles Pedicle flaps Research articles Pedicle flaps review articles Pedicle flaps PubMed articles Pedicle flaps PubMed Central articles Pedicle flaps 2023 articles Pedicle flaps 2024 articles Pedicle flaps Scopus articles Pedicle flaps impact factor journals Pedicle flaps Scopus journals Pedicle flaps PubMed journals Pedicle flaps medical journals Pedicle flaps free journals Pedicle flaps best journals Pedicle flaps top journals Pedicle flaps free medical journals Pedicle flaps famous journals Pedicle flaps Google Scholar indexed journals Joint stiffness articles Joint stiffness Research articles Joint stiffness review articles Joint stiffness PubMed articles Joint stiffness PubMed Central articles Joint stiffness 2023 articles Joint stiffness 2024 articles Joint stiffness Scopus articles Joint stiffness impact factor journals Joint stiffness Scopus journals Joint stiffness PubMed journals Joint stiffness medical journals Joint stiffness free journals Joint stiffness best journals Joint stiffness top journals Joint stiffness free medical journals Joint stiffness famous journals Joint stiffness Google Scholar indexed journals
Article Details
1. Introduction
Finger pulp is a common site for hand injuries, and pulp reconstruction is significantly important for optimal handling and sensation [1]. Although never exceeding a few square centimeters, finger pulp defects are reconstructive challenges due to their special requirements and lack of neighboring tissue reserve [2]. Flaps will be considered for hand reconstruction when the soft tissue coverage is unsuitable for the application of skin grafts, there is need for subcutaneous tissue as well as skin tissue replacement and for the coverage of important structures including nerves joints and tendons [3, 4]. Flap coverage is currently the most effective treatment method. Numerous local or regional flaps have been used to cover medium to small size (within middle and distal phalanges) finger pulp defects, such as the volar V-Y advancement flap [5], hatchet flap [6], reversed digital artery flap [7], thenar flap [8], cross-finger flap [9], and first dorsal metacarpal artery flap [10]. Medium to large defects of the volar soft tissue of the fingers continue to present a therapeutic challenge [11]. There are several options for soft tissue reconstruction in the upper extremity including skin grafting, local flaps, regional flaps and free flaps [12]. The preferred approach is the simplest method which can provide the most stable coverage. The mechanism, time, location and extent of soft tissue injury, severity of contamination, nature of the structure exposed and expected outcomes of spontaneous healing of the defect will dictate the soft tissue reconstruction options used in the upper limb [12]. Successful soft tissue coverage requires removal of all necrotic tissue, control of contamination and confirmation of a good blood supply [13, 14]. Small defects are usually managed by dressings only, skin grafts or with local flaps [15, 16]. Even for these smaller defects, improperly executed local flaps may fail creating larger defects that require salvage. According to the dictum of Harold Gilles which is replacing ‘like for like’, the ideal replacement for volar skin loss on the digits should provide padding or cushion, have a good color and texture match, be sensate or have potential to be sensate, resilient, maintain length and not limit motion [17, 18]. Only glabrous skin can achieve this ideal but are plagued by problem of limited availability. Therefore skin for coverage of defects on the volar surface of the digits should ideally be imported from sources of ‘like tissue’ (i.e. glabrous skin) namely the same or adjacent digits, palm and soles of the feet. Glabrous skin can be provided by loco regional flaps, or free flaps from the foot and toes (toe pulp, toe web, medial plantar artery perforator flap using instep skin)), or digits palm [15, 16, 19-30]. Delayed donor site wound healing, hypertrophic scars, slower mobilization of patient and questionable or low patient acceptance commonly complicate the use of the sole of the foot for free tissue transfer [11, 26]. Tissue transfer from the palm is non-limiting to the patient. This report describes new volar skin flaps for reconstruction of soft tissue defects of the digits.
2. Patients and Method
Two reverse volar flaps i.e. radialis indicis artery (RIA) flap and common palmar digital artery (CPDA) flap, were performed from 2010 to 2014 for reconstruction of posttraumatic soft tissue loss on the index and middle finger distal phalanx (Table 1). All patients were male, manual workers, aged 21–55 (mean age 33.6). The injury mechanisms were avulsion and crush. The defect size ranged from 1.8 cm × 2.6 cm to 1.6 cm × 3 .7 cm.
3. Surgical Technique
Surgery was performed under axillary block with the aid of tourniquet control (250–300 mmHg) and loupe magnification (6). On the basis of anatomical studies, we considered the possibility of drawing the flap’s skin paddle on the first web space and mid palmar region according to the injury. The new flaps was based on the radialis indicis artery and common palmar digital artery and was used to reconstruct the distal index and middle finger injuries.
Designing of radialis indicis artery flap: The radialis indicis artery was found out on the palm of the index proximal phalanx from the MPJ to the PIPJ, and we identified the communicating branches of skin proximally. After identifying the radialis indicis artery from the princeps pollicis artery in the first web space, its proximal end was ligated and cut it there. After ligating the communicating branches between the superficial palmar arch and the radialis indicis artery, we cut it. The flap is transferred into the index finger soft tissue defect, leaving the pedicle intact, and it was sutured. Designing of Common palmar digital artery island flap: The common palmar digital artery from superficial palmar arch was identified in mid palmar region between index and middle finger, it’s both sides were ligated, leaving it intact and was cut. Incision was extended on the radial side of the proximal phalanx of the middle finger peripherally and was detached the common palmar digital artery up to the second web space. Finally the lateral aspect of middle finger was incised, the flap containing the pedicle consisted of common palmar digital artery attached to the recipient area along to the incision groove in depth of subcutaneous fatty tissue and sutured.
The reverse flow flap was supplied by the distal deep communications between the proper palmar digital arteries [31, 32, 33]. It has been shown that Distal anastomatic branches between proper palmar digital arteries and common palmar digital arteries are connected through a deep vascular network which allowed the reverse blood flow to feed the pedicle flap. (Figure: 1, 2). The donor site was covered with split thickness skin graft. Sensory functions of the index and middle finger were assessed using the static 2-point discrimination test.
4. Results
Clinical data are summarized in (Table: 1). The flap size ranged from 1.8 cm x 2.6 cm to 1.6 cm x 3.7 cm. All flaps survived totally and skin grafts healed without adverse events. Moreover, all patients maintained the fingers original length and used it without difficulty. The mean static 2-point discrimination in the distal portion of the flap ranged from 6 to 8 mm.
|
Case |
Age |
Gender |
Side |
Type of Injury |
Defect Size (cm) |
Flap Size (cm) |
Pedicle Length (cm) |
AJ ROM |
Result |
|
1 |
25 |
M |
RIF |
Avulsion |
1.8×2.6 |
2.2×2.8 |
2.5 |
Complete |
Good |
|
2 |
21 |
M |
LIF |
Avulsion |
1.8×3.4 |
2×3.4 |
2.8 |
Complete |
Good |
|
3 |
28 |
M |
RMF |
Crush |
2×2.8 |
2.3×2.8 |
3.4 |
Complete |
Good |
|
4 |
42 |
M |
RMF |
Avulsion |
1..8×3 |
1.8×3.5 |
3.4 |
Complete |
Good |
|
5 |
48 |
M |
RIF |
Crush |
1.6×3.3 |
2×3.5 |
2.8 |
Complete |
Partial necrosis |
|
6 |
36 |
M |
LMF |
Crush |
2×3.5 |
2.2×3.5 |
3.7 |
Complete |
Good |
|
7 |
39 |
M |
RMF |
Crush |
2×3.5 |
2.3×3.7 |
3.3 |
Complete |
Good |
|
8 |
55 |
M |
RMF |
Avulsion |
1.6×2.8 |
2×3 |
3.6 |
Complete |
Good |
|
9 |
27 |
M |
RMF |
Avulsion |
1.6×3 |
1.8×3.2 |
4 |
Complete |
Good |
|
10 |
26 |
M |
RIF |
Crush |
1.8×2.8 |
2×2.8 |
2.3 |
Complete |
Good |
|
11 |
26 |
M |
RIF |
Crush |
2.2×2.8 |
2.2×3 |
2.4 |
Complete |
Good |
|
12 |
33 |
M |
RMF |
Crush |
2×2.8 |
2.2×2.8 |
3.5 |
Complete |
Good |
|
13 |
31 |
M |
RMF |
Crush |
1.6×3.6 |
1.8×3.6 |
3.4 |
Complete |
Good |
|
Average |
33.6 |
1.83×3.07 |
2.06×3.2 |
3.16 |
Complete |
Good |
|||
M-male, RIF-right index finger, RMF-right middle finger, LIF-left index finger, LMF-left middle finger, AJ ROM-
adjacent joint range of motion.
Table 1: Patient data.
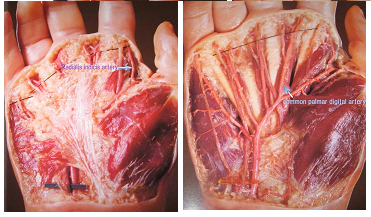
Figure 1: Vascular anatomy in the volar region. a) Radialis indicis artery; b) Common palmar digital artery.
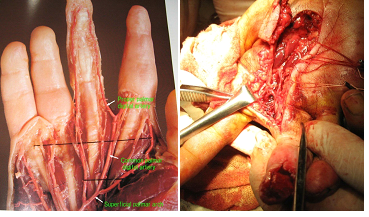
Figure 2: a) Distal anastomatic branches between proper palmar digital arteries and common palmar digital arteries; b) CPDA (common palmar digital artery) flap.
5. Discussion
There are multiple options for soft tissue reconstruction of the upper limb that can restore function in addition to stable coverage. Several local and regional flaps have been identified including advancement flap, rotation flaps in cases where local tissue is available and healthy. Pedicle flaps for soft tissue reconstruction for the upper extremity offer flap versatility, the ability to match color and texture of the recipient site, coverage of vital structures with minimal donor site morbidity. The primary goal of reconstructing finger injuries is restoration of function and sensation by covering the defect with a skin flap without bone shortening [34]. Although several surgical techniques are available for reconstruction, injury treatment remains challenging. Most of the flaps used in the finger soft tissue reconstruction are not perfect. The use of local flaps such as transposition, rotation, and advancement flaps with random vascularization is restricted because of the limited range of flap mobility and the scarce availability of healthy skin from nearby areas [35, 36]. The cross-finger flap requires two stage procedures and has constraints like a considerable immobilization period, with the consequent risk of joint stiffness, and limited arc of transposition. During the last decade the hand arterial network and the communication between the palmar and dorsal vessels have been more clearly understood [37, 38], therefore several new flaps have been described and the hand dorsum has been used more frequently to cover soft-tissue defects of the hand and fingers. The ideal replacement for volar skin loss on the digits should provide padding or cushion, have a good color and texture match, be sensate or have potential to be sensate, resilient, maintain length and not limit motion. Therefore skin for coverage of defects on the volar surface of the digits should ideally be imported from sources of ‘like tissue’ (i.e. glabrous skin) namely the same or adjacent digits, palm and soles of the feet.
6. Conclusion
Volar flaps has many advantages, approaching ideal replacement for the volar tissues of the fingers, excellent tissue match, minimal donor site morbidity, non-sacrifice of a major vessel, can be made ‘sensory’, neurotises well.
It is interesting that without neurorrhaphy, there has been significant functional sensory recovery, as previously shown in pedicled thenar flaps and distal thenar perforator based island flap [39]. This is as a result of neurotization and is likely better because of the proximity of the donor site to the recipient bed with an excellent tissue match and a high density of nerve receptors on the tips of the digits. We therefore routinely do not find any nerve anastomosis essential both in the pedicled version of the flap [40]. The advantages of this procedure include preservation of the finger length, restoration of sensation, unrestricted hand function with early mobilization, and it has one stage procedure. We believe soft tissue reconstruction of digit by reverse-flow volar flaps are reliable technique for reconstruction of full-thickness pulp defects of the fingers with sensible soft- tissue coverage.
References
- Simsek T, Engin MS, Aslan O, et al. Finger pulp reconstruction with free dorsoulnar artery perforator (DUAP) flap. J Reconstr Microsurg 27 (2011): 543-550.
- Tark KC, Rah DK, Shin KS. Pulp reconstruction of fingers with very small sensate medial plantar free flap. Plast Reconstr Surg 101 (1998): 999-1005.
- Tymchak T. In: Grabb and Smith's Plastic Surgery. Charles H, Ed. Soft tissue reconstruction of the hand. 6th ed. USA: Lippincott Williams and Wilkins (2007).
- Giuseppe Checcucci MD. Reverse flow first dorsal metacarpal artery flap for covering the defect of distal thumb. Microsurgery 34 (2014): 283-286.
- Shepard GH. The use of lateral V-Y advancement flaps for fingertip reconstruction. J Hand Surg Am 8 (1983): 254-259.
- Tuncali D, Barutcu AY, Gokrem S, et al. The hatchet flap for reconstruction of fingertip amputations. Plast Reconstr Surg 117 (2006): 1933-1939.
- Lai CS, Lin SD, Yang CC. The reverse digital artery flap for fingertip reconstruction. Ann Plast Surg 22 (1989): 495-500.
- Flatt AE. The thenar flap. J Bone Joint Surg Br 1957; 39(B):80–85.
- Hastings H II. Dual innervated index to thumb cross finger or island flap reconstruction. Microsurgery 8 (1987): 168-172.
- Shi SM, Lu YP. Island skin flap with neurovascular pedicle from the dorsum of the index finger for reconstruction of the thumb. Microsurgery 15 (1994): 145-148.
- Garg R, Fung BK, Chow SP, et al. A Free thenar flap e a case report. J Orthop Surg Res 2 (2007): 4.
- Levin LS, Erdmann DE. Primary and secondary microvascular reconstruction of the upper extremity. Hand Clinics 17 (2001): 447-455.
- Lister G, Scheker L. Emergency free flaps to the upper extremity. J Hand Surg Am 13 (1988): 22-28.
- Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg 78 (1986): 285-292.
- Tranquilli-Leali Ricostruzione dell’apice delle falangi ungueali mediante autoplastica volare peduncolata per scorrimento. Infort Traum Lavaro 1 (1935): 186-193.
- Atasoy E, Ioakimidis E, Kasdan ML, Kutz JE, Kleinert HE. Reconstruction of the amputated fingertip with a triangular volar flap. A new surgical procedure. J Bone Jt Surg Am 52 (1970): 921-926.
- Commerlad BC, McGrouther DA. Resurfacing the sole: long term follow up and comparison of techniques. Br J Plast Surg 31 (1978): 107-116.
- Levin LS, Seraffin D. Plantar skin coverage. Prob Plast Reconstr Surg 1 (1991): 156-184.
- Venkataswami R, Subramanian N. Amputations of the fingertip and thumb. Plast Reconstr Surg 66 (1980): 296-300.
- Seyhan T. Reverse thenar perforator flap for volar hand reconstruction. J Plast Reconstr Surg 62 (2009): 1309-1316.
- May Jr JW, Chait LA, Cohen BE, et al. Free neurovascular flap from the first web of the foot in hand reconstruction. J Hand Surg 2 (1977): 387-393.
- Minami A, Usui M, Katoh H, et al. Thumb reconstruction by free sensory flaps from the foot using microsurgical tech- niques. J Hand Surg 9 (1984): 239-244.
- Zuker RM, Manktelow RT. The dorsalis pedis free flap: tech- nique of elevation, foot closure and flap application. Plast Reconstr Surg 77 (1986): 93-1102.
- Kato H, Ogino T, Minami A, et al. Restoration of sensibility in fingers repaired with free sensory flaps from the toe. J Hand Surg 14 (1989): 49-54.
- Morrison WA, O’Brien BM. Thumb reconstruction with a free neurovascular wrap around flap from the big toe. J Hand Surg 5 (1980): 575-583.
- Turner A, Ragowannsi R, Hanna J, et al. Microvascular soft tissue reconstruction of the digits. J Plast Reconstr Aesthet Surg 59 (2006): 441-450.
- Tsai TM, Sabapathy SR, Martin D. Revascularisation of a finger with a thenar mini-free flap. J Hand Surg Am 16 (1991): 604-606.
- Kamei K, Shimada K, Kimura T, et al. Substantial volar defects of the fingers treated with free thenar flaps. Scand J Plast Reconstr Surg Hand Surg 31 (1997): 87-90.
- Pilz SM, Valenti PP, Harguindeguy ED. Free sensory or retro- grade pedicled fasciocutaneous thenar flap: anatomic study and clinical application. Handchir Mikrochir Plast Chir 29 (1997): 243-246.
- Sassu P, Lin CH, Lin YT, et al. Fourteen cases of free thenar flap: a rare indication in digital reconstruction. Ann Plast Surg 60 (2008): 260-266.
- Fortune C. Iwuagwu. Reconstruction of volar skin and soft tissue defects of the digits including the pulp: Experience with the free SUPBRA flap. Journal of Plastic, Reconstructive & Aesthetic Surgery 68 (2015): 26-34.
- Brunelli Le lambeau dorso-cubital du pouce. Ann Chir Main 12 (1993): 105-114.
- Earley MJ. The arterial supply of the thumb, first web and index fin- ger and its surgical application. J Hand Surg Br 11 (1986):163-174.
- Shao X, ChenC, Zhang X, Ren D, Lu L. Coverage of fingertip defect using a dorsal island pedicle flap including both dorsal digital nerves. J Hand Surg Am 34 (2009): 1474-1481.
- Zhang X, He Y, Shao X, Yi Y, Wen S, Zhu H. Second dorsal meta- carpal artery flap from the dorsum of the middle finger for coverage of volar thumb defect. J Hand Surg A 2008; 34:1467–1473.
- El-Khatib HA. Clinical experiences with the extended first dorsal metacarpal artery island flap for thumb reconstruction. J Hand Surg Am 23 (1998): 647-652.
- Sherif MM. First dorsal metacarpal artery flap in hand reconstruction. J Hand Surg Am 19 91994): 26-31.
- Dautel G, Merle M, Borrelly J, et al. Variations anatomiques du reseau vasculaire de la premiere commessure dorsale:applications au lambeau cerf-volant. Ann Chir Main 8 (1989): 53- 59.
- Melone Jr CP, Beasely RW, Carstens Jr JH. The thenar flap: an analysis of its use in 150 cases. J Hand Surg 7 (1982): 291-297.
- Iwuagwu F, Siddiqui A. Pedicled (antegrade) SUPBRA flap e for wound cover on volar aspect of thumb. J Plast Reconstr Aes- thet Surg 65 (2012): 678-680.
