Clinical Significance of Fetal Echocardiography in Diagnosing Congenital Cardiac Anomalies: An Experience From Eastern India
Article Information
Nurul Islam1, Siddhartha Saha1*, Tasdiqul Islam2, Jheelam Mukherjee3, Mahua Roy4
1Dept of Pediatric Cardiology, Health World Hospitals, Durgapur, West Bengal, India
2Consultant Radiologist, Kolkata, India
3Dept of Obs and Gynae, Health World Hospitals, Durgapur, India
4Paediatric Cardiology, R N Tagore International Institute of Cardiac Sciences, Kolkata, India
*Corresponding Author: Siddhartha Saha.Consultant, Dept of Pediatric Cardiology, Health World Hospitals, Durgapur, West Bengal, India.
Received: 20 April2023;Accepted: 27 April 2023;Published: 08 May 2023
Citation: Nurul Islam, Siddhartha Saha, Tasdiqul Islam, Jheelam Mukherjee, Mahua Roy. Clinical Significance of Fetal Echocardiography in Diagnosing Congenital Cardiac Anomalies: an Experience from Eastern India. Journal of Radiology and Clinical Imaging. 6 (2023): 107-117
View / Download Pdf Share at FacebookAbstract
Background: The role of early diagnosis of fetal cardiac abnormalities (both structural and functional) on the postnatal outcome has been controversial in literature for decade. Our objective was to evaluate the role of fetal echocardiography (FE) as a diagnostic tool for early detection of fetal cardiac abnormalities and its appropriate management plan.
Results: This is a cross-sectional analytical and descriptive study that included 4366 singleton pregnant women (4366 fetuses) referred for FE from 2014 to 2022. Indications for referral and perinatal risk factors were documented. FE and postnatal transthoracic echocardiography were done. Maximum number of fetal echo done for the indication of presence of ICEF (1538, 35.2%).Routine FE done in 1199 (27.5%) individual. In 501(11.5%) individual had bad obstetric history. Fetal cardiac abnormalities were detected in 175 fetuses (4%). CHDs in 149 (3.4%), fetal arrhythmia in 17 (0.4%)cardiomyopathy in 3 (0.07%) fetuses and cardiac mass (Rhabdomyoma) in 6 fetuses (0.14%). Of the structural CHDs, maximum number of cases were large VSD, found in 24 (13.7%) cases, Four cases with tiny muscular ventricular septal defects and two cases with coarctation of aorta, one case of TGA with IVS and one case of large VSD were missed by FE and were diagnosed postnatal. Six cases of critical congenital heart disease were underwent early lifesaving neonatal intervention.
Conclusions: FE can accurately diagnose most of the cardiac anomalies though few errors remain challenging (aortic coarctation). It also offers a good chance for successful early life saving management of some types of cardiac lesions.
Keywords
Congenital heart disease;Fetal echocardiography
Congenital heart disease articles Congenital heart disease Research articles Congenital heart disease review articles Congenital heart disease PubMed articles Congenital heart disease PubMed Central articles Congenital heart disease 2023 articles Congenital heart disease 2024 articles Congenital heart disease Scopus articles Congenital heart disease impact factor journals Congenital heart disease Scopus journals Congenital heart disease PubMed journals Congenital heart disease medical journals Congenital heart disease free journals Congenital heart disease best journals Congenital heart disease top journals Congenital heart disease free medical journals Congenital heart disease famous journals Congenital heart disease Google Scholar indexed journals Fetal echocardiography articles Fetal echocardiography Research articles Fetal echocardiography review articles Fetal echocardiography PubMed articles Fetal echocardiography PubMed Central articles Fetal echocardiography 2023 articles Fetal echocardiography 2024 articles Fetal echocardiography Scopus articles Fetal echocardiography impact factor journals Fetal echocardiography Scopus journals Fetal echocardiography PubMed journals Fetal echocardiography medical journals Fetal echocardiography free journals Fetal echocardiography best journals Fetal echocardiography top journals Fetal echocardiography free medical journals Fetal echocardiography famous journals Fetal echocardiography Google Scholar indexed journals cardiomyopathy articles cardiomyopathy Research articles cardiomyopathy review articles cardiomyopathy PubMed articles cardiomyopathy PubMed Central articles cardiomyopathy 2023 articles cardiomyopathy 2024 articles cardiomyopathy Scopus articles cardiomyopathy impact factor journals cardiomyopathy Scopus journals cardiomyopathy PubMed journals cardiomyopathy medical journals cardiomyopathy free journals cardiomyopathy best journals cardiomyopathy top journals cardiomyopathy free medical journals cardiomyopathy famous journals cardiomyopathy Google Scholar indexed journals gestational age articles gestational age Research articles gestational age review articles gestational age PubMed articles gestational age PubMed Central articles gestational age 2023 articles gestational age 2024 articles gestational age Scopus articles gestational age impact factor journals gestational age Scopus journals gestational age PubMed journals gestational age medical journals gestational age free journals gestational age best journals gestational age top journals gestational age free medical journals gestational age famous journals gestational age Google Scholar indexed journals In vitro fertilization articles In vitro fertilization Research articles In vitro fertilization review articles In vitro fertilization PubMed articles In vitro fertilization PubMed Central articles In vitro fertilization 2023 articles In vitro fertilization 2024 articles In vitro fertilization Scopus articles In vitro fertilization impact factor journals In vitro fertilization Scopus journals In vitro fertilization PubMed journals In vitro fertilization medical journals In vitro fertilization free journals In vitro fertilization best journals In vitro fertilization top journals In vitro fertilization free medical journals In vitro fertilization famous journals In vitro fertilization Google Scholar indexed journals color flow articles color flow Research articles color flow review articles color flow PubMed articles color flow PubMed Central articles color flow 2023 articles color flow 2024 articles color flow Scopus articles color flow impact factor journals color flow Scopus journals color flow PubMed journals color flow medical journals color flow free journals color flow best journals color flow top journals color flow free medical journals color flow famous journals color flow Google Scholar indexed journals Neonatal echocardiography articles Neonatal echocardiography Research articles Neonatal echocardiography review articles Neonatal echocardiography PubMed articles Neonatal echocardiography PubMed Central articles Neonatal echocardiography 2023 articles Neonatal echocardiography 2024 articles Neonatal echocardiography Scopus articles Neonatal echocardiography impact factor journals Neonatal echocardiography Scopus journals Neonatal echocardiography PubMed journals Neonatal echocardiography medical journals Neonatal echocardiography free journals Neonatal echocardiography best journals Neonatal echocardiography top journals Neonatal echocardiography free medical journals Neonatal echocardiography famous journals Neonatal echocardiography Google Scholar indexed journals Tetralogy of Fallot articles Tetralogy of Fallot Research articles Tetralogy of Fallot review articles Tetralogy of Fallot PubMed articles Tetralogy of Fallot PubMed Central articles Tetralogy of Fallot 2023 articles Tetralogy of Fallot 2024 articles Tetralogy of Fallot Scopus articles Tetralogy of Fallot impact factor journals Tetralogy of Fallot Scopus journals Tetralogy of Fallot PubMed journals Tetralogy of Fallot medical journals Tetralogy of Fallot free journals Tetralogy of Fallot best journals Tetralogy of Fallot top journals Tetralogy of Fallot free medical journals Tetralogy of Fallot famous journals Tetralogy of Fallot Google Scholar indexed journals double outlet right ventricle articles double outlet right ventricle Research articles double outlet right ventricle review articles double outlet right ventricle PubMed articles double outlet right ventricle PubMed Central articles double outlet right ventricle 2023 articles double outlet right ventricle 2024 articles double outlet right ventricle Scopus articles double outlet right ventricle impact factor journals double outlet right ventricle Scopus journals double outlet right ventricle PubMed journals double outlet right ventricle medical journals double outlet right ventricle free journals double outlet right ventricle best journals double outlet right ventricle top journals double outlet right ventricle free medical journals double outlet right ventricle famous journals double outlet right ventricle Google Scholar indexed journals Severe aortic stenosis articles Severe aortic stenosis Research articles Severe aortic stenosis review articles Severe aortic stenosis PubMed articles Severe aortic stenosis PubMed Central articles Severe aortic stenosis 2023 articles Severe aortic stenosis 2024 articles Severe aortic stenosis Scopus articles Severe aortic stenosis impact factor journals Severe aortic stenosis Scopus journals Severe aortic stenosis PubMed journals Severe aortic stenosis medical journals Severe aortic stenosis free journals Severe aortic stenosis best journals Severe aortic stenosis top journals Severe aortic stenosis free medical journals Severe aortic stenosis famous journals Severe aortic stenosis Google Scholar indexed journals
Article Details
1. Background
Congenital heart disease (CHD) is the most common congenital anomaly that occurs in 8-12 per 1000 live births [1]. Several risk factors have been incriminated in the pathogenesis of CHD [2]. These include consanguinity [3], maternal medical illnesses [4], teratogenic exposures [5], fetal chromosomal and extra-cardiac abnormalities [6].
The impact of prenatal diagnosis of CHD on the postnatal outcomes has been controversial. Several studies have shown that it decreased neonatal morbidity and mortality; usually of the duct-dependent types [8] as it provides the opportunity for a controlled elective delivery at a tertiary care center with a specialized perinatal cardiac and cardio-thoracic surgical services [9]. Moreover, it helps the detection of concomitant fetal chromosomal and extra-cardiac anomalies, assists in antenatal and postnatal management planning and offers better parental counseling [10]. Other studies found no benefit on neonatal outcomes [11]. Fetal echocardiography (FE) is also the most widely used diagnostic modality for the detection of fetal arrhythmias [12] and evaluation of its consequences such as valve regurgitation, myocardial dysfunction and development of hydrops fetalis [13] FE is used to detect cardiac anomalies in high risk specific cases [14]; though its use as a routine screening tool for all pregnancies is still not well-established [15].
Most of the referrals are still based on the presence of abnormal 4 chamber view on obstetric ultrasound scan, anomaly scan or the presence of a favouring prenatal risk factor despite that only 10% of the affected children have such an identifiable predisposing factor [16]. In this study, our objective was to evaluate the role of fetal echocardiography (FE) as a diagnostic tool for early detection of fetal cardiac abnormalities and its appropriate management plan. We also aimed to study the different kind of indications of referral and find out the perinatal outcome, study the percentages of different type of cardiac anomalies detected in fetal echocardiography and tried to find out discrepancies between anomaly scan and fetal echocardiography as well as tried to calculate sensitivity and specificity of fetal echocardiography in detecting different kind of cardiac anomalies.
2. Methods
This is a cross-sectional analytical and descriptive study that included 4324 pregnant women (4366 fetuses, included singleton and twin) referred for FE from 2014 to 2022. The study was conducted at the Health world hospitals and its outreach clinics and camps conducted for fetal echocardiography. Almost 20% of cases were referred from outreach clinic to our center. Detailed history was taken from all pregnant mothers which included maternal age, obstetric history, gestational age (GA), parity, abortions, still births, assisted reproductive technology like In vitro fertilization(IVF)), and family history of CHD (maternal CHD, other sibling with CHD), chromosomal or other congenital anomalies. Prenatal risk factors were extracted (Maternal medical illnesses, infections, medications). Indications for referral, anomaly scan report and fetal echocardiography diagnosis were reported. Neonatal echocardiography was done for confirmation of FE report; also the management plan and outcome of cardiac anomalies were noted.
2.1 Fetal echocardiography
FE was done for the referred cases to detect any structural or rhythm abnormalities in the fetal heart according to the guidelines and standards of the American Society of Echocardiography for performance of fetal echocardiogram [17] using GE Voluson E6 high-end 4DOB/GYN ultrasound machine and transducer probe with a frequency range of 5-8 MHz, EPIQ CV X made by Philips with transducer 8 MHz. A standard two-dimensional (2D), color flow (CF), Doppler echocardiography examinations were done. Views included four chamber, five chamber, long axis (left and right ventricular outflow), 3 -vessel and tracheal, ductal, and aortic arch views.
Neonatal echocardiography (NE)
NE was done within 72 h of delivery; based on the urgency of each individual case; using Vivid i machine GE Vivid IQ and probe 6SGE ultrasound. EPIQ CV X made by Philips with transducer 8 MHz. Structural CHDs were categorized into common AV canal, ventricular septal defect (VSD), double outlet right ventricle (DORV) with VSD with pulmonary stenosis (PS), Tetralogy of Fallot (TOF), Truncus arteriosus , Tricuspid atresia , Mitral atresia, transposition of great arteries (TGA), corrected transposition of great arteries (CTGA), coarctation of aorta (CoA),hypo plastic left heart syndrome ( HLHS) variant, Severe pulmonary stenosis, Severe aortic stenosis (AS),pulmonary atresia with intact ventricular septum ( PA IVS), Large atrial septal defect (ASD), TOF with absent pulmonary valve, Ebstain anomalies, Hypo plastic right ventricle, Cardiac mass, Endocardial fibro elastosis, Rhythm abnormalities were Complete heart block (CHB), premature atrial contraction (PAC). When abnormalities were found; prognosis and management were discussed with the parents and the referring obstetrician. Arrangement for controlled elective delivery in different tertiary center under the supervision of expert pediatric cardiologists and neonatologists was planned for all fetuses diagnosed with cardiac abnormalities in-utero.
2.2 Statistical analysis
Data were analyzed using Statistical Program for Social Science (SPSS) version 18.0. Quantitative data were expressed as mean. Qualitative data were expressed as frequency and percentage. Sensitivity, specificity, positive and negative predictive values and accuracy of FE were calculated to assess its ability to detect the cardiac abnormality in utero and to detect the same cardiac abnormality in the postnatal period.
3. Results
The study involved 4324 pregnant (both singleton and twin) women (4366 fetuses) whose ages ranged from 18 years to 45 years. All the referred cases had undergone routine obstetric ultrasound before referral to detect multiple gestation and to diagnose any extra- cardiac abnormality such as hydrops fetalis, poly or oligohydramnios, increased first trimester nuchal translucency, abnormal fetal heart beats and abnormal four and five chamber views, Intracardiac echogenic focus (ICEF), single umbilical artery, cardiac mass, abnormal cardiac position. The timing of the anomaly scan ranged from 16 to 32 weeks with a mean of 20weeks. Their gestational age (GA) at referral for FE ranged from 16 to 34 weeks with a mean of 23 weeks.
Table: 1: Indications for referrals and perinatal risk factors
|
Indications for Fetal Echocardiography |
Number |
Percentage |
|
Routine |
1199 |
27.5 |
|
ICEF |
1538 |
35.2 |
|
Maternal illness (GDM+other illness like RA, SLE etc) |
187 |
4.2 |
|
IVF |
100 |
2.2 |
|
Bad obstetric history including advanced maternal age, unexplained previous fetal death |
501 |
11.5 |
|
Single umbilical artery |
76 |
1.7 |
|
Other extra cardiac defect |
178 |
4 |
|
Fetal cardiac anomaly suspected by sonologist |
263 |
6 |
|
Fetal heart rhythm abnormalities defected by sonologist |
29 |
0.6 |
|
Maternal CHD |
47 |
1 |
|
Other baby with CHD |
164 |
3.7 |
|
CHD in family |
23 |
0.5 |
|
Fetal poly/oligohydromnios, IUGR |
19 |
0.3 |
|
Twin |
42 |
1 |
Maximum number of fetal echo done for the indication of presence of ICEF (1538, 35.2%).Routine FE done in 1199 (27.5%) individual. In 501(11.5%) individual had bad obstetric history including advanced age of conception, unexplained previous neonatal death. In vitro fertilization (IVF) was indication for FE in 100 (2.2%) cases. Fetal cardiac structural anomalies and rhythm abnormalities were suspected by sinologist in 263 (6%) and 29 (0.6%) cases respectively. Other fetal anomalies like oligohydramnios, polyhydramnios, IUGR were in 19 (0.3%) cases and twin pregnancy was indication in 42 (1%) case. Single umbilical artery was indication in 76 (1.7%) cases. Mother with CHD, other sibling with CHD and family history of CHD were indications in 47 (1%), 164 (3.7%), and 23 (0.5%) cases respectively
Table 2: Discrepancies between anomaly scan, FE and post-natal echocardiography
|
Fetal Echocardiography |
Anomaly scan |
Post-natal assessment (done only those cases who were not lost in follow up) |
|
|
Conotruncal anomalies (TOF and its variant, Truncusarteriosus) |
Normal scan in 7 cases out of 21 |
FE diagnosis was confirmed in all cases |
|
|
AVSD (complete and partial) |
Normal scan in 5 cases out of 15 cases |
Confirmed in follow up cases |
|
|
DORV+VSD with or without PS |
Normal scan in 1 case out of 8 cases |
Confirmed in follow up cases |
|
|
Large VSD |
4 normal in anomaly scan out of 19+5 cases |
5 cases of large VSD were suspected by anomaly scan but ruled out by FE |
One case missed by FE |
|
Small VSD |
All were normal in anomaly scan out of 15+2 cases |
6 cases of small VSD were suspected by anomaly scan but ruled out by FE |
Four cases missed by FE |
|
VSD with pulmonary atresia |
Two cases were detected by anomaly scan out of 4 cases |
Confirmed in follow up cases |
|
|
Pulmonary atresia intact ventricular septum |
Two normal in anomaly scan out of 6 cases |
Confirmed in follow up cases |
|
|
TGA |
3 were normal in anomaly scan out of 6 cases |
One case missed by FE |
|
|
C TGA |
No case detected by anomaly scan out of 1 case |
Confirmed in follow up cases |
|
|
Tricuspid atresia |
One normal in anomaly scan out of 7 cases |
Confirmed in follow up cases |
|
|
Mitral atresia |
One normal in anomaly scan out of 2 cases |
Confirmed in follow up cases |
|
|
Critical AS |
One normal in anomaly scan out of 3 cases |
Confirmed in follow up cases |
|
|
Critical PS |
3 cases detected in anomaly scan out of 4 cases |
Confirmed in follow up cases |
|
|
CoA |
No case detected in anomaly scan out of 7 cases |
Two cases missed by FE |
|
|
ASD |
3 case detected by anomaly scan out of 3+5 cases |
Two cases were suspected by anomaly scan but ruled out by FE |
Confirmed in follow up cases |
|
Other cardiac anomalies like complex single ventricle (HLHS, HRHS,)Ebstain anomaly, endocardial fibro elastosis, DCM,Cardiac mass, rhythm anomalies |
All cases were suspected in anomaly scan, and confirmed by FE |
Confirmed in follow up cases |
Table 2 shows that among 21 cases of conotruncal anomalies diagnosed by fetal echocardiography (all of them confirmed by post-natal echocardiography), 7 cases were missed in anomaly scan. In AVSD (both complete and partial) out of 15 cases 10 were correctly picked up by anomaly scan. In case of large VSD out of 24 cases only 4 cases were missed in anomaly scan, but in contrary all small VSD cases were missed in anomaly scan. In DORV with VSD only one case was missed in anomaly scan out of 8 cases, whereas 50% cases (2 out of 4 cases) were missed in anomaly scan in case of VSD with pulmonary atresia. Among six cases of PA intact IVS and TGA with intact IVS each,2 and 3 cases were missed respectively by anomaly scan. One case in each was missed in anomaly scan in Tricuspid atresia, mitral atresia, critical AS and critical PS cases among 7, 2, 3, and 4 of total cases detected by FE respectively. None of the cases of CoA were detected by anomaly scan, whereas all cases of HLHS, HRHS, CTGA and cardiac masses were detected by anomaly scan.
Table 3: Different cardiac diagnosis by fetal echocardiography
|
FE diagnosis |
Number |
Percentage |
|
Large VSD |
24 |
13.7 |
|
Small VSD |
17 |
9.7 |
|
TOF |
14 |
8 |
|
TOF with absent PV syndrome |
3 |
1.7 |
|
VSD PA |
4 |
2.2 |
|
Truncusarteriosus |
4 |
2.2 |
|
Tricuspid atresia |
7 |
4 |
|
Mitral atresia |
2 |
1 |
|
Large ASD |
8 |
4.6 |
|
Complete AVSD |
13 |
7.4 |
|
Partial AVSD |
2 |
1 |
|
TGA with intact IVS |
6 |
3.4 |
|
CTGA |
1 |
0.5 |
|
Pulmonary atresia with intact IVS |
6 |
3.4 |
|
Critical AS |
3 |
1.7 |
|
Critical PS |
4 |
2.2 |
|
CoA |
8 |
4.6 |
|
Ebstain anomaly |
1 |
0.5 |
|
Endocardial fibro elastosis |
1 |
0.5 |
|
DORV with VSD |
3 |
1.7 |
|
DORV+VSD+PS |
4 |
2.2 |
|
DORV+VSD+PA |
1 |
0.5 |
|
HLHS |
11 |
6.3 |
|
HRHS |
2 |
1 |
|
Cardiac mass |
6 |
3.4 |
|
DCM |
3 |
1.7 |
|
Complete heart block |
4 |
2.2 |
|
Premature atrial contraction |
13 |
7.4 |
Difficulties in obtaining adequate echocardiographic views were encountered in only 33 cases; twenty-five of them due to the anterior position of the fetal vertebral column obscuring the view, eight cases due to maternal obesity and one case due to inappropriate timing (late referral). Fetal cardiac abnormalities were detected in 175 fetuses (4%). Among them structural CHDs in 149 (3.4%), fetal arrhythmia in 17 (0.4%)cardiomyopathy in 3 (0.07%) fetuses and cardiac mass (Rhabdomyoma) in 6 fetuses (0.14%). Of the structural CHDs, maximum number of cases were large VSD (Fig1), found in 24 (13.7%) cases. Small VSD found in 17 (9.7%) cases, TOF in 14(8%) cases (Fig2). Whereas VSD and pulmonary atresia in 4 (2.2%) cases, TOF variant like TOF with absent pulmonary valve syndrome (APVS) in 3(1.7%) cases. Complete AVSD (Fig3)and partial AVSD were found in 13(7.4%) and 2 (1%) cases respectively. Quite a large number,11 (6.3%) of cases of HLHS were found. Large ASD and CoA (Fig4) were found in 8 (4.6%) cases each. We found 6 (3.4%) cases each of TGA intact IVS (Fig5), PA intact IVS and cardiac mass. Tricuspid atresia, mitral atresia was found in 7 (2.2%) and 2 (1%) cases respectively. DORV with VSD, DORV with VSD and PS, DORV with VSD and PA were found in 3 (1.7%).4(2.2%) and 1(0.5%) cases respectively. DCM were found in 3 (1.7%) cases. All other cases like Ebstain anomaly, endocardial-fibro-elastosis, CTGA were found in less than 1% cases each.
Of the fetal arrhythmias, 13 fetuses had premature atrial contraction, and 4 fetuses had congenital heart block
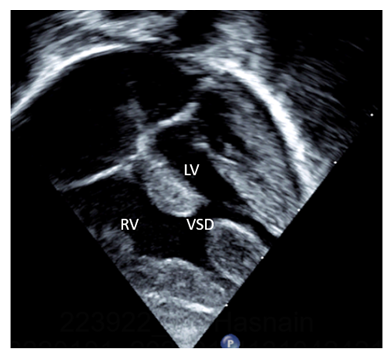
Figure 1: Large mid muscular VSD
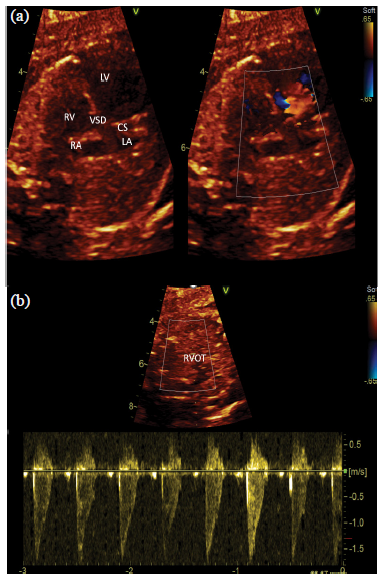
Figure 2 :(a) Large malaligned Perimembraneous VSD (b) Increase pulmonary valve velocity suggestive of Tetralogy of Fallot
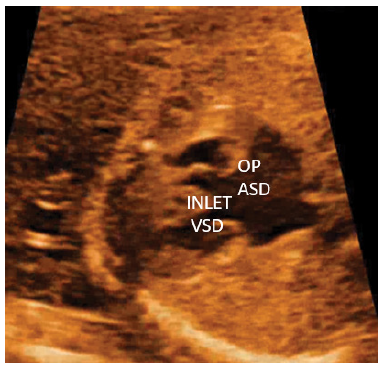
Figure 3: Large OP ASD and large inlet VSD suggestive of complete Atrio-Ventricular septal defect
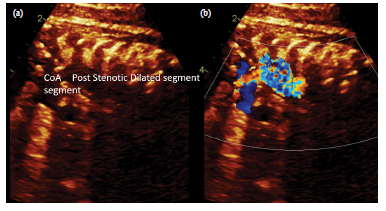
Figure 4: (a) Coarctation of Aorta segment with post stenotic dilatation (b) Terbulence across coarct segment.
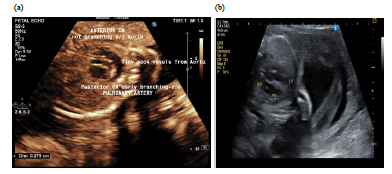
Figure 5: (a) Anterior great artery giving neck vessels suggestive of aorta, posterior great artery early branching suggestive of pulmonary artery.
(b) Aorta arising from RV and pulmonary artery arising from LV suggestive of Transposition of Great arteries (TGA)
3.1 Decision and outcome
The decisions taken regarding fetuses with CHD were watchful follow up and arranging for elective delivery in any tertiary care center which offers highly qualified cardiac and cardiothoracic services. Of the total number of abnormal fetal echocardiography lost to follow up occurred in 65 cases, (IUFD) in 1 cases, and elective termination in 16 case (11 cases of HLHS, 1 case of mitral atresia, 1 case of TGA intact IVS, 3 cases of VSD PA), Total nine cases (one critical AS, two critical PS, five PA intact IVS, one TGA intact IVS) were identified with cardiac lesions required early post-natal intervention. but number of cases actually underwent intervention early in post-natal life was six. Four cases of pulmonary atresia with intact ventricular septum underwent ductal stenting, one case of TGA with intact IVS underwent septostomy, and one case of critical PS was undergone for neonatal BPV.
All the six cases of cardiac mass were found to be rhabdomyoma, one of them diagnosed as having Tuberous Sclerosis, in three cases tumors were getting regressed in follow up, two cases were lost in follow up after neonatal echocardiography. No cardiac mass patients required any kind of surgery or chemotherapy. Among the four cases of complete heart block, one was required permanent pacemaker implantation (PPI), two on oral medication and one was lost in follow up after initial neonatal examination. None of the PAC required any kind of treatment. Among 3 cases of DCM, two patients are on medical management and one case was lost to follow up.
Table 4: Comparison between fetal and postnatal echocardiography
Table 4 shows the sensitivity, specificity, predictive values and accuracy of FE in the diagnosis of each of the specific fetal cardiac abnormalities (after excluding cases that were died which include both IUFD and still birth, electively terminated and cases who were lost in follow up). 65 cases out of 175 cases were lost to follow up. Four cases with tiny muscular ventricular septal defects and two cases with coarctation of aorta, one case of TGA with IVS and one case of large VSD were missed by FE and were diagnosed postnatal. In case of TGA and IVS and large VSD fetal echo was done at an advanced gestational age, so the window was poor. The routine obstetric US scan of the case with aortic coarctation was done at 19 weeks’ gestation and was unsuspicious of any cardiac abnormalities. The case was referred for FE in the view of bad obstetric history (maternal history of multiple previous abortions). FE was done at the age of 20 weeks’ gestation and revealed mild dilatation of the left ventricle. A second look was decided for the case to monitor the disease progression but the mother did not return back for follow up until after delivery when NE revealed coarctation. Another fetus with CoA, where FE done at very early gestation, and that case was missed in FE. One case of large VSD was missed in FE, in that case fetal echocardiography was done in very advanced (34 weeks of GA) pregnancy. One case of DORV type of VSD with PS diagnosed by FE was turned to be DORV type of VSD with pulmonary atresia in neonatal echocardiography, because of progressive nature of the disease. This highlights the importance of follow up FE in progressive cardiac lesions. Almost in all cardiac lesions FE showed 100% sensitivity, specificity, PPV and NPV, except in TGA IVS (sensitivity:87.5%), CoA and small VSD (sensitivity:80%) and large VSD cases (sensitivity:95%).
4. Discussion
In our center; almost all pregnant women undergo a minimum of one anomaly scan that includes fetal heart scanning based on the four chamber and outflow views to screen for CHD. A detailed FE scanning by an expert pediatric cardiologist is indicated when findings in these views do not fulfill the normal criteria [18] or any other risk factors associated with pregnancy that might cause CHD in fetus. Deviation from normality in anomaly scan as per cardiac point of view includes ICEF, abnormal cardiac position or axis, chamber dilatation and or asymmetry, cardiomegaly, outflow tract abnormalities and fetal arrhythmia [19]. Obtaining only a normal four chamber view and outflow view are still not sufficient to exclude underlying cardiac anomalies [20], hence; the anomaly scan may not be the ideal tool to screen for fetal cardiac abnormalities [21]. FE is more sensitive and more specific in the prenatal detection of CHD when compared to the routine obstetric scanning or anomaly scan that can miss a large number of cases [22]. In a study done by Archiron et al. [23], the rate of detection of CHD was raised from 48%; when relying on the four chamber view alone; to 78% when other views were incorporated. Similarly, Carvalho et al. [24] reported a detection rate of 75% with extended screening. In this series, discrepancies between the anomaly scan and the FE were encountered in 35 hemodynamically significant cases (small VSDs are not included). In all 35 cases showed positive findings by FE though their anomaly scan was marked as "Normal". This highlights the need to raise the awareness of the obstetricians and the obstetric ultra- sonographers that limited screening of the fetal heart by the 4 chamber (sometimes with outflow view) view may not be sufficient to totally exclude an underlying fetal cardiac abnormality.
In this series, maximum cases (35.2%) were referred for ICEF on routine obstetric ultrasound, only 6% of cases are referred for suspicion of CHD by sonologist on the basis of abnormal 4 chamber view or outflow tract view in anomaly scan and 0.6% cases were referred for abnormal cardiac rhythm. In a study done by Meyer-Wittkopf et al. [18], cases referred on basis of suspicious cardiac configuration and abnormal fetal rhythm were (26%) and (5.7%) of their studied population respectively and the percentage of FE scans confirmed positive for CHD was 78%. Also in a study done by Chitra and Vijayalakshmi [25], abnormal obstetric scan was the indication of referral in 26.8% of their studied population. This highlights the role of obstetric US scanning as an important screening tool for fetal structural and rhythm abnormalities, though; unfortunately, we were not able to compare between the accuracy of the obstetric and the FE scanning as most of the referral letters included ICEF or “abnormal cardiac views” without mentioning a definitive provisional diagnosis. Currently, FE is reserved for high risk pregnancies where higher incidence of CHD is traditionally expected [22], our study also reflects that a large number of pregnant women referred for FE for their bad obstetric history (11.5%), history of maternal illness (4.2%), and history of CHD in mother (1%) or sibling (3.7%) or in family (0.5%). Although; previous studies reported that most of the cases of CHDs occur in low risk population with no identifiable prenatal risk factors [7, 16, 26].
The ideal timing for prenatal echocardiography is 18-22 weeks’ gestation [17]. In this series, the mean value of gestational age on first FE scanning was 23 weeks. This compares favorably with previous studies [25, 27, 28].
In this study fetal cardiac abnormalities were detected in 175 fetuses (4%). CHDs in 149 (3.4%), fetal arrhythmia in 17 (0.4%) cardiomyopathy in 3 (0.07%) fetuses and cardiac mass (Rhabdomyoma) in 6 fetuses (0.14%). Of the structural CHDs, maximum number of cases were large VSD, found in 24 (13.7%) cases, small VSD in 17 (9.7%) cases, TOF in 14(8%)cases, whereas VSD and pulmonary atresia in 4 (2.2%) cases, TOF variant like TOF with APVS in 3(1.7%) cases. Complete AVSD and partial AVSD were found in 13(7.4%) and 2 (1%) cases respectively. Quite a large number,11 (6.3%) of cases of HLHS were found. Large ASD and CoA were found in 8 (4.6%) cases in each. We found 6 (3.4%) cases each in TGA with intact IVS, PA IVS and cardiac mass. Tricuspid atresia, mitral atresia was found in 7 (2.2%) and 2 (1%) cases respectively. DORV with VSD, DORV with VSD and PS, DORV with VSD and PA were found in 3 (1.7%).4(2.2%) and 1(0.5%) cases respectively. DCM were found in 3 (1.7%) cases. All other cases like Ebstain anomaly, endocardial-fibro-elastosis, CCTGA were found in less than 1% cases each. In their study, Chitra and Vijayalakshmi [25] detected CHD in 18.2%, fetal arrhythmias in 3.6% and rhabdomyomas in 0.6% of their studied population. Among their CHD group, complex lesions were detected in 70% of cases. Also, Meyer-Wittkopf et al. [18] detected CHD in 24.5%. The differences in the detection rate between different studies can be attributed to the significant variations in the incidence of CHD that do exist between different populations belonging to different ethnicities [29].
In a study done by Zhang et al. [30], the sensitivity and specificity of FE in detecting CHD was 68.5% and 99.8% respectively whereas, Soongswang et al. [31] detected sensitivity, specificity, positive predictive value, negative predictive value and accuracy of 96.9%, 90.6%, 84.2%, 98.3% and 92.8% respectively. In this series, postnatal studies revealed that FE was able to diagnose correctly all cases of CHD (conotrunchal anomalies, atrioventricular canal, and complex heart lesions), cardiomyopathy, and cardiac mass after exclusion of cases which lost follow up. We encountered eight false negative diagnoses;
Four cases with tiny muscular ventricular septal defects and two cases with coarctation of aorta, one case of TGA with intact IVS and one case of large VSD were missed by FE and were diagnosed postnatal. Neither of our false negative cases had experienced any deteriorating hemodynamic consequences in the postnatal period and they had come only to medical attention in the view of recruitment for neonatal echocardiography confirmation. One case of DORV type of VSD with PS turned out to be DORV type of VSD with PA postnatal, because of progressive nature of the disease The types of cardiac lesions missed in our study match favorably with the study done by Meyer-Wittkopf et al. [18] who detected a sensitivity of 98% in the prenatal diagnosis of CHD by FE. The difficulty in the prenatal diagnosis of aortic coarctaion is well-known in literature [32] and had been reported in previous studies [33, 34]. This confirms the need for sequential follow up studies as some cardiac lesions have an evolving nature [35].
Fetal arrhythmias account for nearly 10-20% of total referrals for FE [12]. Most of which are in the form of frequent ectopic beats with the atrial ectopics being much more common than those of ventricular origin. Tachyarrythmias are diagnosed when fetal heart rate is above 180 beats per minute. They include sinus, atrial, supraventricular and ventricular tachycardia [36]. Fetal bradyarrythmia are diagnosed when fetal heart rate is persistently below 100 beats per minute which can be due to blocked atrial bigemeny or atrio-ventricular block or sinus bradycardia (rare) [12].
In this series, we detected arrhythmias in 9.6% of the cardiac anomalies. Of the fetal arrythmias, 13 fetuses had premature atrial contraction, and 4 fetuses had congenital heart Among the four cases of complete heart block, one required PPI, two on oral medication and one was lost in follow up after initial neonatal examination. None of the PAC required any kind of treatment Successful treatment of fetal arrhythmia in utero and spontaneous resolution of premature atrial contractions had been also reported by Soongswang et al. [31]. Of their 17 cases diagnosed with fetal arrhythmia, Chitra and Vijayalakshmi [25] reported bradycardia in 10 cases, tachyarrythmias in 5 cases, ectopics in two cases and complete heart block in one case with maternal lupus. They also observed lower association between fetal arrhythmia and underlying structural heart diseases.
Early prenatal diagnoses provide the neonate with a better care in-utero and in the post-natal period. Moreover; it allows for early family counseling which allows the parents to be psychologically and financially prepared to accept such a child [37] as it offers them time to be fully aware of the pathophysiology of the detected anomaly; also the treating physician will have enough time to explain the severity and discuss the prognosis with parents so they can be able to take a decision regarding the course of pregnancy. Missing such cases on routine obstetric scanning or discovering them at late pregnancy would have rendered decision taking more difficult [22]. Management of a neonate with an antenatal diagnosis of CHD necessitates coordinate collaboration between obstetricians, neonatologists, pediatric cardiologists, fetal echo cardiographers and cardio- thoracic surgeons [38, 39].The management plan is tailored for each case putting into consideration the anticipated risk of hemodynamic instability, the available medical resources, presence of feto-maternal complications, the availability and the transportation distance to a specialized cardiac center [39]. Based on our FE findings; delivery in a tertiary care center with availability of pediatric cardiologist for early neonatal echocardiographic confirmation and subsequent management was decided for all cases with hemodynamically significant cardiac abnormalities. Arrangement for future pacemaker was done for congenital heart block. Prevention of termination with strict follow up was the decision taken for cases with expected spontaneous resolution such as ectopic, cardiomyopathy, rhabdomyomas. Early neonatal interventions were done in few cases which were planned and arrangements were made before delivery Termination has been offered in some cases with very complex heart diseases which are not compatible with life.
Some studies have shown that neonates with CHD diagnosed antenatal tend to be born earlier than expected when compared to those diagnosed postnatal [40]. Though, the decision for the delivery timing of a neonate with a prenatal diagnosis of CHD is affected greatly by the presence or absence of maternal or fetal complications, the advantages of term delivery should be always kept in mind [39]. In our study, most of our cases were term deliveries. This reflects the high standard of obstetric care offered to our population.
Study strengths and limitations
Former studies showed that the outcome of neonates who had been diagnosed prenatally with a serious CHD and had consequently been offered an appropriate management in their early neonatal period had shown a better outcome in comparison with those diagnosed in their postnatal period [41]. Unfortunately, based on our study design which lacked a control group, we were not able to compare between pregnant mothers who had undergone prenatal FE and those who had not as regards to the perinatal outcome; hence we reported the outcome of our cases in a descriptive manner rather than a numerical one. Unlike many of the previous studies; it did not only include structural cardiac abnormalities but it also included fetal rhythm abnormalities. Moreover, it highlighted the different varieties of indications for FE and perinatal risk factors frequently encountered in our community. It was limited by the number of cases who did not come for follow up, so postnatal confirmation of the underlying anomaly was not done for all the studied cases.
5. Conclusions
FE can accurately diagnose most of the cardiac anomalies though few errors remain challenging regarding the prenatal diagnosis of aortic coarctation. It also offers a good chance for successful early lifesaving management of some types of CHD. It is important to raise the awareness of the obstetricians and the obstetric-sonographers to refer pregnant mothers for FE in an adequate time when indicated. It is also important to improve the training of the obstetric sonographers to adequately screen for CHD with every follow up visit; owing to the evolving nature of some cardiac lesions; and to refer for FE once suspected. Moreover, there is a growing need to increase the clinical skills of the pediatric cardiologists in the field of FE.
Disclosure of interests:
There is no conflict of interest
Contribution to authorship:
Dr Nurul Islam and Dr Siddhartha Saha: Doing fetal echocardiography at main and peripheral centre, arranging fetal echocardiography camps, planning the study, data collection, family counselling, preparation of master chart, basic write up, ethical committee meeting, statistical analysis, communicating with other co-authors.
Dr Jheelam Mukherjee: Motivating the family for fetal echocardiography test and arranging delivery for high risk cases.Helping in write up and editing
Dr Mahua Roy and Dr Tasdiqul Islam :Doing fetal echocardiography in peripheral clinic and sharing data , helping in write up and editing.
Details of patient's consent:
All the relevant written consent has been taken from patients for publication
Funding:
No funding was needed
Details of ethics approval:
We put the study before ethical committee, as because it was only retrospective observational study, committee allowed us to continue the study without any need for ethical clearance.
Abbreviations
CHD: Congenital heart disease
FE: Fetal echocardiography
IVF: In vitro fertilization
CHB: Complete heart block
PAC: Premature atrial contraction
LV: Left ventricle
RV: Right ventricle
VSD: Ventricular septal defect
ASD: Atrial septal defect
TOF: Tetralogy of Fallot
TGA: Transposition of great arteries
CTGA: Corrected transposition of great arteries
PA: Pulmonary atresia
PS: Pulmonary stenosis
AS: Aortic stenosis
IVS: Interventricular septum
DORV: Double outlet right ventricle
HLHS: Hypoplastic left heart syndrome
HRHS: Hypoplastic right heart syndrome
CoA: Coarctation of aorta
AVSD: Atrioventricularseptal defect
ICEF: Intracardiac echogenic focus
GDM: Gestational diabetes mellitus
SLE: Systemic lupus erythematosus
RA: Rheumatoid arthritis
DCM: Dilated cardiomyopathy
PPI: Permanent pacemaker implantation
References
- Donofrio MT, Moon Grady AJ, Hornberger LK, et al. Diagnosis and treatment of fetal cardiac disease: a scientific statement from the American Heart Association. Circulation 129(21) (2014):2183-2242.
- Hamdan MA, Chedid F, Bekdache GN, et al. Perinatal outcome of congenital heart disease ina population with high consanguinity. J Perinat Med 43(6) (2015):735-740.
- Sheridan E, Wright J, Small N, et al. Risk factors for congenital anomaly in a multiethnic birth cohort: an analysis of the born in Bradford study. Lancet 382(2013):1350-1359.
- Liu S, Joseph KS, Lisonkova S, et al. Association between maternal chronic conditions andcongenital heart defects: a population based cohort study. Circulation128(2013):583-589.
- Bernstein D. Epidemiology of congenital heart disease. In: Behr man RE, Kliegman RM, Jenson HB (eds) Nelson textbook of pediatrics.WB Saunders, Philadelphia 10(2000): 1362-1363
- Meberg A, Hals J, Thaulow E. Congenital heart defects chromo somal anomalies, syndromes and extracardiac malformations. ActaPaediatr 96(2007):1142-1145.
- Buskens E, Stewart PA, Hess J, et al. Efficacy of fetal echocardiography and yield by risk category. ObstetGynecol 87(1996):423-428.
- Mahle WT, Clancy RR, McGaurn SP, et al. Impact ofprenatal diagnosis on survival and early neurologic morbidity in neonates with the hypoplastic left heart syndrome. Pediatrics 107(2001):1277-1282.
- Swanson TM, Selamet Tierney ES, Tworetzky W, et al.Truncusarteriosus: diagnostic accuracy, outcomes, and impactof prenatal diagnosis. PediatrCardiol 30(3) (2009):256-261.
- Morris SA, Ethen MK, Penny DJ, et al. Prenatal diagnosis, birth location, surgical center, and neonatalmortality in infants with hypoplastic left heart syndrome. Circulation129(2014):285-292.
- Cohen MS, Schultz AH, Tian ZY,et al. Heterotaxy syndrome with functional single ventricle:does prenatal diagnosis improve survival? Ann ThoracSurg 82(2006):1629-1636.
- Srinivasan S, Strasburger J. Overview of fetal arrythmias. CurrOpinPediatr 20(5) (2008):522-531.
- Hofstaetter C, Hansmann M, EikNes SH, et al. A cardiovascular profile score in the surveillance of fetal hydrops. JMatern Fetal Neonatal Med 19(7) (2006):407-413.
- Makrydimas G, Sotiriadis A, Ioannidis JP. Screening performanceof first trimester nuchal translucency for major cardiac defects: a metaanalysis. Am J ObstetGynecol 189(5)(2003):1330-1335.
- Volpe P, Tuo G, De Robertis V, etal. interrupted aortic arch: 2D-4Dechocardiography, associations and outcome. Ultrasound ObstetGynecol 35(3) (2010):302-309.
- Allan LD. Echocardiographic detection of congenital heartdisease in the fetus: present and future. Br Heart 74(1995):103-106.
- Rychik J, Ayres N, Cuneo B, et al. American society of echocardiography guidelines and standardsfor performance of the fetal echocardiogram. J Am SocEchocardiogr7(7) (2004):803-810.
- Meyer Wittkopf M, Cooper S, Sholler G. Correlation betweenfetal cardiac diagnosis by obstetric and pediatric cardiologist sonographers and comparison with postnatal findings. Ultrasound ObstetGynecol 17(2001):392-397.
- Chaubal NG, Chaubal J. Fetal echocardiography. Indian J RadiolImaging 19(1)(2009):60-68
- Allan L, Benacerraf B, Copel JA, et al. Isolated major congenital heart disease. Ultrasound ObstetGynecol17(2001):370-379.
- Buskens E, Grobbee DE, Frohn Mulder IM, et al. Efficacy of routine fetal ultrasoundscreening for congenital heart disease in normal pregnancy. Circulation 94(1)(1996):67-72.
- Nayak K, Chandra GSN, Shetty R, et al. Evaluation of fetalechocardiography as a routine antenatal screening tool for detectionof congenital heart disease. CardiovascDiagnTher 6(1)(2016):44-49.
- Archiron R, Glaser J, Gelernter I, et al. Extended fetalechocardiographic examination for detecting cardiac malformations inlow risk pregnancies. BMJ 304(1992):671-674.
- Carvalho JS, Mavrides E, Shinebourne EA, et al.Improving the effectiveness of routine prenatal screening formajor congenital heart defects. Heart 88(2002):387-391.
- Chitra N, Vijayalakshmi IB. Fetal echocardiography for earlyetection of congenital heart diseases. J Echocardiogr 15(1)(2017):13-17.
- Jaeggi E, Sholler GF, Jones O, et al. Impact of fetal echocardiography on the course of major congenital heart disease: a population based study. J Am CollCardiol 31(1998): 71A
- Li M, Wang W, Yang X, et al. Evaluation of referralIndications for fetal echocardiography in Beijing. J Ultrasound Med27(2008):1291-1296.
- Vaidyanathan B, Kumar S, Sudhakar A, et al.Conotruncalanomalies in the fetus: referral patterns and pregnancy outcomes ina dedicated fetal cardiology unit in South India. Ann PediatrCardiol6(2013):15-20.
- Knowles RL, Ridout D, Crowe S, et al. Ethnic andsocioeconomic variation in incidence of congenital heart defects.Arch Dis Child 102(6) (2017):496-502.
- Zhang YF, Zeng XL, Zhao EF, et al. Diagnostic value of fetalechocardiography for congenital heart disease: a systematic reviewand meta analysis. Medicine (Baltimore) 94(2015):e1759.
- Soongswang J, Thitadilok W, Suansaneevithayaakul P, et al.Efficacy of fetal echocardiography and an evaluation of indication. J Med Assoc Thai 88(2005):S215-S220
- Buyens A, Gyselaers W, Coumans A, et al. Difficult prenatal diagnosis: fetal coarctation.Facts Views Vis ObstetGynaecol 4(4) (2012):230-236
- Wilson NJ, Allen BC, Clarkson PM, et al. One year audit of a referral fetal echocardiography service. NZMed J 107(1993):258-260
- Yagel S, Weissman A, Rotstein Z, et al. Congenital heart defects: natural course and in uterodevelopment. Circulation 96(1997):550-555.
- Simpson JM. Hypoplastic left heart syndrome. Ultrasound ObstetGynecol 15(2000):271-278.
- Strasburger JF, Cheulkar B, Wichman HJ. Perinatal arrythmias:diagnosis and management. ClinPerinatol 34(2007):627-652.
- Sklansky M, Tang A, Levy D, et al. Maternal psychological impact of fetal echocardiography. J AmSocEchocardiogr 15(2002):159-16638.
- Brown KL, Sullivan ID. Prenatal detection for major congenitalheart disease: a key process measure for congenital heart networks.Heart 100(05)(2014):359-360.
- Donofrio MT. Predicting the future: delivery room planning ofcongenital heart disease diagnosed by fetal echocardiography. 33(2018).
- Peyvandi S, Nguyen TA, Almeida Jones M, etal.Timing and mode of delivery prenatally diagnosed congenital heart disease: an analysis of practiceswithin the University of California Fetal Consortium (UCfC). PediatrCardiol 38(3) (2017):588-595.
- Holland BJ, Myers JA, Woods CR Jr, et al. Prenatal diagnosis of critical congenital heart disease reduces risk of death fromcardiovascularcompromise prior to planned neonatal cardiac surgery: a metaanalysis.Ultrasound ObstetGynecol 45(06)(2015):631-638.
