Clinical Profiles of Atrial Fibrillation Patients With or Without Cancer: Analysis from the Jordan Atrial Fibrillation Study
Article Information
Ismail Hamam1, Zaid Abdulelah2, Ibrahim Jarrad1, Alia Khamis2, Muyasar Amro3, Ayat Taqash4, Hadeel Abdelkhaleq4, Abdellbaset Al-Khatib1, and Ayman Hammoudeh5
1Department of Internal Medicine, King Hussein Cancer Center, Amman, Jordan
2Office of Scientific Affairs and Research, King Hussein Cancer Center, Amman, Jordan
3Nursing Department, King Hussein Cancer Center, Amman, Jordan
4Data management and biostatics unit, King Hussein Cancer Center, Amman, Jordan
5Department of Internal Medicine, Istishari Hospital, Amman, Jordan
*Corresponding Author: Ismail Hamam, King Hussein Cancer Center - Department of Internal Medicine, Queen Rania Al-Abdullah Street, P.O.Box 1269 Al-Jubaiha, Amman 11941 Jordan.
Received: 18 October 2023; Accepted: 25 October 2023; Published: 04 December 2023.
Citation: Ismail Hamam, Zaid Abdulelah, Ibrahim Jarrad, Alia Khamis, Muyasar Amro, Ayat Taqash, Hadeel Abdelkhaleq, Abdellbaset Al-Khatib, and Ayman Hammoudeh. Clinical Profiles of Atrial Fibrillation Patients With or Without Cancer: Analysis from The Jordan Atrial Fibrillation Study. Journal of Cancer Science and Clinical Therapeutics 7 (2023): 224-232.
View / Download Pdf Share at FacebookAbstract
Background: Atrial Fibrillation (AF) is the most prevalent arrhythmia and is associated with high morbidity and mortality. Cancer can predispose to AF directly or through adverse effects of specific anti-cancer agents.
Methods: A total of 2036 Consecutive adult patients with AF in 19 hospitals and 11 outpatient clinics in Jordan were enrolled in the Jordan AF study from May 2019 to October 2020 and followed prospectively for one year. Clinical and epidemiological characteristics of patients with cancer were compared to those without cancer. Results: Of the 2036 patients enrolled, 133 (6.5%) had cancer; with gastrointestinal cancers being the most common type (21%). Patients with cancer were older (70.6±10 vs. 67.8±1 P=0.041) tends to have fewer symptoms at presentation, have more permanent AF (42.6% vs. 29.4%, P=0.0005), and are more likely to have left ventricular hypertrophy (61.6% vs. 37.7%, p<0.001) and pulmonary hypertension (20.2% vs. 9.0%, p=0.002). These patients were more likely to be prescribed LMWH (21.3% vs. 1.5%, p<0.0001). And less likely to receive DOACs (40.7% vs. 59.1%, p< 0.001), cardio-protective and anti-arrhythmic agents compared to those without cancer. After one year of follow up all-cause mortality and major bleeding were significantly higher in the cancer group (32.8% vs. 13.3% p<0.0001) (6.3% vs. 2.4% P=0.022) respectively.
Conclusion: Middle Eastern patients with AF and cancer were older and had more permanent AF than patients without cancer. They were more likely to be prescribed LMWH, and less likely to receive DOACs and cardio-protective agents. They have significantly higher all-cause mortality and major bleeding at one-year follow-up.
Keywords
<p>Atrial Fibrillation, Cancer, Cardio-oncology.</p>
Atrial Fibrillation articles Atrial Fibrillation Research articles Atrial Fibrillation review articles Atrial Fibrillation PubMed articles Atrial Fibrillation PubMed Central articles Atrial Fibrillation 2023 articles Atrial Fibrillation 2024 articles Atrial Fibrillation Scopus articles Atrial Fibrillation impact factor journals Atrial Fibrillation Scopus journals Atrial Fibrillation PubMed journals Atrial Fibrillation medical journals Atrial Fibrillation free journals Atrial Fibrillation best journals Atrial Fibrillation top journals Atrial Fibrillation free medical journals Atrial Fibrillation famous journals Atrial Fibrillation Google Scholar indexed journals Cancer immunotherapy articles Cancer immunotherapy Research articles Cancer immunotherapy review articles Cancer immunotherapy PubMed articles Cancer immunotherapy PubMed Central articles Cancer immunotherapy 2023 articles Cancer immunotherapy 2024 articles Cancer immunotherapy Scopus articles Cancer immunotherapy impact factor journals Cancer immunotherapy Scopus journals Cancer immunotherapy PubMed journals Cancer immunotherapy medical journals Cancer immunotherapy free journals Cancer immunotherapy best journals Cancer immunotherapy top journals Cancer immunotherapy free medical journals Cancer immunotherapy famous journals Cancer immunotherapy Google Scholar indexed journals Cardio-oncology articles Cardio-oncology Research articles Cardio-oncology review articles Cardio-oncology PubMed articles Cardio-oncology PubMed Central articles Cardio-oncology 2023 articles Cardio-oncology 2024 articles Cardio-oncology Scopus articles Cardio-oncology impact factor journals Cardio-oncology Scopus journals Cardio-oncology PubMed journals Cardio-oncology medical journals Cardio-oncology free journals Cardio-oncology best journals Cardio-oncology top journals Cardio-oncology free medical journals Cardio-oncology famous journals Cardio-oncology Google Scholar indexed journals Direct oral anticoagulant articles Direct oral anticoagulant Research articles Direct oral anticoagulant review articles Direct oral anticoagulant PubMed articles Direct oral anticoagulant PubMed Central articles Direct oral anticoagulant 2023 articles Direct oral anticoagulant 2024 articles Direct oral anticoagulant Scopus articles Direct oral anticoagulant impact factor journals Direct oral anticoagulant Scopus journals Direct oral anticoagulant PubMed journals Direct oral anticoagulant medical journals Direct oral anticoagulant free journals Direct oral anticoagulant best journals Direct oral anticoagulant top journals Direct oral anticoagulant free medical journals Direct oral anticoagulant famous journals Direct oral anticoagulant Google Scholar indexed journals Low molecular weight heparin articles Low molecular weight heparin Research articles Low molecular weight heparin review articles Low molecular weight heparin PubMed articles Low molecular weight heparin PubMed Central articles Low molecular weight heparin 2023 articles Low molecular weight heparin 2024 articles Low molecular weight heparin Scopus articles Low molecular weight heparin impact factor journals Low molecular weight heparin Scopus journals Low molecular weight heparin PubMed journals Low molecular weight heparin medical journals Low molecular weight heparin free journals Low molecular weight heparin best journals Low molecular weight heparin top journals Low molecular weight heparin free medical journals Low molecular weight heparin famous journals Low molecular weight heparin Google Scholar indexed journals Left ventricular hypertrophy articles Left ventricular hypertrophy Research articles Left ventricular hypertrophy review articles Left ventricular hypertrophy PubMed articles Left ventricular hypertrophy PubMed Central articles Left ventricular hypertrophy 2023 articles Left ventricular hypertrophy 2024 articles Left ventricular hypertrophy Scopus articles Left ventricular hypertrophy impact factor journals Left ventricular hypertrophy Scopus journals Left ventricular hypertrophy PubMed journals Left ventricular hypertrophy medical journals Left ventricular hypertrophy free journals Left ventricular hypertrophy best journals Left ventricular hypertrophy top journals Left ventricular hypertrophy free medical journals Left ventricular hypertrophy famous journals Left ventricular hypertrophy Google Scholar indexed journals Pulmonary hypertension articles Pulmonary hypertension Research articles Pulmonary hypertension review articles Pulmonary hypertension PubMed articles Pulmonary hypertension PubMed Central articles Pulmonary hypertension 2023 articles Pulmonary hypertension 2024 articles Pulmonary hypertension Scopus articles Pulmonary hypertension impact factor journals Pulmonary hypertension Scopus journals Pulmonary hypertension PubMed journals Pulmonary hypertension medical journals Pulmonary hypertension free journals Pulmonary hypertension best journals Pulmonary hypertension top journals Pulmonary hypertension free medical journals Pulmonary hypertension famous journals Pulmonary hypertension Google Scholar indexed journals anti-cancer agents articles anti-cancer agents Research articles anti-cancer agents review articles anti-cancer agents PubMed articles anti-cancer agents PubMed Central articles anti-cancer agents 2023 articles anti-cancer agents 2024 articles anti-cancer agents Scopus articles anti-cancer agents impact factor journals anti-cancer agents Scopus journals anti-cancer agents PubMed journals anti-cancer agents medical journals anti-cancer agents free journals anti-cancer agents best journals anti-cancer agents top journals anti-cancer agents free medical journals anti-cancer agents famous journals anti-cancer agents Google Scholar indexed journals epidemiological articles epidemiological Research articles epidemiological review articles epidemiological PubMed articles epidemiological PubMed Central articles epidemiological 2023 articles epidemiological 2024 articles epidemiological Scopus articles epidemiological impact factor journals epidemiological Scopus journals epidemiological PubMed journals epidemiological medical journals epidemiological free journals epidemiological best journals epidemiological top journals epidemiological free medical journals epidemiological famous journals epidemiological Google Scholar indexed journals cerebrovascular diseases articles cerebrovascular diseases Research articles cerebrovascular diseases review articles cerebrovascular diseases PubMed articles cerebrovascular diseases PubMed Central articles cerebrovascular diseases 2023 articles cerebrovascular diseases 2024 articles cerebrovascular diseases Scopus articles cerebrovascular diseases impact factor journals cerebrovascular diseases Scopus journals cerebrovascular diseases PubMed journals cerebrovascular diseases medical journals cerebrovascular diseases free journals cerebrovascular diseases best journals cerebrovascular diseases top journals cerebrovascular diseases free medical journals cerebrovascular diseases famous journals cerebrovascular diseases Google Scholar indexed journals
Article Details
Abbreviations:
AF: Atrial Fibrillation
DOACS: Direct oral anticoagulant
LMWH: Low molecular weight heparin
LVH: Left ventricular hypertrophy
PAH: Pulmonary hypertension (PAH)
1. Introduction
Atrial fibrillation (AF) is the most common clinically significant cardiac arrhythmia [1]. It occurs when a diffuse and chaotic pattern of electrical activity in the atria suppresses or replaces the normal sinus mechanism. It is characterized by the presence of rapid, irregular, fibrillatory waves that vary in size, shape, and timing. There is a significant association of AF with morbidity and mortality with AF being an independent risk factor for cardiac related mortality, overall mortality, and cerebrovascular diseases [2-4]. AF is also common in cancer patients with approximately 2-5% of cancer patients having AF at the time of diagnosis [5-7]. In addition, new-onset AF has a higher incidence in cancer patients compared to the general population [8]. The association between AF and cancer and the underlying mechanism is not fully understood and can be bidirectional [9]. Patients who have cancer are at increased risk of developing AF [10], with inflammation, chemotherapeutic agents and other cancer-related comorbidities are proposed to affect atrial remodeling, resulting in AF [11,12]. Furthermore, cancer patients with AF are considered as special subgroup with an increased risk of bleeding and thromboembolism [13, 14] that are very challenging to treat and the evidence-based management strategies targeting this group are not well-established yet. We aim in our study to investigate the differences in clinical pictures, characteristics, and outcomes between AF patients with confirmed diagnosis of malignant comorbidity and their AF counterparts without cancer.
2. Methods
2.1 Ethical conduct of research:
The study was approved by the Institutional Review Board of each of the participating hospitals and every patient was asked signed a written informed consent prior to their enrolment. Moreover, patients had the right to withdraw from the study at any time without having to provide an excuse for their decision in addition to being able to be informed about the study results. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
2.2 Study Protocol
The Jordan AF Study is a prospective, observational, multicentre registry that enrolled consecutive patients aged >18 years who were diagnosed to have AF in 18 hospitals and 30 out-patient cardiology clinics, including a comprehensive tertiary cancer centre, in Jordan from May 2019 to October 2020. Data were collected on a standardized clinical study form at the time of enrolment. Baseline data included clinical profiles, cardiovascular risk factors, laboratory data, electrocardiographic (EKG) and echocardiographic features. CHA2DS2-VASc score and HAS BLED scores were calculated for each patient. Utilization of pharmacotherapy including oral anticoagulant medications (OACs) was evaluated at time of enrolment in the study. Additionally, patients were followed up for 1-year duration on 1 month, 6 months and 12 months intervals since time of enrolment. Follow up data included major complications of AF such as haemorrhage, systematic embolization, cerebrovascular accidents, TIAs, acute coronary disease and death. Moreover, anticoagulation therapy data were collected on follow up. We divided the patients into two groups; a patient who was had a confirmed diagnosis of cancer at the time of enrolment versus those who were enrolled in the study while being cancer free at the time of enrolment. Diagnosis of AF was confirmed by one of the following: (1) 12-lead EKG, (2) rhythm strip, lasting >30 seconds, [3] one or more episodes of AF on the Halter monitor, or (4) a diagnosis by a treating cardiologist. The definitions of AF types, namely first attack of AF, paroxysmal AF, persistent AF, and permanent AF, were according to the American College of Cardiology/American Heart Association/Heart Rhythm Society 2019 update on guidelines for the Treatment of patients with AF [15]. CHA2DS2-VASc score and HAS BLED scores were calculated for each patient according to the 2014 AHA/ACC/HRS Guideline on management of AF [16].
2.3 Statistical Analysis
Statistical analysis was conducted using the SPSS software package (version 25.0, SPSS Inc. Chicago, Illinois). Continuous variables were represented by mean (Standard deviation [SD]) or median (Interquartile range [IQR]) where suitable while categorical variables were represented by N (%). Univar ate analyses were carried out through comparing continuous variables by student’s t-test for independent samples or Mann-Whitney U test. Categorical data were compared using Chi-Squared test (χ2). Variables which were significant on Univar ate analyses were included in a multiple logistic regression to assess the association of each variable with the presence of atrial fibrillation-specific symptoms. Statistical significance level below 0.05 was used for all the study tests. All tests assumptions were met unless indicated elsewhere.
4. Results
We included 2036 consecutive AF patients over 16 months’ period. Of these patients, 133 (6.5%) had a coexisting cancer at the time of enrolment, with gastrointestinal cancers being the most common type of cancer (21%) followed by breast cancer (19.5%) (Table1). Table (1) shows the baseline demographic, clinical, and echocardiography features of the whole cohort and the non-cancer and the cancer subgroups. Patients with cancer were significantly older than patients without cancer (70.6 ± 10 vs. 67.8± 1 P= 0.041) with no gender difference between the two groups. Cancer patients have less dyslipidaemia (32% vs. 46% P=0.003), less likely to have heart failure diagnosis (11.3% vs 24.6% P < 0.001). Patients with AF and cancer were more likely to have permanent AF at presentation compared to patients without cancer (42.6% vs. 29.4%, P=0.0005). Left ventricular hypertrophy (LVH) and pulmonary hypertension (PAH) were diagnosed more frequently on echocardiography in patients with cancer compared to those without cancer (61.6% vs. 37.7%, p < 0.001) and (43.6 vs. 24.4%, p < 0.001) respectively. In addition to this calculated left ventricular ejection fraction (LVEF) is significantly lower in AF with cancer than without cancer (51±10 vs. 53± 12 P=0.00024). While mean CHA2DS2-VASc in patients with cancer was similar to those without cancer (3.7 ± 1.7 vs. 3.6 ± 1.8 p=0.337), the cancer group had a higher proportion of patients with CHA2DS2-VASc score ≥ 2.0 compared to those without cancer (91.9% vs. 84.8%, p=0.023). On the contrary, patients without cancer had higher mean HAS-BLED score compared to patients with cancer (1.7±1.1 vs. 1.4±0.8 vs. P=0.035) and higher proportions of patients with HAS-BLED score ≥3 compared to patients with cancer (20.2% vs. 9.0%, p=0.002). Figure 1 shows the use of cardiovascular agents including anticoagulant in cancer and non-cancer groups. While patients with cancer had a lower rate of direct oral anticoagulants (DOACs) utilization compared to patients without cancer (40.7% vs. 59.1%, p < 0.001), they had a higher rate of Low molecular weight heparin (LMWH) utilization (21.3% vs. 1.5%, p<0.0001). There was no difference in the utilization of vitamin K antagonist between the two groups (38% vs. 39.3%. p=0.568). In addition to this, AF patients with cancer are less likely to be prescribed with aspirin, amiodarone, renin angiotensin system blockers; diuretics and statins (Figure 1). Patients with cancer were found to be less symptomatic compared to those without cancer; fatigue (6.0% vs. 23.7%, p<0.0001), dizziness (3.0% vs. 12.3%, p<0.0001) and shortness of breath (6.0% vs. 36.2%, p<0.0001) (Figure 2). Of 2036 consecutive patients enrolled in this study, a total of 1636 patients stayed alive after 1 year follow up. 121 (5.9%) patients lost follow ups at one point. Overall total number of patients who were reported dead at one year follow up was 279 (13.7%). All-cause mortality was significantly higher in the group of patients with cancer compared with patients without cancer 32.8% vs. 13.3% p<0.0001) (Table 2). In addition to this major bleeding occurred in 2.4% of patients without cancer compared with 6.3% of the cancer group P=0.022. Major significant events occurred more frequently in patients with cancer than patients without cancer at 1, 6, and 12 months follow ups. These events including death, death at home, cardiac arrest, huge CVA, septic and cardiogenic shocks, development of renal failure, and new diagnosis of cancer. Despite of this there was no statistical deference in the rate of cerebrovascular accidents, acute coronary syndrome, systemic embolization or performance of electrical cardio version (Table 2). Multivariate analysis was carried out using conditional logistic regression to study the effect of active cancer of the aforementioned variables. The following variables were statistically significant: left ventricular hypertrophy (p-value = 0.0115), pulmonary hypertension (p-value = 0.0122), treatment with low molecular weight heparin (p-value = 0.0001), death at one year (p-value = 0.0003). All these variables increased with cancer patients with history of receiving LMWH (OR = 12.009, 95% CI = 4.629 - 31.152) and death at one year (OR = 4.465, 95% CI = 2.004 - 9.95) having the higher odds (Table 3).
Table 1: Demographic and characteristics of patients with (n = 133) and without (n = 1903) a history of cancer at the time of enrolment.
|
Variable |
All AF patients |
No cancer |
Cancer |
P-value |
|
Total 2036 |
||||
|
Female Sex |
1099 (54%) |
1031(54%) |
68(51%) |
0.495 |
|
Age (years) mean ± SD |
67.8± 13 |
70.6 ± 10 |
0.041 |
|
|
Type of cancer |
133 (6.5%) |
GI 28 (21%) |
||
|
Breast 26 (19.5%) |
||||
|
Urology 18 (13.5%) |
||||
|
Lung 10 (7.5%) |
||||
|
Leukemia 7 (5.2%) |
||||
|
Hypertension |
1518 (75%) |
1421(75%) |
97(73%) |
0.656 |
|
Diabetes mellitus |
889 (44%) |
821(43%) |
68(51%) |
0.073 |
|
Current Smoker |
283 (14%) |
263(14%) |
20(15%) |
0.695 |
|
Dyslipidemia |
914 (44%) |
871(46%) |
43(32%) |
0.003 |
|
BMI grp 25-<30 |
676 (33%) |
637(36%) |
39(34%) |
0.844 |
|
<25 |
430 (21%) |
402(23%) |
28(24%) |
|
|
>=30 |
766 (38%) |
717(41%) |
49(42%) |
|
|
AF type permanent |
610(30.3%) |
552(29.4%) |
58(42.6%) |
0.0005 |
|
AF Type paroxysmal |
735 (36%) |
687(36%) |
48(36%) |
0.998 |
|
Non-Valvular AF |
1865 (92%) |
1745(92%) |
120(90%) |
0.54 |
|
Stroke History |
313 (15%) |
300(16%) |
13(10%) |
0.064 |
|
Systemic Embolization History |
29 |
28(1.5%) |
1(0.8%) |
1 |
|
Heart failure |
483 |
468(24.6%) |
15(11.3%) |
0 |
|
Coronary artery disease |
221 |
208(10.9%) |
13(9.8%) |
0.679 |
|
Sleep Apnea |
84 |
77(4.0%) |
7(5.3%) |
0.495 |
|
Left Ventricle Ejection Fraction |
53± 12 |
51±10 |
0.00024 |
|
|
Left Ventricular Hypertrophy |
725 |
648(37.7%) |
77(61.6%) |
0 |
|
Pulmonary Hypertension |
520 |
462(24.4%) |
58(43.6%) |
0 |
|
Chronic Kidney Disease |
182 |
174(9.1%) |
8(6.0%) |
0.221 |
|
Mean CHA2DS2-VASc score |
3.6±1.8 |
3.7±1.7 |
0.337 |
|
|
Mean HAS-BLED Score |
1.7±1.1 |
1.4±0.8 |
0.035 |
|
|
HAS-BLED Score ≥ 3.0 |
384(20.2%) |
12(9.0%) |
0.002 |
|
|
CHA2DS2-VASc score ≥ 2.0 |
84.80% |
91.9 % . |
0.023 |
|
Data are given as n (%, complete case analysis) and mean ± SD.BMI body mass index, AF atrial fibrillation
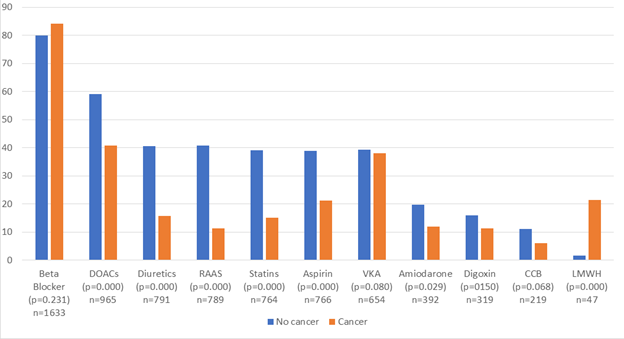
Figure 1: Cardiovascular medications in patients with atrial fibrillation and two subgroups of cancer and non-cancer patients
Data are given as (%), p value and total patients including cancer and non-cancer.
DOACs: direct oral anticoagulant agents, RAAS: renin angiotensin system blockers; VKA: vitamin K antagonists, CCB: Calcium channel blockers LMWH: low molecular weight heparin;
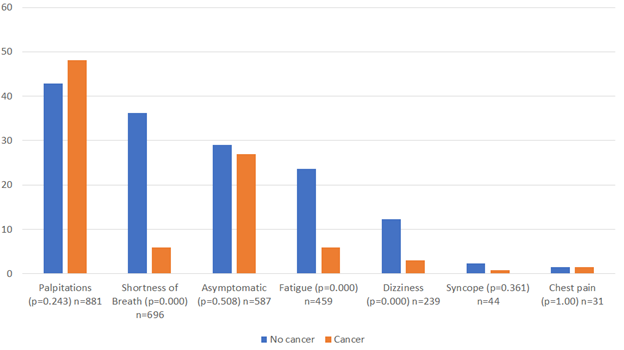
Figure 2: Atrial fibrillation related symptoms in the two subgroups of cancer and non-cancer patients
Data are given as (%), p value and total patients including cancer and non-cancer.
Table 2: One year outcomes in patients with atrial fibrillation and the two subgroups of cancer and non-cancer patients
|
Outcome |
Total |
No cancer |
Cancer |
P value |
|
Death (overall at one year) |
279 |
238(13.3%) |
41(32.8%) |
0 |
|
One month outcome (Death) |
89 |
77(4.0%) |
12(9.0%) |
0.007 |
|
6 month outcome (Death) |
122 |
104(5.5%) |
18 (13.5%) |
0 |
|
Electric cardioversion |
24 |
21(0.6%) |
3 (2.3%) |
0.062 |
|
CVA (overall at one year) |
67 |
63(3.9%) |
4(4.2%) |
0.786 |
|
Systemic Embolization Day(181-365) |
1 |
1 (0.1%) |
0% (0%) |
1 |
|
Major Bleeding |
45 |
39(2.4%) |
6(6.3%) |
0.022 |
|
Other Significant Event |
158 |
133(6.9%) |
25(18.8%) |
0.001 |
|
ACS |
37 |
34(2.1%) |
3(3.2%) |
0.453 |
CVA cerebrovascular accident, ACS: acute coronary syndrome.
Table 3: Multivariate analysis of the variables that are associated with active cancer
|
Effect |
Odds ratio |
95% Wald |
p-value |
|
|
Confidence Limits |
||||
|
dyslipidemia (Present vs. Absent) |
1.07 |
0.6 |
1.909 |
0.8176 |
|
AF Symptoms SOB (Yes vs. No) |
0.136 |
0.052 |
0.357 |
<.0001 |
|
AF Symptoms dizziness (Yes vs. No) |
0.254 |
0.068 |
0.94 |
0.0402 |
|
Comorbidity HF (Yes vs. No) |
0.26 |
0.106 |
0.637 |
0.0032 |
|
Left Ventricular Hypertrophy (Yes vs. No) |
1.987 |
1.167 |
3.383 |
0.0115 |
|
Pulmonary Hypertensio (Yes vs. No) |
2.031 |
1.167 |
3.535 |
0.0122 |
|
LMWH vs. DOACs |
12.009 |
4.629 |
31.152 |
<.0001 |
|
VKA vs. DOACs |
1.258 |
0.715 |
2.213 |
0.4255 |
|
Amiodarone (Yes vs. No) |
0.719 |
0.346 |
1.491 |
0.375 |
|
Aspirin (Yes vs. No) |
0.658 |
0.244 |
1.775 |
0.4083 |
|
Antiplatelet Agents (Yes vs. No) |
0.918 |
0.361 |
2.333 |
0.8572 |
|
RAAS inhibitor ACE (Yes vs. No) |
0.466 |
0.238 |
0.911 |
0.0255 |
|
Statin (Yes vs. No) |
0.566 |
0.28 |
1.144 |
0.1128 |
|
Diuretic (Yes vs. No) |
0.374 |
0.187 |
0.749 |
0.0055 |
|
HAS-BLED Score (more than or equal 3 vs. less than 3) |
0.161 |
0.056 |
0.458 |
0.0006 |
|
Status 1Year (Death vs. Alive) |
4.465 |
2.004 |
9.95 |
0.0003 |
LMWH: low molecular weight heparin; DOACs: direct oral anticoagulant agents, RAAS: renin angiotensin system blockers; VKA: vitamin K antagonists.
4. Discussion
Although association between AF and cancer has been extensively studied before [17], and it is well known that cancer patients have a higher risk of AF than general population [18] but data on direct comparison between AF patients who have and who have not cancer are lacking. Our main objective in this study was to compare AF patients in cancer and non-cancer patients using data from the Jordan AF study and to study the effect of cancer on AF patients included in this study. The comparison between 133 AF patients who have cancer and a cohort of 1903 AF patients with no history of cancer from the same general middle eastern population revealed that those with cancer, whether metastatic or not, were less likely to have comorbidities such as dyslipidemia, chronic kidney diseases, heart failure and less mean HAS-BLED score. However, they were older and more often to have history of permanent AF, PAH and lower mean LVEF than in non-cancer patients. In addition to this, there were no difference in the findings of DM, HTN, sleep apnea and many other classical risk factors for AF .This suggests that while these medical conditions might play a significant role in the development of AF in many patients, finding of AF in cancer patients can be related to cancer itself rather than to other classical medical risk factors. This finding is consistent with many previous studies that found AF to be common in cancer patients and new-onset AF has a higher incidence in cancer patients compared to the general population [5, 6, 7]. In our study we observed some differences and similarities when we compare cancer and non-cancer patients with AF. This can be explained by the facts that the factors contributing to the development, diagnosis, treatment, and complications of AF and cancer have complex interrelations, many of which are bidirectional. The development of AF and cancer are promoted by genetics, risk factors, systemic inflammation, and neurohormonal changes [19]. Management of AF patients with cancer is challenging because of an increased risk of stroke and major bleeding in these patients. Unfortunately, current clinical prediction tools, e.g., CHA2DS2-VASc and HAS-BLED score, do not consider cancer diagnosis and may not be suitable for patients with cancer. Nevertheless, in the absence of better tools, the CHA2DS2-VASc score is recommended. In our study we found that the cancer group had a higher proportion of patients with CHA2DS2-VASc score ≥ 2.0 compared to those without cancer, although mean CHA2DS2-VASc score was similar in both groups. In addition to this, patients without cancer had higher mean HAS-BLED score compared to patients with cancer. Despite of this, we found that after one year of prospective follow up, the major bleeding was significantly higher in cancer patients compared with non-cancer (table 2). This reflects the need to add other components to these scores like cancer itself to the current stroke and bleeding risk schemes as these score may underestimate bleeding and stroke risk in cancer patients. One of the main findings of our study was that AF patients with cancer are less likely to be prescribed with many cardio-protective agents such as aspirin, renin angiotensin system blockers, beta blocker; and statins (Figure 1), despite the fact that both groups shared the same baseline cardiovascular comorbidities such as smoking, DM, HTN and others. We noticed that patients with cancer are less likely to be prescribed anti arrhythmic agents like amiodarone as well. All of these raise the question about the suboptimal cardiovascular care in patients with cancer where focusing on providing complex anti-cancer treatment without establishing optimal cardiovascular care can increase the cardiovascular events in these patients [20]. We also found that cancer patients had a lower rate of DOACs utilization and higher rate of LMWH compared to patients without cancer. This finding reflects the complexity in managing cancer patients, where fear of bleeding, drug –drug interactions, prolonged half-life, lack of dedicated clinical trials, presence of anemia, thrombocytopenia and renal impairment favor LMWH over DOACs [21,22] We found that Patients with cancer tends to be less symptomatic compared to those without cancer (Figure 2), and this can be explained by the fact that patients with cancer frequently attend medical visits, so detection of asymptomatic AF is more likely in patients with cancer than in those without cancer and the fact that cancer patients have more permanent AF than non-cancer which is known to cause less symptoms than other types of AF [23]. Our data confirm that all-cause mortality, major bleeding and major significant events were significantly higher in the group of patients with cancer compared with patients without cancer at 1,6 and 12 months follow ups (Table 2). After extensive search in the literatures we found that this study is the first prospective study to show increased all-cause mortality when we compare AF patients without and with cancer. Systematic review and meta-analysis of 18 published studies by Murtaza et al suggested that cancer patients who subsequently develop AF have an increased rate of mortality as compared to those who do not [24]. Both cancer and AF are known separately to increase risk of death when compared to general population as both of them are a high-risk of life-threatening conditions. This can support our findings of increased mortality in our patients who have concomitant cancer and AF. This implies that extra care and specific measures must be taken in the management of cancer patients when it combines with AF.
Limitations:
Our study is subject to the same limitations as other prospective observational studies as they have potential bias of residual confounding, issues with validity, data collection, and patient recall of events. These limitations were overcome by the special care was taken in collecting and reviewing the data by the registry team at all participating centre across Jordan, in addition to efforts done by the registry organizers who worked on the completion of any missing or unclear data by contacting team members, patients and their families if needed directly. All participating study centres have collected data using same standardized clinical study form and were monitored directly by the registry organizing comity. Another limitation of this study is the relatively small size of patients with cancer (6.5%) compared to the number of patients without cancer which can affect the statistical analysis in general and out comes analysis in particular.
Conclusion
This is the first prospective, observational, multicentre study that enrolled consecutive patients who have AF in Jordan. We compared patients who had a confirmed diagnosis of cancer with those who had no cancer at the time of enrolment. We found that patients who have AF and coexisting cancer were older, tends to have less symptoms at presentation, and higher prevalence of permanent AF than patients without cancer. These patients were more likely to be prescribed LMWH and less likely to receive DOACs, cardio-protective and anti-arrhythmic agents compared to those without cancer. After one year of follow up we found that all-cause mortality, major bleeding and major significant events were significantly higher in patients with cancer compared with patients without cancer.
Acknowledgments
The authors would like to thank the participating physicians who enrolled patients for the study (in alphabetical order): Abdallah Al-Kasasbeh, Abdelrahman Obiedat, Abdullah Bani-Melhim, Abdul Nasser Almohamed, Ahmad Abdelsattar, Ahmad Abu Awwad, Ahmad Sbaih, Ahmad Tamari, Alaa Ababneh, Alanoud Hamada, Ali Abu-Romman, Ali Shakhatreh, Amer Asia, Amin Ibdah, Amr Adas, Assem Nammas, Aws Mukhtar, Ayad Al Qudsi, Basil Abdeen, Dalia Rawashdeh, Eid Abu- Eid, Eyadeh Madanat, Eyas Al Mousa, Fahd Al-Karmi, Farah Al-Sayyed, Farah Halaweh, Fatima Al Nadi, Hana Al- Raie, Haneen Shawer, Hani Juha, Hanin Saleh, Hanna Makhamreh, Hazem Abu Asbeh, Hesham Janabi, Hisham Amin, Ibrahim Abbadi, Imad A AlhaddadI ,slam Abu Sedo, Islam Obeidat, Kais Bilbeisi, Lama Khader, Leen Sharqawi, Liza Shaban, Lubaba Qabbaa, Lubna Haikal, Lubaba Qabbaah, Laith Habahbeh, Marwan Nemri, Marwan Al Sultan, Mo’ath Alfawar’a, Mohammad Abdah, Mohammad Afeef, Mohammad Al-Jawabreh, Mohammad Ali Jarrah, Mohammad Hani, Mohammad Kraishan, Mohannad Ababneh, Mohamad Jarrah, Mohammad Jabary, Munir Zaqqa, Mustafa Jammal, Nazih Kaderi, Noor Al-Badaineh, Obada Mansour, Odai Khasawneh, Oday Abu Ajameyyeh, Omar Abu Slieh, Omar Obeidat, Omar Salaymeh, Omran Abukhalaf, Osama Oudeh, Qusai Abu Ajameyyeh, Raed Awaisheh, Rami Bataineh, Ramzi Tabbalat, Rashid Abdah, Sa’ad Al-Muhaisen, Saed Al Ghamri, Safa’ Amro, Said Meri, Saleh Ghamdi, Sukaina Rawashdeh, Sara Al-Thunibat, Sara Younis, Sharif Adwan, Sulafa Saffarini, Tamer Salhab, Tawfiq Barqawi, Yahya Badaineh, Yahya Ismail, Yousef Khader, Zaid Dabash, Zeina Abu-Orabi, Zainab Salahat, Zainah Matani, and Zakariya Al-Hasanat.
Declarations:
Ethical Approval:
The study was approved by the Institutional Review Board of each of the participating hospitals. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Consent to participate:
Every patient was asked signed a written informed consent prior to their enrolment. Moreover, patients had the right to withdraw from the study at any time without having to provide an excuse for their decision in addition to being able to be informed about the study results.
Consent to publish:
All authors have read and approved the manuscript for publications.
Competing interests:
The authors declare that they have no competing interests.
Authors' contributions:
I.H. and A.H. participated in the conception and design of the manuscript. I.H., Z.A., and A. Kh worked on the paperwork and IRB submission. I.H, I. J, A. Kh, Z. A, A. Al, M. A, and A.H worked on patients’ enrolments and follow-ups.I.H, Z. A, A. Kh and A.H worked on the drafting of the manuscript and revising the manuscript critically for important intellectual content. A. T and H.A participated in the statistical analysis and interpretation of data. All authors read and approved the final manuscript. I.H participated in oversight and leadership responsibility for the research activity in addition to the manuscript submission process.
Funding:
All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Availability of data and materials:
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. This is subject to the institutional data sharing policy.
References
- Zimetbaum P. Atrial Fibrillation [published correction appears in Ann Intern Med 166 (2017 ): 33-48.
- Kannel WB, Benjamin EJ. Current perceptions of the epidemiology of atrial fibrillation. Cardiol Clin 27 (2009): 13.
- Wolf PA, Abbott RD and Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 22 (1991): 983-988.
- Benjamin EJ, Wolf PA, D'Agostino RB, et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 98 (1998): 946-952.
- Hu YF, Liu CJ, Chang PM et al. Incident thromboembolism and heart failure associated with new-onset atrial fibrillation in cancer patients. Int J Cardiol 165 (2013): 355-357.
- Patell R, Gutierrez A, Rybicki L, et al. Usefulness of CHADS2 and CHA2DS2-VASc Scores for Stroke Prediction in Patients With Cancer and Atrial Fibrillation. Am J Cardiol 120 (2017): 2182-2186.
- Sorigue M, Gual-Capllonch F, Garcia O, et al. Incidence, predictive factors, management, and survival impact of atrial fibrillation in non-Hodgkin lymphoma. Ann Hematol 97 (2018): 1633-1640.
- Conen D, Wong JA, Sandhu RK, et al. Risk of Malignant Cancer Among Women With New-Onset Atrial Fibrillation. JAMA Cardiology 1 (2016): 389-396.
- Rahman F, Ko D, Benjamin EJ. Association of Atrial Fibrillation and Cancer. JAMA Cardiol 1 (2016): 384-386.
- Hu YF, Liu CJ, Chang PM, et al. Incident thromboembolism and heart failure associated with new-onset atrial fibrillation in cancer patients. Int J Cardiol 165 (2013): 355-357.
- Velagapudi P, Turagam MK, Kocheril AG. Atrial fibrillation in cancer patients: an underrecognized condition. South Med J 104 (2011): 667-668.
- Mann DL, Krone RJ. Cardiac disease in cancer patients: an overview. Prog Cardiovasc Dis 53 (2010): 80-87.
- Mery B, Guichard JB, Guy JB, et al. Atrial fibrillation in cancer patients: Hindsight, insight and foresight. Int J Cardiol 240 (2017): 196-202.
- Farmakis D, Parissis J, Filippatos G. Insights into onco-cardiology: atrial fibrillation in cancer. J Am Coll Cardiol 63 (2014): 945-953.
- January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation 140 (2019): 125-151.
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American college of Cardiology/American heart association task force on practice guidelines and the heart rhythm society. J Am Coll Cardiol 64 (2014): 1-76.
- Mery B, Guichard JB, Guy JB, et al. Atrial fibrillation in cancer patients: Hindsight, insight and foresight. Int J Cardiol 240 (2017): 196-202.
- Vedovati MC, Giustozzi M, Verdecchia P, et al. Patients with cancer and atrial fibrillation treated with DOACS: a prospective cohort study. Int J Cardiol 269 (2018):152-157.
- Faisal Rahman, a Darae Ko, Emelia J, et alAssociation of atrial fibrillation and cancer, JAMA Cardiol 1(2016): 384-386.
- WY Cheung, R Levin, S Setoguchi. Appropriateness of cardiovascular care in elderly adult cancer survivors- Medical Oncology (2013).
- Dimitrios Farmakis, Pavlos Papakotoulas, Eleni Angelopoulou, et al. Anticoagulation for atrial fibrillation in active cancer .Oncol Lett 23 (2022): 124.
- Lee JY, Oh IY, Lee JH, et al. The increased risk of bleeding due to drug-drug interactions in patients administered direct oral anticoagulants. Thromb Res 195 (2020): 243-249.
- Flaker GC, Belew K, Beckman K, et al. Asymptomatic atrial fibrillation: demographic features and prognostic information from the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study. Am Heart J 149 (2005): 657-663.
- Minha Murtaza, Mirza Mehmood Ali Baig, Jawad Ahmed, et al. Higher Mortality Associated With New-Onset Atrial Fibrillation in Cancer Patients: A Systematic Review and Meta-Analysis. Cardiovasc. Med Sec. Cardio-Oncology 9 (2022).
