Clinical Profile of Patients of Acute Rheumatic Fever in a Specialized Center
Article Information
Md. Saidul Alam*, 1, Mohammad Abdul Hye2, Shuperna Ahmed3, Mohammad Aminul Islam4, Md. Arifur Rahman5, Shamsi Sumaiya Ashique6, Lohani Md Tajul Islam7, Mohammad Jobayer8
1Associate Professor, Department of Cardiology, National Center for Control of Rheumatic Fever & Heart Diseases, Dhaka, Bangladesh.
2Assistant Professor, Department of Pediatrics, Magura Medical College, Bangladesh.
3Associate Professor, Department of Pharmacology, Magura Medical College, Magura. Bangladesh.
4Assistant Professor, Department of Cardiology, National Center for Control of Rheumatic Fever & Heart Diseases, Dhaka, Bangladesh.
5Assistant Professor, Department of Cardiology, National Center for Control of Rheumatic Fever & Heart Diseases, Dhaka, Bangladesh.
6Assistant Professor, Department of Paediatrics, National Center for Control of Rheumatic Fever & Heart Diseases, Dhaka, Bangladesh.
7Medical Officer, Department of Cardiology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
8Assistant Professor, Department of Microbiology, National Center for Control of Rheumatic Fever & Heart Diseases, Dhaka, Bangladesh
*Corresponding author: Md. Saidul Alam, Associate Professor, Department of Cardiology, National Center for Control of Rheumatic Fever & Heart Diseases, Dhaka, Bangladesh
Received: 25 August 2023; Accepted: 02 September 2023; Published: 09 September 2023
Citation: Md. Saidul Alam, Mohammad Abdul Hye, Shuperna Ahmed, Mohammad Aminul Islam, Md. Arifur Rahman, Shamsi Sumaiya Ashique, Lohani Md Tajul Islam, Mohammad Jobayer. Clinical Profile of Patients of Acute Rheumatic Fever in a Specialized Center. Fortune Journal of Health Sciences. 6 (2023): 314 - 318.
View / Download Pdf Share at FacebookAbstract
Background: Acute rheumatic fever (ARF) is an important preventable health problem in developing countries. Early detection of clinical manifestations leads to better management of the disease. The study was designed to analyze the clinical characteristics of patients of ARF in a specialized center.
Methods: This cross-sectional study was conducted from January 2019 to March 2021 in National Center for Control of Rheumatic Fever and Heart Diseases, Dhaka, Bangladesh. A total of 185 clinically diagnosed patients of ARF, irrespective of age and sex were enrolled. Clinical profile of patients based on revised Jones criteria 2015 were recorded and analyzed.
Results: Fever was the commonest presenting complaint of patients with ARF followed by joint pain. The most common major criterion of ARF was carditis (78.4%) among which 25.4% was clinical carditis and 53% was subclinical carditis detected by Doppler echocardiography. Polyarthralgia was present in 56.7% patients whereas migratory polyarthritis and monoarthritis was found in 5.4% and 7.5% patients respectively. Two patients had Sydenham chorea and there was a solitary case of Erythema marginatum and no case of subcutaneous nodules was detected. Raised ASO titer (>200IU/ml) was found in 88.6% patients; 82.7% had high ESR, elevated CRP was found in 62.2% and fever (≥380C) was recorded in 50.3% patients.
Conclusions: Carditis was the most common major criterion with clinical carditis and subclinical carditis in about one-third and two-third of patients respectively. Polyarthralgia was the main joint manifestation. Echocardiography is essential to diagnose subclinical carditis in ARF patients.
Keywords
Acute rheumatic fever, arthritis, carditis, echocardiography
Article Details
1. Introduction
Acute Rheumatic fever (ARF) is a syndrome of autoimmune and non-suppurative inflammation that occurs as a sequel of pharyngeal infection by group A beta-haemolytic Streptococcu
s.[1] Usually the symptoms of ARF develop after two to three weeks of infection and can persist long after the infection has been cleared.[2] ARF involves heart, joints, skin, brain and subcutaneous cellular tissue.[3]
The major systemic inflammatory manifestations of ARF include carditis, arthritis, erythema marginatum, subcutaneous nodules and Sydenhams’ chorea.[2] Minor manifestations are less severe joint involvements, PR prolongation in ECG, fever, and several elevated inflammatory markers.[2] Carditis of ARF is pancarditis and valvulitis is the most common presentation.[4] It may range from mild sub-clinical involvement to severe carditis with congestive heart failure.[5] Arthritis of ARF has a predilection for large joints; it typically affects lower extremities first and ankles, knees, wrists and elbows are commonly affected.[6] Erythema marginatum is a transient skin manifestation the incidence of which is very low.[7] Subcutaneous nodules are of varying size with periarticular locations and overlying bony prominences.[8] These nodules are invariably associated with severe carditis.[9] Sydenhams’ chorea is a neurological condition characterized by involuntary movement and behavioral changes.[6] In view of an important public health issue especially in developing countries, it is important to emphasize early detection of the clinical manifestations of ARF which will consequently lead to better outcomes. The primary objective of the present study was to analyze the clinical characteristics of patients of ARF in a specialized center in Bangladesh.
2. Materials and Methods
This was a cross-sectional study and was conducted in the National Center for Control of Rheumatic Fever and Heart Diseases (NCCRF&HD), Bangladesh from January 2019 to April 2021.
Inclusion Criteria: A total of 185 clinically diagnosed patients of acute rheumatic fever were included in this study.
Exclusion Criteria: a) Patients with any history of acute illness (e.g., ischemic heart disease, renal or pancreatic diseases); and b) Patients with uncontrolled DM.
Study procedure: Patients of ARF irrespective of age and sex were included in this study. Patients were attended by specialist physicians and laboratory investigations (CBC with ESR, ASO titer, CRP), ECG were done and Doppler echocardiography was performed by cardiologists. Clinical features were classified as per the revised Jones Criteria 2015. Collaborating clinical history, physical examination, and investigation reports a clinical diagnosis of ARF was made.
Laboratory investigations: Quantitative ASO titer and semi-quantitative test of CRP was done in automated analyzer machine (ERBA Automated XL 200). ASO titer ≥200 International unit/ml and CRP ≥3.0 mg/dL were considered as significant.[2] ESR was performed in automated ESR machine (VES metric 20) and level ≥30 mm in first hour was considered an elevated level of ESR.[2] Doppler echocardiography was done with a modern echocardiography machine (Philips, Affinity, Taiwan).
Case definition
Acute rheumatic fever: Two major or one major and two minor Jones criteria and an evidence of recent streptococcal infection. Clinical carditis: Detection of pathological cardiac murmur on clinical examination by auscultation that was not previously present. Subclinical carditis: Pathological cardiac murmur detected on echocardiography that is not evident clinically on auscultation.
Statistical Analysis: All data were recorded systematically in preformed data collection form and quantitative data was expressed as mean and standard deviation and qualitative data was expressed as frequency distribution and percentage. Chi-square test was used for testing statistical significance. Statistical analysis was performed by using SPSS 21 (Statistical Package for Social Sciences). Probability value <0.05 was considered as level of significance.
Ethical Consideration: Ethical Review Committee of NCCRF&HD approved the study. Informed written consent was taken from each patient or authorized legal guardian. Participants were informed about the purpose of the study, the anonymity of the patients, and the confidentiality of information was maintained strictly.
3. Results
Table 1: Distribution of patients of acute rheumatic fever according to age and sex (n-185).
|
<5 yr |
5-7 yr |
8-10 yr |
11-13 yr |
14-16 yr |
17-19 yr |
≥ 20 yr |
Total |
|
|
n(%) |
n(%) |
n(%) |
n(%) |
n(%) |
n(%) |
n(%) |
n(%) |
|
|
Male |
1(0.5) |
10(5.4) |
29(15.7) |
21(11.3) |
9(4.9) |
8(4.3) |
3(1.6) |
81(43.8) |
|
Female |
2(1.1) |
15(8.1) |
37(20.0) |
30(16.2) |
12(6.5) |
6(3.2) |
2(1.1) |
104(56.2) |
|
Total |
3(1.6) |
25(13.5) |
66(35.7) |
51(27.6) |
21(11.3) |
14(7.6) |
5(2.7) |
185(100) |
Table 2: Major manifestations of acute rheumatic fever (following revised Jones criteria 2015)
|
Major manifestations |
Male n(%) |
Female n(%) |
Total n(%) |
P-value |
|
All carditis |
61(33.0) |
84(45.4) |
145(78.4) |
0.3707 |
|
Clinical carditis |
19(10.3) |
28(15.1) |
47(25.4) |
0.5911 |
|
Subclinical carditis |
42(22.7) |
56(30.3) |
98(53.0) |
0.7875 |
|
Polyarthritis |
4(2.2) |
6(3.2) |
10(5.4) |
0.8041 |
|
Monoarthritis |
6(3.2) |
8(4.3) |
14(7.5) |
0.942 |
|
Polyarthralgia |
45(24.3) |
60(32.4) |
105(56.7) |
0.771 |
|
Sydenham chorea |
0(0.0) |
2(1.1) |
2(1.1) |
- |
|
Erythema marginatum |
0(0.0) |
1(0.5) |
1(0.5) |
- |
|
Subcutaneous Nodules |
0(0.0) |
0(0.0) |
0(0.0) |
- |
Table 3: Minor manifestations and inflammatory markers in acute rheumatic fever
|
Minor manifestations |
Male n(%) |
Female n(%) |
Total n(%) |
P-value |
|
Monoarthralgia |
3(1.6) |
6(3.2) |
9(4.9) |
0.517 |
|
Fever (≥ 380C) |
42(22.7) |
51(27.6) |
93(50.3) |
0.7041 |
|
ESR ≥ 30mm in 1 hour |
68(36.8) |
85(45.9) |
153(82.7) |
0.4704 |
|
CRP ≥ 3.0 mg/dL |
47(25.4) |
68(36.8) |
115(62.2) |
0.3787 |
|
Prolonged PR interval |
2(1.1) |
1(0.5) |
3(1.6) |
0.4205 |
|
Inflammatory markers |
||||
|
Neutrophilia |
39(21.1) |
63(34.1) |
102(55.1) |
0.0917 |
|
ASO Titer (>200IU/ml) |
71(38.4) |
93(50.3) |
164(88.6) |
0.7067 |
ESR- erythrocyte sedimentation rate, CRP- c-reactive protein, ASO- anti-streptolysin O.
A total of 185 patients with clinically diagnosed acute rheumatic fever were enrolled in this study. Among them 63.3% patients were between the age of 8 to 13 years with maximum 35.7% diagnosed in 8-10 years age group followed by 11-13 years (27.6%). Female was predominant (56.2%) and female to male ratio was 1.28:1 in our study. [Table 1]
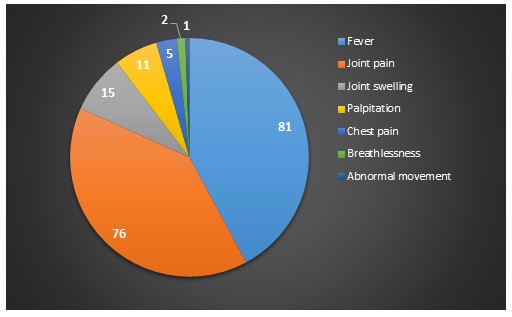
Fever and joint pain were the most common presenting features found in 81.1% and 76.2% of patients with ARF respectively, followed by joint swelling in 15.1% patients. [Figure 1]
The most common major criteria was carditis, present in 78.4% patients among which 53% were subclinical carditis and 25.4% were clinical carditis. Arthritis was found in 69.8% patients with polyarthralgia in 56.7% patients, migratory polyarthritis and monoarthritis was found in 5.4% and 7.5% cases respectively. There were two cases of Sydenham's chorea and a solitary case of Erythema marginatum was present. Differences between the occurrence of major manifestations among male and female patients were not statistically significant. [Table 2]
Monoarthralgia was found in 4.9% patients, fever with temperature ≥38°C was recorded in 50.3%, ESR ≥30mm in 1st hour was found in 82.7%, CRP ≥3mg/dL was found in 62.2% patients and prolonged PR interval in ECG was reported in 1.6% patients. Among the inflammatory markers, neutrophilia was present in 55.1% and raised ASO titer >200 IU per ml was found in 88.6% patients. Differences between rate of minor manifestations and inflammatory markers among male and female patients were not statistically significant. [Table-3].
4. Discussion
Acute rheumatic fever was common in females and among children of 5 to13 years of age and carditis was the most common major manifestation. Acute rheumatic fever is still an important public health burden in Bangladesh. ARF was more prevalent in female in this study and female to male ratio was 1.28:1. Thirty-five percent patients were diagnosed in 8-10 years of age followed by 11-13 years (27.6%). In majority of the patients with ARF in this study the presenting complaints was fever and joint pain which was consistent with finding of studies in Bangladesh and Malaysia where arthritis and fever were the most frequent presenting features of ARF cases.[10-12] The most common major criterion of ARF among this enrolled population was carditis and was detected in four-fifth (more than 78%) of the patients which was very much consistent with data of Bhardwaj et al in India.[13] Globally, carditis is the most common presentations of ARF and was detected in about half to as high as 92% patients in different studies.[10,13-16] Clinical carditis (with valvulitis murmur) and subclinical carditis (without murmur of valvulitis but with echocardiographic evidence of valvulitis) was present in about one-third and two-thirds patients respectively. Subclinical carditis (SCC) is relatively common and as a major Jones criterion it influenced the diagnosis of ARF in about 16% patients.[17] Use of Doppler echocardiography leads to detection of previously unrecognized cases of SCC and that increases the detection rate of ARF and rheumatic heart diseases several times than those diagnosed by auscultation alone.[18,19] This fact been established in this study where majority of patients would have been missed if echocardiography was not done.
Detection rate of SCC is higher in this study compared with other studies who reported the rate was 28-31%.[14,20] This data may indicate that SCC was much higher in this cohort of patients in this center and clinicians should be more careful during performing echocardiography not to miss the mild forms of carditis. Echocardiography was advised to be done by specialists to overcome the difficulties of detecting SCC and to minimize the possibility of overdiagnosis.[21] However, the consequences of underdiagnosis of ARF seem to be greater than over-diagnosis. Another explanation might suit the fact that NCCRF&HD is an outdoor-based center and patients with obvious manifestations of carditis usually seek treatment in hospitals with indoor facilities and support of admission. Every patient with suspected ARF should undergo echocardiography for evaluation of carditis, with those who remain negative in the first evaluation.[2] Echocardiography is more specific than auscultation and it excludes diagnosis of clinical carditis.[2,22] Recently, echocardiography (both conventional and portable) is being used increasingly, as a result, more and more cases of subclinical carditis are being diagnosed.[23] Joint manifestation of ARF was present in about seventy percent of patients among whom majority had polyarthralgia and migratory polyarthritis was present in only 5.4% patients. Arthritis of ARF is most classically a painful large joint migratory polyarthritis; it improves dramatically with anti-inflammatory therapy and a history of self-medication prior to presentation can mask its recognition. Migratory polyarthritis is often the first symptomatic sign of ARF. Though diagnosis of arthritis in ARF is challenging because of its non-specific presentation, and delayed onset.[6] NCCRF&HD, being a specialized center received a fair number of referred patients and due to its location in capital city, most of the patients came here after being treated or self-medicated with NSAIDs. Therefore, majority of them presented with arthralgia rather than arthritis and number of patients seeking treatment with arthritis or arthralgia was lower than normally should have been found if they came without medication.
In this study two children had isolated chorea; both of them were female and had delayed presentation (70 and 90 days). Sydenham chorea is characterized by abrupt and involuntary movements of trunk and/or extremities.[24] Chorea is often associated with emotional labiality and obsessive-compulsive disorder and can be used alone to confirm ARF.[25] The incidence of Erythema marginatum was very low and was seen only in one patient in this study. It is a rare manifestation of ARF and is seen in less than 10% of cases.[26] Low level of detection (0.4-3%) was reported in several studies.[13,17,20] Erythema marginatum is transient and may not be present at the time of examining the patient by physicians. Besides, this skin manifestation is more often missed due to darker skin complexion in Bangladeshi patients. Another major criterion, subcutaneous nodules was not present in any patient in our study. Erythema marginatum and subcutaneous nodules are rare manifestations of ARF. These were even absent in a few studies in this geographical region. [10,27,28] Some authors argued about reconsideration of these symptoms in major Jones criteria mentioning that they had no importance in the diagnosis of new cases. [27,29]
Limitations of the study
Our study was a single-center study. The sample size was not rich and our study period was short. After evaluating those patients, we did not follow them up for a long term and have not known about other possible interference that may happen in the long term with these patients.
Conclusion & Recommendations
Acute rheumatic fever was common in females and among 8 to 13 years of age patients. Fever was the commonest presenting complaint of patients followed by joint pain. Carditis was the most common major manifestation, two-thirds of which was subclinical. Therefore, echocardiography should be used to diagnose subclinical carditis in every suspected ARF patient. So, we recommend that further study with a prospective and longitudinal study design including a larger sample size needs to be done on rheumatic fever for early diagnosis and to reduce morbidity.
Funding of the work
The research did not receive any rant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgment
We, the authors thankfully acknowledge NCCRF&HD for providing data collection and the entire laboratory facilities.
Declaration of competing interest
The authors have no competing interests to declare
References
- Pathak H, Marshall T. Post-streptococcal reactive arthritis: where are we now. BMJ Case Rep (2016): bcr2016215552.
- Gewitz MH, Baltimore RS, Tani LY, et al. Revision of the Jones criteria for the diagnosis of acute rheumatic Fever in the era of Doppler echocardiography: a scientific statement from the American heart association. Circulation 131 (2015): 1806-18.
- Carapetis JR, Beaton A, Cunningham MW, et al. Acute rheumatic fever and rheumatic heart disease.Nat Rev Dis Primers 2 (2016): 15084.
- Edwards WD, Peterson K, Edwards JE. Active valvulitis associated with chronic rheumatic valvular disease and active myocarditis. Circulation 57 (1978): 181-5.
- Tubridy-Clark M, Carapetis JR. Subclinical carditis in rheumatic fever: a systematic review. Int J Cardiol 119 (2007): 54-8.
- Seckeler MD, Hoke TR. The worldwide epidemiology of acute rheumatic fever and rheumatic heart disease. Clin Epidemiol 3 (2011): 67-84.
- Achebe I, Hussain K, Abraham A, et al. Acute rheumatic fever presenting as a mimicker of septic arthritis. Cureus 12 (2020): e9431.
- Webb RH, Grant C, Harnden A. Acute rheumatic fever. BMJ 351 (2015): h3443.
- Kumar JD, James SS, Venkataraman P, et al. Subcutaneous nodules in acute rheumatic fever-a case report. Sri Ramachandra Journal of Medicine 4 (2011): 40-1.
- Saha SK, Choudhury KN, Sarker NR, et al. Non adherence to secondary prophylaxis for rheumatic fever. Int J ContempPediatr 7 (2020): 2101-5.
- Zaman MM, Choudhury SR, Rahman S, et al. Prevalence of rheumatic fever and rheumatic heart disease in Bangladeshi children. Indian Heart Journal 67 (2015): 45-9.
- Gururaj AK, Choo KE, Ariffin WA, et al. A clinical, laboratory and echocardiographic profile of children with acute rheumatic fever. Singapore Med J 31 (1990)): 364-7.
- Bhardwaj R, Sood A. Clinical profile of acute rheumatic fever patients in a tertiary care institute in present era. J Assoc Physicians India 63 (2015): 22-4.
- Caldas AM, Terreri MT, Moises VA, et al. What is the true frequency of carditis in acute rheumatic fever? A prospective clinical and Doppler blind study of 56 children with up to 60 months of follow-up evaluation. Pediatr Cardiol 29 (2008): 1048-53.
- Breda L, Marzetti V, Gaspari S, et al. Population-based study of incidence and clinical characteristics of rheumatic fever in Abruzzo, central Italy, 2000-2009. J Pediatr 160 (2012): 832-6.
- Rayamajhi A, Sharma D, Shakya U. Clinical, laboratory and echocardiographic profile of acute rheumatic fever in Nepali children. Ann Trop Paediatr 27 (2007): 169-77.
- Vijayalakshmi IB, Vishnuprabhu RO, Chitra N, et al. The efficacy of echocardiographic criterions for the diagnosis of carditis in acute rheumatic fever. Cardiol Young 18 (2008): 586-92.
- Marijon E, Ou P, Celermajer DS, et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med 357 (2007): 470-6.
- Saxena A, Ramakrishnan S, Roy A, et al. Prevalence and outcome of subclinical rheumatic heart disease in India: the RHEUMATIC (Rheumatic Heart Echo Utilisation and Monitoring Actuarial Trends in Indian Children) study. Heart 97 (2011): 2018-22.
- Paulo LT, Terreri MT, Barbosa CM, et al. Is rheumatic fever a more severe disease in pre-school children? ActaReumatol Port 34 (2009): 66-70.
- Jobayer M, Alam MS, Rana RA, et al. Rheumatic fever and rheumatic heart disease among clinically suspected patients with joint pain in a specialized hospital. Bangladesh Med Res Council Bull 48 (2022): 83-9.
- Roberts K, Maguire G, Brown A, et al. Rheumatic heart disease in Indigenous children in northern Australia: differences in prevalence and the challenges of screening. Med J Aust 203 (2015): 221.
- Islam AKMM, Majumder AAS. Rheumatic fever and rheumatic heart disease in Bangladesh: A review. Indian Heart Journal 68 (2016): 88-98.
- Kaminecki I, Verma R, Brunetto J, et al. Delayed diagnosis of acute rheumatic fever in a patient with multiple emergency department visits. Case Reports in Pediatrics (2018): 9467131.
- Punukollu M, Mushet N, Linney M, et al. Neuropsychiatric manifestations of Sydenham’s chorea: a systematic review. Developmental Medicine and Child Neurology 58 (2016): 16-28.
- Qurashi MA. The pattern of acute rheumatic fever in children: experience at the children’s hospital, Riyadh, Saudi Arabia. J Saudi Hear Assoc 21 (2009): 215-20.
- Rana M, Brijesh K. Validity of Jones criteria for diagnosis of rheumatic fever and rheumatic heart disease. Int J Adv Med 3 (2016): 250-3.
- Sarkar MK, Malviya K, Barpha AS, et al. Role of echocardiography in acute rheumatic fever compared with Jones Criteria. Int J Med Res Rev 3 (2015): 502-6.
- Okello E, Ndagire E, Muhamed B, et al. Incidence of acute rheumatic fever in northern and western Uganda: a prospective, population-based study. Lancet Glob Health 9 (2021): e1423-30.