Clinical Profile and Maternal–Neonatal Outcomes of Thrombocytopenia in Pregnancy: A Prospective Observational Study
Article Information
Vidhi Singh*,1, Priyanka kanwaria2, Ayushi Aggrawal3
1Assistant Professor – Department of Obstetrics and Gynecology, govt medical college Datia
2Senior Resident – Department of Obstetrics and Gynecology, govt medical college Datia
3Resident -– Department of Obstetrics and Gynecology, govt medical college Datia
*Corresponding Author: Vidhi Singh, Department of Obstetrics and Gynaecology, Govt Medical College Datia, India.
Received: 26 January 2025; Accepted: 29 January 2026; Published: 07 February 2026
Citation: Vidhi Singh, Priyanka kanwaria, Ayushi Aggrawal. Clinical Profile and Maternal–Neonatal Outcomes of Thrombocytopenia in Pregnancy: A Prospective Observational Study. Fortune Journal of Health Sciences. 9 (2026): 88-93.
View / Download Pdf Share at FacebookAbstract
Background: Thrombocytopenia is a common hematological abnormality encountered during pregnancy and may range from a benign physiological finding to a manifestation of severe maternal disease with significant fetomaternal implications.
Objectives: To evaluate the clinical profile, etiological spectrum, severity, and associated maternal and neonatal outcomes of thrombocytopenia in pregnancy. Methods: This prospective observational study was conducted over 24 months at a tertiary care center and included 350 pregnant women with platelet counts <150 × 109/L. Maternal demographics, severity and etiology of thrombocytopenia, and maternal and neonatal outcomes were analyzed.
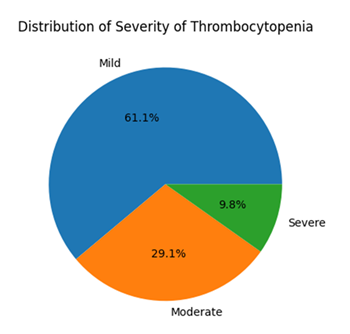
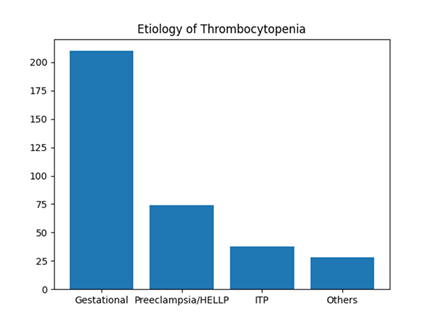
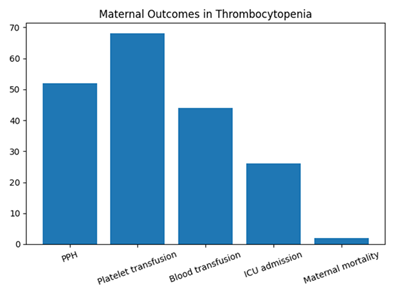
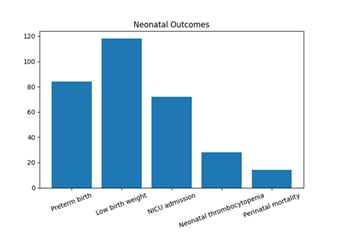
Results: Mild thrombocytopenia was observed in 61.1% of women, moderate in 29.1%, and severe in 9.8%. Gestational thrombocytopenia was the most common etiology (60%), followed by hypertensive disorders of pregnancy (21.1%) and immune thrombocytopenic purpura (10.9%). Postpartum hemorrhage occurred in 14.9% of cases, and 19.4% required platelet transfusion. Severe thrombocytopenia was significantly associated with increased rates of postpartum hemorrhage, intensive care unit admission, and transfusion (p < 0.001). Adverse neonatal outcomes included preterm birth (24%), low birth weight (33.7%), neonatal intensive care unit admission (20.6%), neonatal thrombocytopenia (8%), and perinatal mortality (4%).
Conclusion: Thrombocytopenia in pregnancy is a heterogeneous condition. While mild gestational thrombocytopenia is largely benign, moderate to severe thrombocytopenia—particularly when associated with hypertensive disorders or immune thrombocytopenic purpura—is associated with significant maternal and neonatal morbidity.
Keywords
Thrombocytopenia, Pregnancy, Gestational thrombocytopenia, HELLP syndrome, Immune thrombocytopenic purpura, Maternal outcomes, Neonatal outcomes
Thrombocytopenia articles, Pregnancy articles, Gestational thrombocytopenia articles, HELLP syndrome articles, Immune thrombocytopenic purpura articles, Maternal outcomes articles, Neonatal outcomes articles.
Article Details
Introduction
Thrombocytopenia, defined as a platelet count below 150,000/µL, is one of the most common hematological abnormalities encountered during pregnancy, second only to anemia. It affects approximately 7–10% of pregnancies, depending on the population studied and diagnostic thresholds used [1–3]. Although often incidental, thrombocytopenia in pregnancy can range from a benign physiological finding to a marker of severe maternal disease with significant fetomaternal implications. The most frequent cause of thrombocytopenia in pregnancy is gestational thrombocytopenia, accounting for nearly 60–70% of cases [3,4]. This condition is typically mild, detected in the late second or third trimester, and not associated with adverse maternal or neonatal outcomes. In contrast, pathological causes such as hypertensive disorders of pregnancy (including preeclampsia and HELLP syndrome) and immune thrombocytopenic purpura (ITP) are less common but clinically significant, often presenting with moderate to severe thrombocytopenia and increased risk of hemorrhagic complications [4–6].
Hypertensive disorders contribute substantially to pregnancy-associated thrombocytopenia, where declining platelet counts often reflect disease severity rather than isolated hematological dysfunction [6,7]. Similarly, ITP, though relatively uncommon, poses challenges in management due to potential maternal bleeding and the risk of neonatal thrombocytopenia secondary to transplacental transfer of antiplatelet antibodies [8,9]. Thrombocytopenia in pregnancy has been associated with adverse outcomes such as postpartum hemorrhage, increased transfusion requirements, preterm birth, low birth weight, and neonatal intensive care unit admission, particularly in cases of severe thrombocytopenia or underlying systemic disease [10–12]. Early identification of thrombocytopenia, accurate etiological classification, and timely multidisciplinary intervention are therefore essential to optimize maternal and neonatal outcomes. Despite its clinical relevance, there remains variability in reported prevalence, etiological distribution, and outcome associations across different populations, especially in low- and middle-income countries. This prospective observational study was undertaken to evaluate the clinical profile, severity, etiological spectrum, and maternal–neonatal outcomes of thrombocytopenia in pregnancy at a tertiary care center.
Study Objectives
Primary Objective
- • To evaluate maternal and neonatal outcomes in pregnancies complicated by thrombocytopenia.
Secondary Objectives
- To describe the clinical and etiological profile of thrombocytopenia in pregnancy.
- To assess the relationship between severity of thrombocytopenia and adverse maternal outcomes.
- To determine the incidence and predictors of neonatal thrombocytopenia.
To evaluate the association between thrombocytopenia and postpartum hemorrhage (PPH).
Methodology
Study Design
- • Prospective observational study
Study Setting
- • Single tertiary care center (Department of Obstetrics & Gynecology)
Study Duration
- • 24 months
Sample Size
- • 350 pregnant women
Study Population
Inclusion Criteria
- • Pregnant women at any gestational age
- • Platelet count <150 ×109/L
- • Singleton pregnancy
- • Willing to provide informed consent
Exclusion Criteria
- • Known haematological malignancies
- • Chronic liver disease or splenomegaly
- • Use of anticoagulants
Pre-existing bone marrow disorders
Results
A total of 350 pregnant women with thrombocytopenia were included in the study
Table 1: Baseline demographic and obstetric characteristics (n=350)
|
Variable |
n |
% |
|
Primigravida |
148 |
42.3 |
|
Multigravida |
202 |
57.7 |
|
Booked |
286 |
81.7 |
|
Unbooked |
64 |
18.3 |
The majority of women were in the 25–30-year age group, and multigravidae constituted 57.7% of the study population, while 42.3% were primigravidae. Most women were booked cases (81.7%), indicating adequate antenatal care. Thrombocytopenia was predominantly detected during the third trimester, reflecting routine antenatal surveillance and disease progression in later gestation (Table 1).
Table 2: Severity of thrombocytopenia
|
Severity |
Platelet count (/µL) |
n |
% |
|
Mild |
100,000–150,000 |
214 |
61.1 |
|
Moderate |
50,000–99,999 |
102 |
29.1 |
|
Severe |
<50,000 |
34 |
9.8 |
Based on platelet count at diagnosis, mild thrombocytopenia (100,000–150,000/µL) was the most common presentation, observed in 214 women (61.1%). Moderate thrombocytopenia (50,000–99,999/µL) was noted in 102 women (29.1%), while severe thrombocytopenia (<50,000/µL) was seen in 34 women (9.8%) (Table 2, Figure 1).
Table 3: Etiology of thrombocytopenia
|
Etiology |
n |
% |
|
Gestational |
210 |
60 |
|
Preeclampsia/HELLP |
74 |
21.1 |
|
ITP |
38 |
10.9 |
|
Others |
28 |
8 |
Gestational thrombocytopenia was the predominant etiology, accounting for 60.0% (n=210) of cases. Hypertensive disorders of pregnancy, including preeclampsia and HELLP syndrome, constituted 21.1% (n=74). Immune thrombocytopenic purpura (ITP) was identified in 10.9% (n=38), while other causes such as viral infections, sepsis, and acute fatty liver of pregnancy accounted for 8.0% (n=28) (Table 3, Figure 2).
Table 4: Maternal outcomes
|
Outcome |
n |
% |
|
PPH |
52 |
14.9 |
|
Platelet transfusion |
68 |
19.4 |
|
ICU admission |
26 |
7.4 |
|
Maternal mortality |
2 |
0.6 |
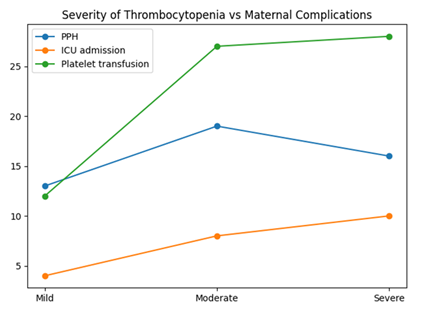
Maternal complications were observed more frequently with increasing severity of thrombocytopenia. Postpartum hemorrhage (PPH) occurred in 52 women (14.9%), and 19.4% (n=68) required platelet transfusion. ICU admission was necessary in 7.4% (n=26) cases. Maternal mortality was reported in 2 cases (0.6%), both associated with severe thrombocytopenia and underlying hypertensive disorders (Table 4, Figure 3).
Table 5: Neonatal outcomes
|
Outcome |
n |
% |
|
Preterm birth |
84 |
24 |
|
Low birth weight |
118 |
33.7 |
|
NICU admission |
72 |
20.6 |
|
Perinatal mortality |
14 |
4 |
Adverse neonatal outcomes were common. Preterm birth (<37 weeks) occurred in 24.0% (n=84) of neonates, while low birth weight (<2.5 kg) was observed in 33.7% (n=118). NICU admission was required for 20.6% (n=72) neonates. Neonatal thrombocytopenia was detected in 8.0% (n=28), and perinatal mortality was noted in 4.0% (n=14) cases (Table 5, Figure 4).
Table 6: Association between severity and maternal complications
|
Severity |
PPH % |
ICU % |
Transfusion % |
|
Mild |
6.1 |
1.9 |
5.6 |
|
Moderate |
18.6 |
7.8 |
26.5 |
|
Severe |
47.1 |
29.4 |
82.3 |
A significant association was observed between the severity of thrombocytopenia and maternal complications. The incidence of PPH increased from 6.1% in mild cases to 47.1% in severe thrombocytopenia. Similarly, ICU admission and platelet transfusion requirements rose markedly with severity, reaching 29.4% and 82.3%, respectively, in the severe group. This association was statistically significant (p < 0.001) (Table 6, Figure 5).
Discussion
Thrombocytopenia is a common hematological abnormality in pregnancy, with reported prevalence ranging from 7–10% in antenatal populations [1,2]. In the present prospective study of 350 women, mild thrombocytopenia constituted the majority (61.1%), followed by moderate (29.1%) and severe forms (9.8%). This distribution closely mirrors observations by Burrows and Kelton and Sainio et al., who reported that nearly two-thirds of thrombocytopenia in pregnancy is mild and clinically benign [1,3]. The predominance of third-trimester diagnosis in our cohort is consistent with the natural history of gestational thrombocytopenia, which is believed to result from hemodilution and increased platelet turnover in late pregnancy [4]. In our study, gestational thrombocytopenia accounted for 60% of cases, comparable to rates reported by McCrae (55–70%) and other Indian studies [4,5]. These findings reaffirm that gestational thrombocytopenia remains the most frequent and least morbid cause of low platelet counts during pregnancy.
Hypertensive disorders of pregnancy, including preeclampsia and HELLP syndrome, constituted 21.1% of cases in this study. Similar proportions have been reported by Sibai et al. and Goodnight et al., where thrombocytopenia served as a marker of disease severity rather than an isolated laboratory abnormality [6,7]. Importantly, these conditions were disproportionately represented among women with moderate and severe thrombocytopenia, highlighting their contribution to adverse outcomes. Immune thrombocytopenic purpura (ITP) accounted for 10.9% of cases, aligning with previously reported rates of 5–15% in tertiary-care settings [8,9]. Although ITP is relatively uncommon, its association with severe thrombocytopenia necessitates close maternal and neonatal monitoring due to the risk of hemorrhage and neonatal thrombocytopenia.
Maternal outcomes in the present study demonstrated a clear association between thrombocytopenia severity and complications. The overall incidence of postpartum hemorrhage (14.9%) is comparable to rates reported by Charoenkwan et al. and Bussel et al., particularly in women with platelet counts below 50,000/µL [10,11]. Notably, PPH occurred in nearly half (47.1%) of women with severe thrombocytopenia, underscoring platelet count as a critical determinant of bleeding risk. The rising need for platelet transfusion (82.3%) and ICU admission (29.4%) in severe cases parallels findings from earlier observational studies [6,11]. Neonatal morbidity in this study was also substantial. The rates of preterm birth (24%), low birth weight (33.7%), and NICU admission (20.6%) are comparable to those reported in pregnancies complicated by hypertensive disorders and HELLP syndrome [6,7]. Although neonatal thrombocytopenia was observed in only 8%, this aligns with existing literature indicating that most neonates born to thrombocytopenic mothers have normal platelet counts, except in cases of ITP or severe maternal disease [8,12]. The observed perinatal mortality rate of 4% likely reflects the severity of underlying maternal conditions rather than thrombocytopenia alone. Overall, these findings reinforce that thrombocytopenia in pregnancy is a heterogeneous condition, and clinical outcomes depend largely on etiology and severity of platelet reduction. While mild thrombocytopenia is generally benign, moderate and severe thrombocytopenia—particularly when associated with hypertensive disorders or ITP—pose significant maternal and neonatal risks. Early detection, etiological evaluation, and multidisciplinary management remain essential for improving outcomes.
Conclusion
Thrombocytopenia in pregnancy is a common yet heterogeneous condition, with clinical significance determined primarily by etiology and severity of platelet reduction. In this prospective observational study of 350 women, mild thrombocytopenia—predominantly gestational in origin—was the most frequent and generally associated with favorable maternal and neonatal outcomes. However, moderate and severe thrombocytopenia, particularly when associated with hypertensive disorders of pregnancy and immune thrombocytopenic purpura, were linked to a significantly increased risk of maternal hemorrhage, transfusion requirement, intensive care admission, and adverse neonatal outcomes. The findings underscore that thrombocytopenia should not be viewed as a uniform laboratory abnormality, but rather as a clinical marker that warrants etiological evaluation and risk stratification. Increasing severity of thrombocytopenia was independently associated with poorer fetomaternal outcomes, emphasizing the importance of platelet count as a prognostic indicator.
Clinical Implications
- • Routine platelet count estimation during antenatal care, particularly in the third trimester, is essential for early detection of thrombocytopenia.
- • Mild gestational thrombocytopenia usually requires reassurance and observation without aggressive intervention.
- • Moderate to severe thrombocytopenia mandates close maternal and fetal surveillance, with prompt identification of underlying causes such as preeclampsia, HELLP syndrome, or ITP.
- • Multidisciplinary management involving obstetricians, anesthesiologists, hematologists, and neonatologists is crucial in optimizing outcomes in high-risk cases.
- • Delivery planning should be individualized, with preparedness for blood and platelet transfusion, especially in women with platelet counts below 50,000/µL.
Neonatal monitoring, particularly for thrombocytopenia and prematurity-related complications, should be an integral component of postnatal care.
References
- Burrows RF, Kelton JG. Thrombocytopenia at delivery: a prospective survey of 6715 deliveries. Am J Obstet Gynecol 162 (1990): 731–734.
- Boehlen F, Hohlfeld P, Extermann P, et al. Platelet count at term pregnancy: a reappraisal. Br J Obstet Gynaecol 107 (2000): 737–741.
- Sainio S, Kekomäki R, Riikonen S, et al. Maternal thrombocytopenia at term: a population-based study. Acta Obstet Gynecol Scand 79 (2000): 744–749.
- McCrae KR. Thrombocytopenia in pregnancy. Hematology Am Soc Hematol Educ Program (2010): 397–402.
- Nisha S, Amita D, Uma S. Thrombocytopenia in pregnancy: clinical profile and outcome. J Obstet Gynaecol India 62 (02012): 413–416.
- Sibai BM. Diagnosis, controversies, and management of the syndrome of hemolysis, elevated liver enzymes, and low platelet count. Obstet Gynecol 103 (2004): 981–991.
- Goodnight WH, Soper DE. HELLP syndrome. Clin Obstet Gynecol 42 (1999): 381–389.
- Provan D, Stasi R, Newland AC, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood 115 (2010): 168–186.
- Gernsheimer T. Immune thrombocytopenia in pregnancy. Hematol Oncol Clin North Am 25 (2011): 293–310.
- Charoenkwan K, Sirivatanapa P. Pregnancy outcomes in women with thrombocytopenia. J Obstet Gynaecol Res 40 (2014): 214–220.
- Bussel JB, Primiani A. Current best practice in the management of immune thrombocytopenia. Ther Adv Hematol 7 (2016): 353–368.
- Payne SD, Resnik R, Moore TR. Outcome of pregnancies complicated by idiopathic thrombocytopenic purpura. Am J Obstet Gynecol 176 (1997): 734–738.