Clinical Course of Amyloid A Amyloidosis Secondary to Rheumatoid Arthritis Treated with Anti-Rheumatic Drugs Including Biologic Agent: Case Series in Answer Cohort
Article Information
Toru Hirano1, Yuichi Maeda1, Kosuke Ebina2, Koji Nagai3, Yonsu Son4, Hideki Amuro4, Ryota Hara5, Motomu Hashimoto6, Astushi Kumanogoh1
1Department of Respiratory Medicine and Clinical Immunology, Graduate School of Medicine, Osaka University, Suita, Osaka, Japan
2Department of Orthopaedic Surgery, Graduate School of Medicine, Osaka University, Suita, Osaka, Japan
3Department of Internal Medicine (IV), Osaka Medical College, Takatsuki, Osaka, Japan
4First Department of Internal Medicine, Kansai Medical University, Hirakata, Osaka, Japan
5The Center for Rheumatic Diseases, Nara Medical University, Kashihara, Nara, Japan
6Department of the Control for Rheumatic diseases, Graduate School of Medicine, Kyoto University, Kyoto, Japan
*Corresponding Author: Dr. Toru Hirano, Department of Respiratory Medicine and Clinical Immunology, Graduate School of Medicine, Osaka University, Suita, Osaka, Japan
Received: 06 August 2019; Accepted: 30 August 2019; Published: 02 September 2019
Citation: Hirano T, Maeda Y, Ebina K, Nagai K, Son Y, Amuro H, Hara R, Hashimoto M, Kumanogoh A. Clinical Course of Amyloid A Amyloidosis Secondary to Rheumatoid Arthritis Treated with Anti-Rheumatic Drugs Including Biologic Agent: Case Series in Answer Cohort. Archives of Clinical and Medical Case Reports 3 (2019): 508-517..
View / Download Pdf Share at FacebookAbstract
Systemic amyloid A (AA) amyloidosis secondary to rheumatoid arthritis (RA) is a serious complication, often leading to end-stage renal disease (ESRD) or death. Intervention with biologic agent, which has brought a paradigm shift in the treatment of RA, may improve the prognosis of AA amyloidosis. Among RA patients in ANSWER Cohort in Japan, 11 patients with biopsy-proven AA amyloidosis were identified and retrospectively investigated. Median age at the diagnosis of AA amyloidosis was 64 years and median disease duration of RA was 16 years. ESRD occurred in 5 patients, and 3 of them died. Seven patients received the treatment with biologic agents. Poor prognosis such as ESRD or death was associated with advanced renal dysfunction, insufficient anti-inflammatory treatment and longer disease duration of RA, whereas good prognosis was associated with no renal involvement or mild renal dysfunction, and the use of biologic agents. This observation, along with presentations of all identified cases, suggests the importance of disease control during mild kidney damage using potent anti-inflammatory drug such as biologic agent to improve prognosis..
Amyloid A amyloidosis articles, Rheumatoid arthritis articles, Biologic agent articles, Prognosis articles
Amyloid articles Amyloid Research articles Amyloid review articles Amyloid PubMed articles Amyloid PubMed Central articles Amyloid 2023 articles Amyloid 2024 articles Amyloid Scopus articles Amyloid impact factor journals Amyloid Scopus journals Amyloid PubMed journals Amyloid medical journals Amyloid free journals Amyloid best journals Amyloid top journals Amyloid free medical journals Amyloid famous journals Amyloid Google Scholar indexed journals Amyloidosis articles Amyloidosis Research articles Amyloidosis review articles Amyloidosis PubMed articles Amyloidosis PubMed Central articles Amyloidosis 2023 articles Amyloidosis 2024 articles Amyloidosis Scopus articles Amyloidosis impact factor journals Amyloidosis Scopus journals Amyloidosis PubMed journals Amyloidosis medical journals Amyloidosis free journals Amyloidosis best journals Amyloidosis top journals Amyloidosis free medical journals Amyloidosis famous journals Amyloidosis Google Scholar indexed journals Rheumatoid Arthritis articles Rheumatoid Arthritis Research articles Rheumatoid Arthritis review articles Rheumatoid Arthritis PubMed articles Rheumatoid Arthritis PubMed Central articles Rheumatoid Arthritis 2023 articles Rheumatoid Arthritis 2024 articles Rheumatoid Arthritis Scopus articles Rheumatoid Arthritis impact factor journals Rheumatoid Arthritis Scopus journals Rheumatoid Arthritis PubMed journals Rheumatoid Arthritis medical journals Rheumatoid Arthritis free journals Rheumatoid Arthritis best journals Rheumatoid Arthritis top journals Rheumatoid Arthritis free medical journals Rheumatoid Arthritis famous journals Rheumatoid Arthritis Google Scholar indexed journals Anti-Rheumatic articles Anti-Rheumatic Research articles Anti-Rheumatic review articles Anti-Rheumatic PubMed articles Anti-Rheumatic PubMed Central articles Anti-Rheumatic 2023 articles Anti-Rheumatic 2024 articles Anti-Rheumatic Scopus articles Anti-Rheumatic impact factor journals Anti-Rheumatic Scopus journals Anti-Rheumatic PubMed journals Anti-Rheumatic medical journals Anti-Rheumatic free journals Anti-Rheumatic best journals Anti-Rheumatic top journals Anti-Rheumatic free medical journals Anti-Rheumatic famous journals Anti-Rheumatic Google Scholar indexed journals Drugs articles Drugs Research articles Drugs review articles Drugs PubMed articles Drugs PubMed Central articles Drugs 2023 articles Drugs 2024 articles Drugs Scopus articles Drugs impact factor journals Drugs Scopus journals Drugs PubMed journals Drugs medical journals Drugs free journals Drugs best journals Drugs top journals Drugs free medical journals Drugs famous journals Drugs Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Cohort articles Cohort Research articles Cohort review articles Cohort PubMed articles Cohort PubMed Central articles Cohort 2023 articles Cohort 2024 articles Cohort Scopus articles Cohort impact factor journals Cohort Scopus journals Cohort PubMed journals Cohort medical journals Cohort free journals Cohort best journals Cohort top journals Cohort free medical journals Cohort famous journals Cohort Google Scholar indexed journals ESRD articles ESRD Research articles ESRD review articles ESRD PubMed articles ESRD PubMed Central articles ESRD 2023 articles ESRD 2024 articles ESRD Scopus articles ESRD impact factor journals ESRD Scopus journals ESRD PubMed journals ESRD medical journals ESRD free journals ESRD best journals ESRD top journals ESRD free medical journals ESRD famous journals ESRD Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals anti-inflammatory treatment articles anti-inflammatory treatment Research articles anti-inflammatory treatment review articles anti-inflammatory treatment PubMed articles anti-inflammatory treatment PubMed Central articles anti-inflammatory treatment 2023 articles anti-inflammatory treatment 2024 articles anti-inflammatory treatment Scopus articles anti-inflammatory treatment impact factor journals anti-inflammatory treatment Scopus journals anti-inflammatory treatment PubMed journals anti-inflammatory treatment medical journals anti-inflammatory treatment free journals anti-inflammatory treatment best journals anti-inflammatory treatment top journals anti-inflammatory treatment free medical journals anti-inflammatory treatment famous journals anti-inflammatory treatment Google Scholar indexed journals
Article Details
1. Introduction
Systemic amyloid A (AA) amyloidosis is a serious complication of rheumatoid arthritis (RA). Deposition of AA fibrils in kidney, intestine, heart and/or other organs leads to dysfunction of the organs and indicates poor prognosis. It has been reported that median survival time after diagnosis of AA amyloidosis was 133 months and factors associated with end-stage renal disease (ESRD) or death were high concentration of serum amyloid A protein (SAA), older age, long duration of inflammatory diseases and the existence of renal dysfunction [1]. Emergence of biologic agent such as tumor necrosis factor a (TNF) inhibitor, anti-Interleukin-6 (IL6) receptor agent and cytotoxic T lymphocyte associated protein 4 (CTLA4)-Fc fusion agent, or Janus kinase inhibitor has brought a paradigm shift in the treatment strategy of RA [2]. These drugs suppress joints’ inflammation and their destruction and reduce systemic inflammation of the patient. It is not clearly understood whether administration of these treatments could improve long-term prognosis for several years in RA patients with AA amyloidosis. Here we describe the clinical courses of 11 cases among a multicenter cohort with or without treatment of biologic agent.
2. Patients and Methods
The ANSWER Cohort consists of RA patients who were treated at the 7 hospitals in Kansai region, western Japan. Patients were diagnosed as RA according to the 2010 American College of Rheumatology (ACR)/European League against Rheumatism (EULAR) criteria, or the 1987 ACR criteria for rheumatoid arthritis [3, 4]. This cohort is a collaboration among Osaka University Hospital, Kyoto University Hospital, Kobe University Hospital, Osaka Medical University Hospital, Nara Medical University Hospital, Kansai Medical University Hospital and Osaka Redcross Hospital. The protocol of this cohort is approved by the ethics committee in each institution. All patients agreed with the participation in this cohort study. The study was conducted in accordance with the Helsinki Declaration.
Patients who were diagnosed as AA amyloidosis by histological examination were identified during the maximum observation period of 12 years among the cohort population. Pathologist in each institution diagnosed as AA amyloidosis by standard procedures, e.g. Congo Red Staining. We retrospectively collected their clinical information such as characteristics of the patients, organs affected by AA amyloidosis, laboratory data, treatments and prognosis. The most important outcome to consider in this study was the incidence of ESRD or death. The occurrence of ESRD was defined as the administration of dialysis due to advanced renal failure.
3. Results
Eleven patients with biopsy-proven AA amyloidosis were identified. Among these patients, 3 patients were diagnosed by renal biopsy, 5 patients were by upper gastrointestinal endoscopy and 3 patients were by lower gastrointestinal endoscopy. Characteristics of the patients are presented in Table 1. Ten patients were female, and one patient was male. Median age at the diagnosis of AA amyloidosis was 64 years with median duration of 16 years from the onset of RA (range 1 - 28 years). Organ involvements were seen in intestine (8/11), heart (2/11) and kidney (7/11). Treatments and the prognosis are summarized in Table 2. Drugs such as methotrexate (5/11), tacrolimus (2/11), glucocorticoid (7/11), salazosulfapyridine (1/11) and any biologic agent (7/11) were used to treat the patients. Five patients led to ESRD (case 5, 6, 7, 8 and 11), and 3 patients died (case 6, 8 and 11). All 4 patients without renal involvement survive, whereas patients with renal involvement had poor life prognosis (Figure 1A, p = 0.13, unadjusted). Patients with the use of biologic agent had better life prognosis than those without the use of biologic agent (Figure 1B, p = 0.0085, unadjusted). These results were mostly the same in ESRD-free survival rate (Figure 1C and 1D, p = 0.067 and p = 0.072, unadjusted). As shown in Figure 1E, poor prognosis such as ESRD or death was associated with the elevated levels of serum creatinine (p = 0.010, unadjusted). Disease durations of RA in patients with poor prognosis were tended to be longer than those in patients with good prognosis (median 21 years versus 13 years, p = 0.31, unadjusted).
|
Case |
Age |
Sex |
Duration of RA |
Organs |
|
1 |
51 |
F |
12 years |
Intestine (L)* |
|
2 |
62 |
F |
1 years |
Intestine (U)* |
|
3 |
69 |
F |
9 years |
Intestine (U)* |
|
4 |
69 |
F |
22 years |
Kidney* |
|
5 |
59 |
F |
25 years |
Intestine (U)*, Kidney, Heart |
|
6 |
64 |
M |
23 years |
Intestine (U)*, Kidney, Heart |
|
7 |
64 |
F |
12 years |
Intestine (U)*, Kidney |
|
8 |
68 |
F |
16 years |
Kidney* |
|
9 |
59 |
F |
14 years |
Intestine (L)* |
|
10 |
63 |
F |
28 years |
Intestine (U) (L)*, Kidney |
|
11 |
64 |
F |
21 years |
Kidney* |
Intestine (U): upper-gastrointestinal tract, Intestine (L): lower gastrointestinal tract, * denotes diagnosis of AA amyloidosis by histological examination
Table 1: Patients’ characteristics at the diagnosis of AA amyloidosis.
|
Case |
Biologic agent |
Others |
Observation period |
Prognosis |
|
1 |
aIL6R, TNFi, CTLA4Fc |
MTX |
50 months |
Good |
|
2 |
TNFi, aIL6R |
MTX |
84 months |
Good |
|
3 |
TNFi, aIL6R, CTLA4Fc |
MTX |
106 months |
Good |
|
4 |
aIL6R, CTLA4Fc |
TAC, GC |
20 months |
Good |
|
5 |
TNFi |
GC |
37 months |
ESRD |
|
6 |
None |
GC |
3 months |
ESRD, Death |
|
7 |
None |
TAC, GC |
113 months |
ESRD |
|
8 |
None |
MTX, GC |
24 months |
ESRD, Death |
|
9 |
aIL6R, TNFi |
MTX |
29 months |
Good |
|
10 |
TNFi, aIL6R |
GC |
108 months |
Good |
|
11 |
None |
SASP, GC |
17 months |
ESRD, Death |
GC: glucocorticoid, TNFi: Tumor Necrosis Factor inhibitor, aIL6R: anti-Interleukin-6 receptor agent, CTLA4Fc: cytotoxic T lymphocyte associated protein 4-Fc fusion agent, MTX: methotrexate, TAC: tacrolimus, SASP: salazosulfapyridine, GC: glucocorticoid, ESRD: end-stage renal disease.
Table 2: Treatments and Prognosis.
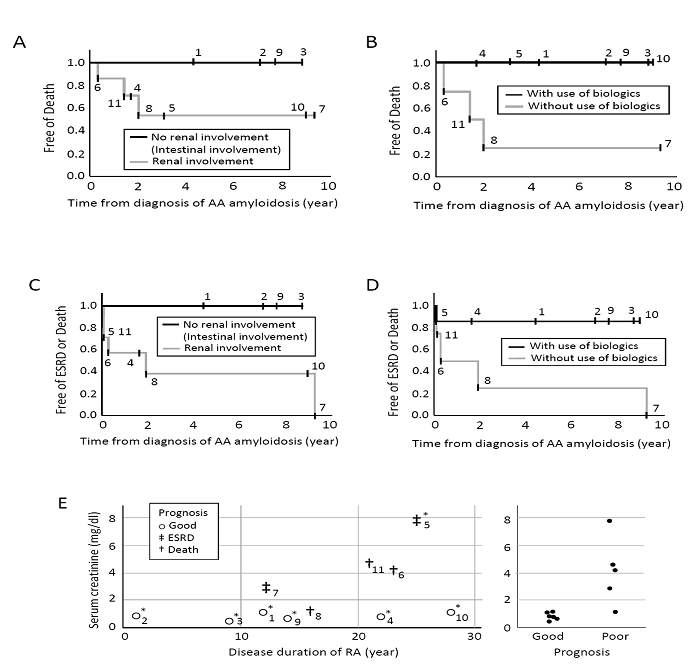
Figure 1: Prognosis of AA amyloidosis secondary to RA. A: Survival rate. Black line represents patients without renal involvement of AA amyloidosis, and gray line represents patients with renal involvement. B: Black line represents patients treated with the use of any biologic agent, and gray line represents patients treated without the use of biologic agent. C: ESRD-free Survival rate. Black line represents patients without renal involvement of AA amyloidosis, and gray line represents patients with renal involvement. D: Black line represents patients treated with the use of any biologic agent, and gray line represents patients treated without the use of biologic agent. E: Association between disease duration of RA, serum creatinine level at the diagnosis of AA amyloidosis and prognosis. Number identifies each case. * denotes cases with the use of biologic agent. ESRD: end-stage renal disease, RA: rheumatoid arthritis.
4. Case Presentation
Case 1 was a 50-year-old woman suffering severe diarrhea, appetite loss and weight loss. She needed total parenteral nutrition. Histological examination revealed deposition of AA fibrils in colon. Blood test showed hypoalbuminemia (1.6 g/dl) and elevated C-reactive protein (CRP, 72 mg/L). Treatments with etanercept and then infliximab, TNF inhibitors, combined with methotrexate did not ameliorate her symptoms. Tocilizumab, anti-IL6 receptor (IL6R) agent was started. After 3 months, her intestinal symptoms and deposition of AA fibrils completely disappeared. However, as joint symptoms persisted, adalimumab, TNF inhibitor, and later abatacept, CTLA4-Fc agent, was started. After 1 year, her intestinal symptom worsened again, and deposition of AA fibrils was proved again. Tocilizumab was re-administered, and her intestinal symptoms improved promptly. The deposition of AA fibrils disappeared again. The clinical course during the first administration of tocilizumab was reported previously [5].
Case 2 was a 62-year-old woman diagnosed as AA amyloidosis by upper gastrointestinal endoscopy. She was diagnosed as RA at the previous year. Her manifestations were diarrhea, edema, hypoalbuminemia (1.7 g/dl) and elevated CRP (89 mg/L). Infliximab combined with methotrexate was administered, however joint inflammation and gastrointestinal manifestation persisted. Tocilizumab was started. Gradually, her condition improved. She maintained low disease activity of RA and showed no gastrointestinal symptom.
Case 3 was a 64-year-old woman diagnosed as AA amyloidosis by upper gastrointestinal endoscopy. Her symptoms were arthralgia and edema. Laboratory examination revealed elevated CRP (37 mg/L), anemia (hemoglobin, 10.2 g/dl), hypoalbuminemia (2.1 g/dl) and elevated brain natriuretic peptide (BNP, 767 pg/ml). No clinical signs of heart failure except BNP elevation were observed. Infliximab combined with methotrexate was administered, however inflammation of joints persisted. The biological agents were serially changed to adalimumab, tocilizumab, abatacept, etanercept, golimumab and finally certolizumab pegol. The reason of changing these agents was insufficient responses to joint inflammation. Then, she continued to receive certolizumab pegol. The level of serum CRP and albumin normalized. Serum BNP level also improved to 126 pg/ml. No finding of heart failure was observed during the entire period.
Case 4 was a 69-year-old woman diagnosed as AA amyloidosis by renal biopsy. Her symptoms were arthralgia and edema. Laboratory test showed urinary protein excretion (2+, 0.4 g/gcreatinine), elevated CRP (9.2 mg/L), hypoalbuminemia (2.2 g/dl) and normal serum creatinine level (0.9 mg/dl). She was treated with tocilizumab, and later abatacept, combined with low-dose glucocorticoid and tacrolimus. The reason tocilizumab was changed to abatacept was insufficiency to joint inflammation. Her disease activity of RA remained low. The level of serum CRP normalized, and the urinary protein excretion disappeared. Serum level of creatinine increased slightly (1.35 mg/dl).
Case 5 was a 59-year-old woman suffering edema, diarrhea and appetite loss. She was diagnosed as AA amyloidosis by upper gastrointestinal endoscopy. Blood examination showed advanced renal dysfunction (serum creatinine 7.8 mg/dl) and elevated CRP (67 mg/L) and BNP (678 pg/ml). She needed hemodialysis. Advanced renal failure, heart failure and gastrointestinal insufficiency were considered due to AA amyloidosis. She was treated with adalimumab. Three years later, she continued to receive hemodialysis. The level of CRP declined to 16 mg/L, and the level of serum creatinine remained high (5.9 mg/dl). Symptoms such as edema and pleural effusion persisted due to heart failure. She was transferred to a different hospital and the course after that was not traced.
Case 6 was a 64-year-old man suffering edema, pleural effusion, severe diarrhea and appetite loss. The level of serum creatinine was 4.1 mg/dl, and the urinary protein excretion was massive (4+, 2.4 g/gcreatinine). Serum level of BNP was highly elevated (1180 pg/ml). Renal failure, heart failure and gastrointestinal insufficiency were considered due to AA amyloidosis. He was treated with moderate dose of glucocorticoid (prednisolone 20 mg/day), however serum creatinine level continued to increase and the heart failure did not improve. His general condition worsened, and three months after the diagnosis of AA amyloidosis, he died.
Case 7 was a 64-year-old woman diagnosed as AA amyloidosis by upper gastrointestinal endoscopy. Her symptoms were edema, diarrhea and appetite loss. The level of serum creatinine was 3.0 mg/dl. Renal failure and gastrointestinal symptoms were considered due to AA amyloidosis. High dose glucocorticoid (prednisolone 50mg/day) and tacrolimus were administered. Her joint and gastrointestinal manifestations improved. However, serum creatinine level reached to 7.1 mg/dl, and she needed hemodialysis.
Case 8 was a 68-year-old woman diagnosed as AA amyloidosis by renal biopsy. She received methotrexate and entecavir due to positivity of hepatitis B virus (HBV). The level of serum creatinine was 1.2 mg/dl. Treatment of tocilizumab was considered, however she did not accept the administration, because she was concerned about HBV reactivation and hepatitis. Serum CRP level remained high (around 20 mg/L). After 2 year, the level of serum creatinine reached to 7.2 mg/dl, and hemodialysis was administered. Three month later, she died unexpectedly at the other hospital. The detailed cause of death was unknown.
Case 9 was a 59-year old woman diagnosed as AA amyloidosis by lower gastrointestinal endoscopy. She was suffering severe diarrhea and abdominal pain. Serum examination showed elevate CRP (45 mg/L) and hypoalbuminemia (2.0 g/dl). Tocilizumab combined with methotrexate was started. At the second infusion of tocilizumab, severe infusion reaction occurred, and tocilizumab was discontinued. Adalimumab was started. Her joint and gastrointestinal manifestations disappeared. Serum levels of CRP and albumin normalized. Adalimumab combined with methotrexate was well tolerated.
Case 10 was a 63-year old woman diagnosed as AA amyloidosis by upper gastrointestinal endoscopy. She had arthralgia and diarrhea. Laboratory examination showed urinary protein excretion (2+), slight elevation of serum creatinine (1.2 mg/dl) and elevation of serum CRP (20 mg/L). Etanercept was started. However, 2 years later, etanercept was discontinued due to insufficient response to joint symtoms. She was suffering severe diarrhea again. Tocilizumab was started. Joint and intestinal symptoms improved. Serum level of CRP normalized and serum level of creatinine slightly increased (2.0 mg/dl). Urinary protein excretion persisted (2.5 g/gcreatinine). Her general condition remained stable.
Case 11 was a 64-year-old woman diagnosed as AA amyloidosis by renal biopsy. The level of serum creatinine was 3.3 mg/dl. She was treated with salazosulfapyridine. Serum CRP remained positive. One year later, serum level of creatinine reached to 4.7 mg/dl, and she needed to receive hemodialysis. Laboratory test showed elevated CRP (46 mg/L) and urinary protein excretion (2+, 3.3 g/gcreatinine). Treatment with salazosulfapyridine was continued. Two years later, she was admitted to another hospital and died due to heart failure.
5. Discussion
In this cohort, 11 patients were identified as AA amyloidosis secondary to RA. All the patients were diagnosed by histological examination of gastrointestinal tract or kidney. Poor prognosis such as ESRD or death was associated with the existence of renal involvement, especially the elevation of serum creatinine at the diagnosis of AA amyloidosis. On the other hand, good prognosis was associated with the administration of biologic agent, and no renal involvement or mild renal dysfunction. Disease duration of RA was tended to be longer in patient with poor prognosis.
In the case 4 and 10, although they had renal dysfunction and their disease durations of RA were relatively long (22 and 28 years), their prognosis were not poor. Serum creatinine levels of these patients at the time of diagnosis of AA amyloidosis were 0.92 mg/dl and 1.2 mg/dl, and these two patients received treatments with biologic agent such as etanercept, abatacept or tocilizumab. Introduction of biologic agent might suppress the progression of kidney disease or even ameliorate the renal involvement of AA amyloidosis because of the earlier phase of kidney disease. All 4 patients without renal involvement, who had only intestinal involvement (case 1, 2, 3 and 9), had good clinical courses with the use of biologic agent. Three patients showed the elevated serum BNP (case 3, 5 and 6). Among them, 2 patients (case 5 and 6) had advanced renal dysfunction, and their heart failure did not improve. In the case 3, who did not manifest heart failure clinically and her disease duration of RA was relatively short, serum BNP level declined and normalized with the treatment.
Irreversibility of organ damage may be strong in kidney and lesser in intestine. One case report suggested that therapeutic effects of tocilizumab might vary among organs and administration of tocilizumab ameliorated intestinal and heart findings however did not ameliorate renal insufficiency [6]. In our current study, differences of the efficacy among various biologic agents or by mode of action could not be assessed due to the small number of patients and the variation of patients’ background. There are some reports that administration of tocilizumab, anti-IL6R agent, promptly ameliorated organ damage induced by AA deposition [7-9]. There are also some reports that TNF inhibitor such as infliximab and etanercept ameliorated findings of AA amyloidosis [10-12]. One non-randomized controlled study suggested that tocilizumab may be superior to TNF inhibitor to suppress SAA production and ameliorate organ damage by AA deposition [13]. Abatacept, CTLA4-Fc agent, was reported to be effective in two RA patients with AA amyloidosis [14]. In the case 4, administration of abatacept switched from tocilizumab ameliorated the manifestations of RA and AA amyloidosis. Rituximab, anti-CD20 agent, was also reported to be effective in some patients [15].
This case series study is retrospective, observational and descriptive research. Patients’ background such as age, disease duration, affected organs, comorbidities and concomitant drugs differed widely between the patients. The number of the patients was too small to prove the clinical hypothesis statistically and to compensate confounders by multivariable analysis. Decisive conclusions need further verification by controlled study or observational study with more patients and longer period. However, we consider that the results of this study would contain important viewpoints for the management of AA amyloidosis secondary to RA or other inflammatory diseases.
6. Conclusion
In conclusion, our report suggests that poor prognosis of AA amyloidosis secondary to RA was associated with advanced renal dysfunction, insufficient anti-inflammatory treatment and longer duration of RA. By therapeutic intervention within the early stage of renal dysfunction, and by the use of potent anti-inflammatory drugs such as biologic agent, poor prognosis such as ESRD or death will be avoided.
Funding
None
Acknowledgement
We thank to Kengo Akashi, Akira Onishi, Masaaki Katayama, Keiichi Yamamoto, Shuzo Yoshida and Wataru Yamamoto for discussion on research protocol and interpretation of the results.
Conflict of Interest
The authors declare no conflicts of interest.
References
- Lachmann HJ, Goodman HJ, Gilbertson JA, et al. Natural history and outcome in systemic AA amyloidosis. N Engl J Med 356 (2007): 2361-2371.
- Smolen JS, Landewé R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis 76 (2017): 960-977.
- Aletaha D, Neogi T, Silman AJ, et al. Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62 (2010): 2569-2581.
- Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31 (1988): 315-324.
- Nishida S, Hagihara K, Shima Y, et al. Rapid improvement of AA amyloidosis with humanised anti-interleukin 6 receptor antibody treatment. Ann Rheum Dis 68 (2009): 1235-1236.
- Matsui M, Okayama S, Tsushima H, et al. Therapeutic Benefits of Tocilizumab Vary in Different Organs of a Patient with AA Amyloidosis. Case Rep Nephrol 2014 (2014): 823093.
- Sato H, Sakai T, Sugaya T, et al. Tocilizumab dramatically ameliorated life-threatening diarrhea due to secondary amyloidosis associated with rheumatoid arthritis Clin Rheumatol 28 (2009): 1113-1116.
- Inoue D, Arima H, Kawanami C, et al. Excellent therapeutic effect of tocilizumab on intestinal amyloid a deposition secondary to active rheumatoid arthritis. Clin Rheumatol 29 (2010): 1195-1197.
- Courties A, Grateau G, Philippe P, et al. Club Rhumatismes Inflammation and the REGATE Registry. AA amyloidosis treated with tocilizumab: case series and updated literature review. Amyloid 22 (2015): 84-92.
- Kuroda T, Otaki Y, Sato H, et al. A case of AA amyloidosis associated with rheumatoid arthritis effectively treated with Infliximab. Rheumatol Int 28 (2008): 1155-1159.
- Nakamura T, Higashi S, Tomoda K, et al. Efficacy of etanercept in patients with AA amyloidosis secondary to rheumatoid arthritis. Clin Exp Rheumatol 25 (2007): 518-522.
- Gottenberg JE, Merle-Vincent F, Bentaberry F, et al. Anti-tumor necrosis factor alpha therapy in fifteen patients with AA amyloidosis secondary to inflammatory arthritides: a followup report of tolerability and efficacy. Arthritis Rheum 48 (2003): 2019-2024.
- Okuda Y, Ohnishi M, Matoba K, et al. Comparison of the clinical utility of tocilizumab and anti-TNF therapy in AA amyloidosis complicating rheumatic diseases. Mod Rheumatol 24 (2014): 137-143.
- Nakamura T, Kumon Y, Hirata S, et al. Abatacept may be effective and safe in patients with amyloid A amyloidosis secondary to rheumatoid arthritis. Clin Exp Rheumatol 32 (2014): 501-508.
- Kilic L, Erden A, Sener YZ, et al. Rituximab Therapy in Renal Amyloidosis Secondary to Rheumatoid Arthritis. Biomolecules 8 (2018): 136.
