Chest Expander Spring a Low Cost Home Physiotherapy-Based Exercise Rehabilitation after Total Hip Arthroplasty
Article Information
Bahaa Kornah1, Saied K.Abdel-hameed2, Abdel-hamid A. Atallah3, Mohamed Ibrahem Abuelesoud4, Tharwat Abdel ghany5, Mohamed Abdelaziz6, Mohamed Abdel-AAl7,*, Nagi Saleem8
1Professor orthopedic surgery, Faculty of medicine for boys, Al-Azhar University, Cairo, Egypt
2Assistant professor of orthopedic surgery, Faculty of medicine for girls, Al-Azhar University, Cairo, Egypt
3Assistant Professor orthopedic surgery, Faculty of medicine for girls, Al-Azhar University,Cairo, Egypt
4Lecturer of orthopedic surgery, Faculty of medicine for boys, Al-Azhar University. Cairo, Egypt
5Assistant professor of orthopedic surgery, Faculty of medicine for boys, Al-Azhar University. Cairo, Egypt
6Lecturer of orthopedic surgery, Faculty of medicine for boys, Al-Azhar University. Cairo, Egypt
7Consultant orthopedic surgery – El bakey General Hospital, Ministry of Health, Cairo, Egypt
8Lecturer orthopedic surgery, Faculty of medicine for girls, Al-Azhar University. Cairo, Egypt
*Corresponding Author: Mohamed A. Abdel-AAl, Department of Orthopedics, El bakey General Hospital,
Ministry of Health, Cairo Egypt/p>
Received: 12 February 2020; Accepted: 25 Februaey 2020; Published: 29 August 2020
Citation: Bahaa Kornah, Saied K.Abdel-hameed, Abdel-hamid A. Atallah, Mohamed Ibrahem Abuelesoud, Tharwat Abdel ghany, Mohamed Abdelaziz, Mohamed Abdel-AAl, Nagi Saleem. Chest Expander Spring A Low Cost Home Physiotherapy-Based Exercise Rehabilitation after Total Hip Arthroplasty. Journal of Orthopaedics and Sports Medicine 2 (2020): 157-167.
View / Download Pdf Share at FacebookAbstract
Background: The demand for total hip arthroplasty (THA) is rising. Postoperative exercise rehabilitation helps patients recover normal joint functions by strengthening the muscles surrounding the replaced hip joint. In the face of rapidly increasing health care costs, ensuring widespread, cost-effective rehabilitation is a priority. However, the high cost of professionally supervised exercise rehabilitation programs limits access to program participation and, thus, to optimal recover of normal joint functions. Therefore, the development of an effective home-based, self-monitored exercise rehabilitation program is critical to promote the optimal recovery of THR patients.
Purpose: The aim of this study was to assess the feasibility, evaluate the effectiveness of a specific Progressive Resistance Exercise program for improving hip muscles strength, resorting hip joint mobility and address the functional needs of the patient treated with primary total hip arthroplasty. Additionally; spreading the idea of a low-cost post-operative rehabilitation program using chest expander spring.
Study Design: Prospective case series study.
Patients and Methods: This was a prospective single-center clinical study with a 12-week intervention program carried out in an outpatient clinic and in home based. 120 patients (84 males) had been enrolled in this study to which primary total hip arthroplasty had been done. Patients were evaluated preoperatively, at baseline, 2 weeks postoperative, one week following last visit of follow-up and at 6 months postoperatively. Clinical outcome measures involved: Harris Hip Score (HHS), Oxford Hip Score (OHS), WOMAC activity score, range of hip movements (ROM), Timed Get Up and GO Test and 6 Minutes walking test.
Results: The study included 120 patients (84 males). The mean age 65.3 years (range = 53-76 year
Keywords
Total hip arthroplasty; Home-based rehabilitation; Physiotherapy protocol; Chest expander; Hip functional outcomes
Orthopedic surgery articles Orthopedic surgery Research articles Orthopedic surgery review articles Orthopedic surgery PubMed articles Orthopedic surgery PubMed Central articles Orthopedic surgery 2023 articles Orthopedic surgery 2024 articles Orthopedic surgery Scopus articles Orthopedic surgery impact factor journals Orthopedic surgery Scopus journals Orthopedic surgery PubMed journals Orthopedic surgery medical journals Orthopedic surgery free journals Orthopedic surgery best journals Orthopedic surgery top journals Orthopedic surgery free medical journals Orthopedic surgery famous journals Orthopedic surgery Google Scholar indexed journals Total hip arthroplasty articles Total hip arthroplasty Research articles Total hip arthroplasty review articles Total hip arthroplasty PubMed articles Total hip arthroplasty PubMed Central articles Total hip arthroplasty 2023 articles Total hip arthroplasty 2024 articles Total hip arthroplasty Scopus articles Total hip arthroplasty impact factor journals Total hip arthroplasty Scopus journals Total hip arthroplasty PubMed journals Total hip arthroplasty medical journals Total hip arthroplasty free journals Total hip arthroplasty best journals Total hip arthroplasty top journals Total hip arthroplasty free medical journals Total hip arthroplasty famous journals Total hip arthroplasty Google Scholar indexed journals Arthritis articles Arthritis Research articles Arthritis review articles Arthritis PubMed articles Arthritis PubMed Central articles Arthritis 2023 articles Arthritis 2024 articles Arthritis Scopus articles Arthritis impact factor journals Arthritis Scopus journals Arthritis PubMed journals Arthritis medical journals Arthritis free journals Arthritis best journals Arthritis top journals Arthritis free medical journals Arthritis famous journals Arthritis Google Scholar indexed journals Joint articles Joint Research articles Joint review articles Joint PubMed articles Joint PubMed Central articles Joint 2023 articles Joint 2024 articles Joint Scopus articles Joint impact factor journals Joint Scopus journals Joint PubMed journals Joint medical journals Joint free journals Joint best journals Joint top journals Joint free medical journals Joint famous journals Joint Google Scholar indexed journals Muscle atrophy articles Muscle atrophy Research articles Muscle atrophy review articles Muscle atrophy PubMed articles Muscle atrophy PubMed Central articles Muscle atrophy 2023 articles Muscle atrophy 2024 articles Muscle atrophy Scopus articles Muscle atrophy impact factor journals Muscle atrophy Scopus journals Muscle atrophy PubMed journals Muscle atrophy medical journals Muscle atrophy free journals Muscle atrophy best journals Muscle atrophy top journals Muscle atrophy free medical journals Muscle atrophy famous journals Muscle atrophy Google Scholar indexed journals Quadriceps muscles articles Quadriceps muscles Research articles Quadriceps muscles review articles Quadriceps muscles PubMed articles Quadriceps muscles PubMed Central articles Quadriceps muscles 2023 articles Quadriceps muscles 2024 articles Quadriceps muscles Scopus articles Quadriceps muscles impact factor journals Quadriceps muscles Scopus journals Quadriceps muscles PubMed journals Quadriceps muscles medical journals Quadriceps muscles free journals Quadriceps muscles best journals Quadriceps muscles top journals Quadriceps muscles free medical journals Quadriceps muscles famous journals Quadriceps muscles Google Scholar indexed journals Physiotherapy articles Physiotherapy Research articles Physiotherapy review articles Physiotherapy PubMed articles Physiotherapy PubMed Central articles Physiotherapy 2023 articles Physiotherapy 2024 articles Physiotherapy Scopus articles Physiotherapy impact factor journals Physiotherapy Scopus journals Physiotherapy PubMed journals Physiotherapy medical journals Physiotherapy free journals Physiotherapy best journals Physiotherapy top journals Physiotherapy free medical journals Physiotherapy famous journals Physiotherapy Google Scholar indexed journals Rehabilitation articles Rehabilitation Research articles Rehabilitation review articles Rehabilitation PubMed articles Rehabilitation PubMed Central articles Rehabilitation 2023 articles Rehabilitation 2024 articles Rehabilitation Scopus articles Rehabilitation impact factor journals Rehabilitation Scopus journals Rehabilitation PubMed journals Rehabilitation medical journals Rehabilitation free journals Rehabilitation best journals Rehabilitation top journals Rehabilitation free medical journals Rehabilitation famous journals Rehabilitation Google Scholar indexed journals Hip articles Hip Research articles Hip review articles Hip PubMed articles Hip PubMed Central articles Hip 2023 articles Hip 2024 articles Hip Scopus articles Hip impact factor journals Hip Scopus journals Hip PubMed journals Hip medical journals Hip free journals Hip best journals Hip top journals Hip free medical journals Hip famous journals Hip Google Scholar indexed journals Arthroplasty articles Arthroplasty Research articles Arthroplasty review articles Arthroplasty PubMed articles Arthroplasty PubMed Central articles Arthroplasty 2023 articles Arthroplasty 2024 articles Arthroplasty Scopus articles Arthroplasty impact factor journals Arthroplasty Scopus journals Arthroplasty PubMed journals Arthroplasty medical journals Arthroplasty free journals Arthroplasty best journals Arthroplasty top journals Arthroplasty free medical journals Arthroplasty famous journals Arthroplasty Google Scholar indexed journals Chest articles Chest Research articles Chest review articles Chest PubMed articles Chest PubMed Central articles Chest 2023 articles Chest 2024 articles Chest Scopus articles Chest impact factor journals Chest Scopus journals Chest PubMed journals Chest medical journals Chest free journals Chest best journals Chest top journals Chest free medical journals Chest famous journals Chest Google Scholar indexed journals Fitness articles Fitness Research articles Fitness review articles Fitness PubMed articles Fitness PubMed Central articles Fitness 2023 articles Fitness 2024 articles Fitness Scopus articles Fitness impact factor journals Fitness Scopus journals Fitness PubMed journals Fitness medical journals Fitness free journals Fitness best journals Fitness top journals Fitness free medical journals Fitness famous journals Fitness Google Scholar indexed journals Osteoarthritis articles Osteoarthritis Research articles Osteoarthritis review articles Osteoarthritis PubMed articles Osteoarthritis PubMed Central articles Osteoarthritis 2023 articles Osteoarthritis 2024 articles Osteoarthritis Scopus articles Osteoarthritis impact factor journals Osteoarthritis Scopus journals Osteoarthritis PubMed journals Osteoarthritis medical journals Osteoarthritis free journals Osteoarthritis best journals Osteoarthritis top journals Osteoarthritis free medical journals Osteoarthritis famous journals Osteoarthritis Google Scholar indexed journals Fracture articles Fracture Research articles Fracture review articles Fracture PubMed articles Fracture PubMed Central articles Fracture 2023 articles Fracture 2024 articles Fracture Scopus articles Fracture impact factor journals Fracture Scopus journals Fracture PubMed journals Fracture medical journals Fracture free journals Fracture best journals Fracture top journals Fracture free medical journals Fracture famous journals Fracture Google Scholar indexed journals Exercises articles Exercises Research articles Exercises review articles Exercises PubMed articles Exercises PubMed Central articles Exercises 2023 articles Exercises 2024 articles Exercises Scopus articles Exercises impact factor journals Exercises Scopus journals Exercises PubMed journals Exercises medical journals Exercises free journals Exercises best journals Exercises top journals Exercises free medical journals Exercises famous journals Exercises Google Scholar indexed journals
Article Details
1. Introduction
Total hip Arthroplasty (THA) is considered as one of the most common elective, cost-effective and successful operations for relieving hip pain and improving physical functions caused by arthritis [1]. Also, a dramatic annual increase in the number of joint replacements over the last few decades throughout the world [2]. Owing to persistence of the underlying pre-operative pathology, patients may present with muscle atrophy and loss of strength, particularly in the glutei and quadriceps muscles. Consequently the elderly patients are less independent [3]. It makes sense that surgical intervention will correct the joint problems( either mechanical or anatomical) but associated muscle power impairment and functional limitations that was present before surgery, will remain (even up to a year following surgery) and require post-operative rehabilitation. Traditionally, physiotherapy has been a routine component of patient rehabilitation following hip replacement surgery [4]. So it is valid to consider how effective post-discharge Rehabilitation protocols after total hip replacement vary widely in both the specific exercises used and the timeframes for their delivery [4, 5].
Research has shown hip abductor weakness after surgery is a major risk associated with joint instability and prosthetic loosening [6]. So; post-operative rehabilitation program is mandatory to restore hip joint mobility, gain muscle strength and flexibility and share in reducing pain. In low income countries with unavailability of good rehabilitation centers there is an increased demand for a low cost rehabilitation protocol, easy to do, cost effective and easy to understand to the patient and relatives without highly occupied palace for rehabilitation to achieve satisfactory outcome after hip Arthroplasty.
2. Patient and Method
Chest Expander Spring is simple exercise equipment consisting of a pair of handles connected by springs (either 4 or 5 springs) that provide resistance (Figure 1).
Figure 1:
Traditionally, it targets the chest muscles but it can also be used to exercise the legs and back muscles as well. In this study the expander used to restore the hip muscles strength through Resistive hip muscle exercise as self-dependent patient rehabilitation. The 4 muscles group of the hip (Flexors, Extensors, Abductors and Adductors group of muscles) are trained and strengthened by adding one spring each time the muscles trained. Many strengthening exercises can be accomplished with the patient standing, sitting on a chair or lying on an exercise mat, allowing the patient to make the workout as strenuous or as relaxing as he/she needs. One end (hand gripper) is fixed to the ground while the other end is free to be prepared to adapt the foot of the patient. It is used as an outdoor or indoor Exercise Fitness Strength and Training Adjustable Resistance tool. The program is so simple as Exercise can be done while patient watching TV, at the office, traveling, or doing outdoor activities! It is a a versatile device allows the patient to strengthen almost every muscle part, and at the same time is light and takes up little space To increase the resistance as the muscles are developed, the user can simply add additional springs Many new types of expanders have appeared on the market. The most universal are those made of rubber. They can extend to a greater width, and at the same time have cables with different degrees of tension (Figure 2).

Figure 2:
2.1 Flexor group
The patient is standing with his/her back against the seat to which the Chest Expander Spring is attached. Patient's foot of operated limb anchored to the free hand gripper of the Chest Expander Spring. The patient pulls the operated limb forward against resistance of the spring keeping the knee straight then he/she allows his/her limb to return to its previous position (Figures 3a, 3b).
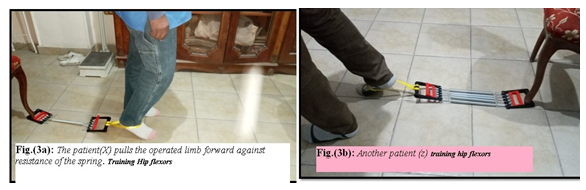
Figure 3:
2.2 Extensor group
The patient is standing and faces forward toward the seat to which the Chest Expander Spring is attached. Patient's feet are slightly apart and the foot of operated limb anchored to the free hand gripper of the spring. The patient pulls his/her operated limb straight backward against resistance of the spring with the knee straight then allowing the operated limb to return to its previous position (Figures 4a, 4b).
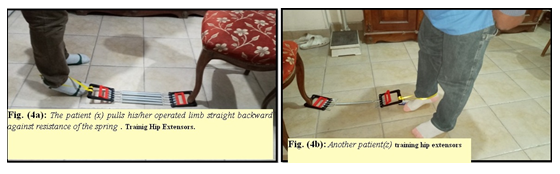
Figure 4:
2.3 Adductor group
The patient stands with his/her operated limb abducted. Patient's ankle of operated limb anchored to the handgrip end of the spring. Patient Keeps his/her operated limb straight, drawing it inward against resistance of the spring until it touches the other limb or moving the operated limb toward the center of his/her body Pausing in this position for a second before slowly returning to the starting position and repeat the exercise. Patient warranted never cross the midline or the other feet (Figures 5a, 5b, 5c, 5d).
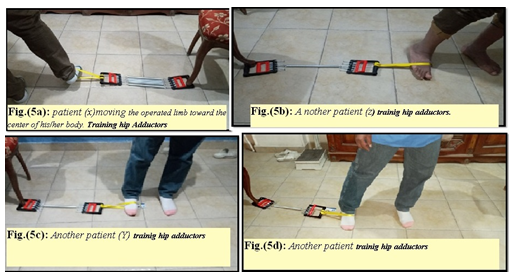
Figure 5:
2.4 Abductor group
Patient stands sideway from the seat to which the Chest Expander Spring is attached. He/she extends his/her operated limb out to the side against resistance of the spring then allows his/ her limb to return to its previous position (Figures 6a, 6b, 6c). Each exercise is done for 10-15 minutes twice daily then gradually building up to 20 to30 minutes 3 or 4 times a day. The whole exercises started by single spring within the expander then increase by one more every week of exercises. Total time of the program 5 weeks (equal 5 springs within the chest expander).
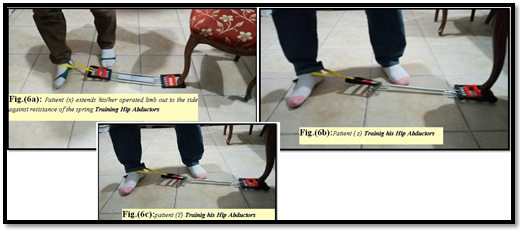
Figure 6:
3. Study Population
120 patients (84 males and 36 females) were enrolled in this prospective observational clinical study. All were complaining of varying complaint of osteoarthritis of hip joint and primary total hip arthroplasty had been done. The mean age 49.8 years (range, 38 to 65 years). All the patients completed the study and non was lost to follow-up. The study was initiated after receiving approval from the institutional ethics committee for research in accordance with the ethical standards laid down in the 1964 declaration of Helsinki and its later amendments. Also, a written consent had been obtained from all patients for participating in the study. Exclusion criteria involved patients below 20 years age, patients with revision hip arthroplasty, Arthroplasty due to fracture or causes other than osteoarthritis, patients with neuromuscular disorders that affect cognition or movement ability,
any condition that resulted in complete lack of sensation in the lower extremity or patients had any cardiovascular or pulmonary condition that would affect their ability to practice the physiotherapy program. Also patients with complicated prosthesis (as loosening, infection and implant failure were excluded.
4. Measurements
Patients completed a pre-operative assessment two weeks before THA bytwo of the authors and immediate postoperatively then two weeks after surgery while practicing the physiotherapy program. Again reassessment one week after last follow-up visit and another one after 6 months follow-up. Functional status was tested objectively through Performance-based tests included the Six Minute Walk Test [7, 8]Timed Up and Go test (TUG) [9].
|
- |
Immediate P.O. |
Last visit of F.U. |
6 months P.O. |
Clinical measures included hip range of motions (ROM) performed by two authors using a goniometer, Harris Hip Score (HHS) [10] and WOMAC activity Score [11]. To assess safety, descriptive data were reported. Safety was measured by assessing the number and type of adverse events during exercises treatment.
5. Results
After 6 weeks of training, the participants' showed greater change in 6-minute walking distance with mean increase 41.34%, and with a mean change of 117.12 meters. Up-and-go time test decreased 47.63% from the baseline measurements, with a mean change of 7.28 seconds. No cases showed high risk for falling. Clinical outcome measures showed that Passive range of hip motions was markedly improved at last follow-up visit by about 42.66%. The increase is more evident in hip flexors. Harris Hip Score (HHS) showed significant benefits from the program exercises with mean change of the score at last visit of follow-up 33.7 points. Changes of HHS shown in (Table I).
|
Pre-operative |
42,5 |
|
Immediate P.O. |
45.1 |
|
Last visit of F.U. |
77.3 |
|
6 months P.O |
87.2 |
Table 1: Changes of HHS shown.
Mean change of total WOMAC activity scores is shown in (Table 2).
|
Pain |
48 |
74 |
86 |
|
Stiffness |
47 |
69 |
79 |
|
Physical Functions |
52 |
68 |
81 |
Table 2: Results for pain, stiffness, and physical functioning measured using the WOMAC subscales.
P.O. = postoperative.
F.U. = Follow up
WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index and revealed significant improvement of the score following exercises at last visit of follow-up and 6 months postoperative. Regarding safety no adverse events occurred during practicing the program of exercises for all patients.
6. Discussion
Total hip arthroplasty (THA) is considered the gold standard treatment of end-stage hip arthritis in the presence of relevant functional impairments when conservative treatment options have failed. Also; the number of person who undergo THA has increased significantly over the last few years in our country due to governmental treatment policies which depends largely on state's expense also owing to increased number of patients suspended on operative waiting lists. Those patients (particularly at end-stage arthritis) would have muscular, soft tissue disorders and proprioceptive deficit owing to modified hip anatomy and biomechanics prior to surgery. The later might cause relevant hip joint stiffness, deformity, deficient muscle strength and walking difficulty. Success of THA is due to its predictable pain relief, functional recovery and improvement in quality of life facilitating the patient’s return to activities of daily living (ADLs) and even to labor activities [12]. Following surgery, variables rehabilitation programs had been proposed in clinical practice to strengthen the muscles, improve gait and coordination to optimize functional recovery [13]. Several studies supported such physiotherapy programs and showed better results when compared to minimal or even no intervention following THA [14, 15]. Not only joint functional gain was the benefit but also some studies emphasized that rehabilitation could reduce incidence of complications as prosthetic infection, osteoloysis, sublaxation or dislocation and variable thromboembolic disease [16].
Although there is still no routine rehabilitation protocol worldwide admitted after THA, However, most of these programs are supervised by healthcare professionals and are conducted using expensive training equipment’s so; it is considered costly and inconvenient particularly for those patients who live in remote areas, lack personal transportation, or those who have restricted mobility [17]. Adding to these difficulties certain patient specific factors like capability and readiness of patient to come to physiotherapy center, availability of assistance and finical burden beside lack of availability of rehabilitation center and place to do that specially in suburban area and country side [18]. This may explain the low rates of adherence that are reported for these rehabilitation programs. Furthermore, because of lack of accessibility and financial considerations, these types of exercise programs are difficult for patients to continue by themselves after the completion of any research studies [19]. In this study, We propose a strategy of rehabilitation program which can be carried out at the outpatient clinic or monitored at home utilizing a low cost equipment. Using the Chest Expander Spring device in Physiotherapy-based exercise rehabilitation after total hip replacement with progressive increase in the exercise resistance according to the patient capacity and compliance. Also, we have evaluated the clinical and functional outcomes of the program which showed significant improvement of the results relative to preoperative state. The program has many advantages including: availability of its equipment’s , low cost so no much financial burden, easiness to be done and monitored at home, office or even outdoor. Progression can be increased by increase the number of springs and duration of exercise which could be done by patient self and it does not need much human resources which is suitable for low income countries.
Our study has been supported by many previous reviews which stated that rehabilitation after hip and knee replacement whether carried out at the clinic or monitored at home, appears beneficial but type, intensity and duration of interventions were not consistently associated with outcomes [20]. Coulter et al. [13]; Artz et al. [19] mentioned that home-based physical rehabilitation, i.e. having received one or a few initial exercise instructions, seems equally effective as out-patient, supervised rehabilitation. Bandholm et al., [6] concluded that there is a continuous major need to improve functional recovery after hip and knee replacement, because studies to date have not found superiority of one exercise regime over another. However, whilst exercise-based rehabilitation seems superior to no or minimal rehabilitation after THA and TKA, other authors emphasized that among patients who had completed standard rehabilitation after hip fracture, the use of home-based functionally oriented exercises resulted in improved physical function at 6 months and 9 months [21]. At the same time many authors declared that there were no statistical differences between patients who received exercise program under the supervision of the physiotherapist and the patients who were treated with standardized home-based exercise program for the efficacy of treatment in the evaluation of pain, functional status, quality of life, and depression status. When the rehabilitation programs were analyzed for cost effectiveness, the supervised physiotherapy group was found to have higher costs [21].
7. Conclusion
Physiotherapy can improve muscle power, range of motion and coordination after total hip replacement and help prevent complications such as subluxation and thromboembolic disease which is associated with a greater probability of earlier discharge, which is in turn associated with a lower total cost of care. Provides pain relief, promotes rehabilitation and the reintegration of patients into ADLs. It also provides a better quality of life through the patients’ reintegration into social life Additionally, Patients who had completed rehabilitation program after hip arthroplasty the use of home-based functionally oriented exercises resulted in improved physical function. A low cost physiotherapy program can be utilized which is suitable for ruler, suburban area and country side.
8. Limitations of Our Study
Our study presents some limitations, namely small sample size. Also, follow-up period is somewhat short relatively and being an observational trial assessing short-term as well as medium-term clinical outcomes and lacking of comparative study. Additionally direct and indirect costs will be evaluated from a societal perspective. Study enrollment was not randomized and patients had a choice in where they received treatment, which may have affected outcomes.
References
- Pivec R, Johnson AJ, Mears SC, et al. Hip Arthroplasty. Lancet 380 (2012): 1768-1777.
- Maradit Kremers H Larson DR Crowson CS, et al. Prevalence of total hip and knee replacement in the United States.J Bone Jt Surg 97(2015): 1386-1397.
- Kurtz S, Ong K Lau E, Mowat F, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030.J Bone Joint Surg Am 89 (2007): 780-785.
- Siri B Winther, Olav A Foss, Otto S Husby, et al. A randomized controlled trial on maximal strength training in 60 patients undergoing THA Implementing maximal strength training into clinical practice Journal of physiotherapy 59 ( 2013): 219-226.
- Minns Lowe C, Barker KL, Dewey ME, et al. Effectiveness of physiotherapy exercise following hip Arthroplasty for osteoarthritis: A systematic review of clinical trials. BMC Musculoskeletal Disorders 10 (2009): 98-112.
- Bandholm T, Wainwright TW, Kehlet Rehabilitation strategies for optimization of functional recovery after major joint replacement, J Exp Orthop 5 (2018): 44-52.
- Harada N, Chiu V, et al. Mobility-related function in older adults: assessment with a 6-minute walk test. Archives of physical medicine and rehabilitation 80 (1999): 837-841.
- Steffen TM, Hacker TA, et al. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up and Go Test, and gait speeds. Physical Therapy 82 (2002): 128-137.
- Shumway-Cook A, Brauer S, Woollacott M.Predicting the probability for falls in community-dwelling older adults using the timed up and go test. Phys Ther 80 (2000): 896-903.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation.J Bone Joint Surg Am 51(1969): 737-575.
- Bellamy N1,Buchanan WW,Goldsmith CH,et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15 (1988):1833-1840.
- Freburger JK. An analysis of the relationship between the utilization of physical therapy services and outcomes of care for patients after total hip arthroplasty.Phys Ther80 (2000): 448-458.
- Okoro T, Lemmey AB, Maddison P, et al. An appraisal of rehabilitation regimes used for improving functional outcome after total hip replacement surgery.Sports Med Arthrosc Rehabil Ther Technol 4(2012): 5.
- Trudelle-Jackson E, Smith SS. Effects of a late-phase exercise program after total hip arthroplasty: A randomized controlled trial.Arch Phys Med Rehabil 85 (2004): 1056-1062.
- Chiung-Jui Su D, Yuan K, Weng S, et al. Can Early Rehabilitation after Total Hip Arthroplasty Reduce Its Major Complications and Medical Expenses? Report from a Nationally Representative Cohort.Biomed Res Int(2015): 641958.
- Galea MP, Levinger P, Cimoli C, et al. A targeted home-and center-based exercise program for people after total hip replacement:a randomized clinical trial. Archives of physical medicine and rehabilitation 89 (2008):1442-1447.
- Di Monaco M, Vallero F, Tappero R, et al. Rehabilitation after total hip arthroplasty: A systematic review of controlled trials on physical exercise programs.Eur J Phys Rehabil Med 45(2009): 303-317.
- Artz N, Elvers KT, Lowe CM, et al. Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis.BMC Musculoskelet. Disord 16 (2015):15.
- Sinnott KA, Hipango J,Dunn JA,et al. Rehabilitation after total joint replacement: a scoping study. Disabil Rehabil 40 (2018): 1718-1731.
- Büker N,Kitis A,Akkaya S,et al. Comparison of the results of supervised physiotherapy program and home-based exercise program in patients treated with arthroscopic-assisted mini-open rotator cuff repair. Eklem Hastalik Cerrahisi 22 (2011): 134-149.
