Chemical Intolerance in Patients With Nasal Inflammatory Disorders Using QEESIⓒ
Article Information
Byung Woo Kwon, Woo Yong Bae*, Nam Yoon Jung, Chang Bae Lee, Daeyeon Kim
Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, Dong-A University, Busan, Korea
*Corresponding Author: Woo Yong Bae, Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, Dong-A University, Daesingongwon-ro, Seo-Gu, Busan, 49201, Republic of Korea
Received: 13 June 2019; Accepted: 27 June 2019; Published: 01 July 2019
Citation: Byung Woo Kwon, Woo Yong Bae, Nam Yoon Jung, Chang Bae Lee, Daeyeon Kim. Chemical Intolerance in Patients With Nasal Inflammatory Disorders Using QEESIⓒ. Archives of Clinical and Biomedical Research 3 (2019): 257-271.
View / Download Pdf Share at FacebookAbstract
Background: In some of the inflammatory disorders, such as chronic rhinosinusitis (CRS), non-allergic rhinitis (NAR), or allergic rhinitis (AR), environmental agents can incite or exacerbate the symptoms of each disease. The aim of the study was to investigate the relationship of chemical intolerance in the nasal inflammatory disorders using QEESI©.
Methods and Findings: Subjects were 261 outpatients who presented themselves for rhinologic evaluation. Subjects completed the QEESI© (Korean version) during the first visit. The prevalence rate of the very suggestive scores in all the rhinologic disease cases overall and CRS, NAR, and AR cases was examined and compared between each disease group. We compared the chief complaint and ARIA classification of AR with the degree of suggestive chemical intolerance. Of 261 patients, 45 patients (17.24%) were categorized into very suggestive of risk of chemical intolerance. The prevalence rate of very suggestive was higher in female (16.33%) than in male (9.82%). Among the CRS, NAR and AR groups, the number of very suggestive cases were 17 (18.47%), 4 (15.38%), and 11 (13.25) respectively and a statistical difference was not observed between each group (P>.05). When we compared the chief complaint according to the degree of severity, rhinorrhea and nasal obstruction was the chief complaint in the cases of very suggestive scores.
Conclusions: We suggest that control of chemical intolerance can be helpful to treat nasal inflammatory disorders and QEESI© may be useful questionnaire for the screening of chemical intolerance in the nasal inflammatory disorders.
Keywords
Chemical intolerance; QEESI; Chronic rhinosinusitis; Non-allergic rhinitis; Allergic rhinitis
Article Details
Introduction
Human nasal mucosa scrub particulate and water soluble volatile compounds from inhaled air, protect airways from injury caused by inhaled allergens, irritants, bacteria, and viruses and humidify and warm the inspired air. Processes to control the inhaled air are under strict physiological control and depend on local mucosal feedback and sensory and autonomic reflexes [1]. Common chemical sense in the nasal cavity is a nasal sensation provoked by airborne chemicals which are distinct from taste and smell. This sense results from the exposure of trigeminal nerve endings to irritants. Several protein receptors on cell membranes are the activation site for chemical irritants. Neurogenic inflammation is a well defined process by which inflammation is triggered by the nervous system. Sensory nerves act as both afferent and efferent nerves for neurogenic inflammation. A variety of chemical irritants trigger the nervous system, induce the release of neuropeptides, such as substance P, neurokinin A and then produce vasodilatation, edema, and other manifestations of inflammation, known as neurogenic inflammation [2, 3]. Chemical intolerance is the subjective report of feeling ill from low-level exposure to a variety of common outdoor and indoor odorants, such as auto emissions, pesticides, carpet glue, drying paint, and perfume [4].
Multiple chemical sensitivity (MCS) is an acquired disorder that develops after some identifiable environmental exposure and a kind of chemical intolerance [5, 6]. MCS can be referred to in many ways such as Idiopathic Environmental Intolerance, Chemical sensitivity or Intolerance and Toxicant-induced loss of tolerance [4]. To screen for MCS, several questionnaires have been developed. However, the majority of instruments for testing are very cursory and there is a lack of a uniform approach [4, 7, 8]. A tool that could gauge the multi-system symptoms and multiple intolerances reported by these patients with good validity and reliability would be useful for research. The Quick Environmental Exposure and Sensitivity Inventory (QEESI©) is a questionnaire, which was developed by Miller and Prihoda, for the screening of MCS [9, 10. Chemical intolerance such as MCS may be associated with many diseases such as rhinosinusitis, polyps, allergic rhinitis, recurrent otitis media and other ENT problems [11-13]. However, there was not investigated chemical intolerance in nasal inflammatory disorders using QEESI©.
The aim of the study was to investigate the relationship of chemical intolerance in the nasal inflammatory disorders using QEESI©.
Materials and Methods
- Subjects
Subjects were outpatients who presented themselves for rhinologic evaluation at Dong-A university medical center between January, 2012 and December, 2012. The subjects were 261 patients (163 males, 98 females) and the mean age was 40.66 ± 14.12. Nasal inflammatory disorders were classified into chronic rhinosinusitis (CRS), Non-allergic rhinitis (NAR) and allergic rhinitis (AR). There were 92 CRS (54 males, 38 females), 26 NAR (13 males, 13 females), and 83 AR (57 males, 26 females) patients. A control group was selected from among patients without rhinologic disease and 98 were enrolled.
- Diagnostic study of disease groups
Most subjects were stratified into 3 groups based on whether they had CRS, NAR or AR. The CRS cases were evaluated with symptoms, endoscopic findings, or a PNS CT and diagnosed based on the minimal criteria for CRS [14]. NAR and AR were diagnosed with symptoms including chief complaints, endoscopic findings and the results of multiple allergen simultaneous test (MAST) using MAST CLA Allergy test (Hitachi Chemical Diagnostics, Inc, CA, USA). AR patients were classified into 4 groups using the ARIA classification [15].
- Prevalence study of disease groups
Subjects completed the QEESI© (Korean version) during the first visit. The degree to which MCS is suggested is classified in 4 degrees - very suggestive, somewhat suggestive, problematic and not suggestive - using 2 categories (chemical intolerance and symptom severity) (Table 1). We examined the prevalence rate of the very suggestive scores in all the rhinologic disease cases overall and CRS, NAR, and AR cases and compared between each disease group. Comparisons were also performed separately for male and female patients.
- Analysis of scores of 50 items on 5 scales
We calculated the average of the 50 items on five scales. On each scale, We compared the highest total score and the five highest scores in 10 items among males and females and for each of the 3 disease groups.
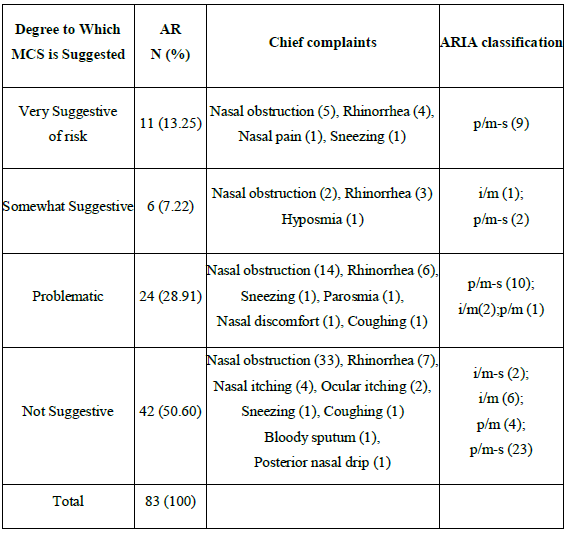
- Analysis of AR characteristics with the degree of suggestive chemical intolerance
We examined the chief complaint and classified the patients according to ARIA classification. We compared the chief complaint and ARIA classification of AR with the degree of suggestive chemical intolerance. We also analyzed the results of the MAST.
- Statistical analysis
All the statistical analyses were performed using SPSS ver. 16. Comparison of the prevalence rate of very suggestive cases between control groups and disease groups was done using the Chi-square test or Fisher's exact test.Comparison of the prevalence rate of very suggestive cases between males and females was done using the Chi-square test or Fisher's exact test in all the rhinologic diseases cases overall with the rate from each of the 3 groups. Comparison of the prevalence rate of very suggestive cases of each of the 3 groups was performed using the Chi-square test or Fisher's exact test. Comparison of the scores of 50 items of 5 subscales in QEESI©between males and females was done using the Mann-Whitney test, because the data were not normally distributed as a result of Shapiro-Wilks test. Lastly, Comparison of the scores of the 50 items for each of the 3 disease groups was done using Kruskal Wallis test. P<.05 was considered statistically significant.
- Informed consent
We obtained the informed consent from each patient and the study was approved by the institutional review board of Dong-a University hospital in Busan, Korea.
Results
- Prevalence rates of chemical intolerance for rhinologic diseases
Of 261 patients, 45 patients (17.24%) were categorized into very suggestive of risk, 27 (10.34%) into somewhat suggestive and 67 (25.67%) into problematic (Table 1). Eight subjects in the control group were categorized into very suggestive of risk and a statistical difference between the control groups and the disease group was observed (P<.05). Of very suggestive cases, 25 were males (15.33%) and 20 were females (20.40%). A statistical difference between males and females in the very suggestive cases was not observed (P>.05).
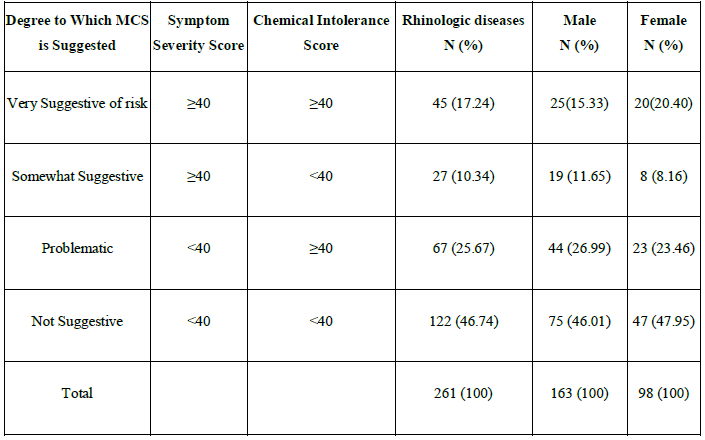
MCS: Multiple chemical sensitivity
Table 1: MCS risk criteria using symptom severity score and chemical intolerance score and prevalence rates of chemical intolerance for the rhinologic diseases
- Prevalence rates of chemical intolerance in each disease group
Among the CRS, NAR and AR groups, the number of very suggestive cases was 17 (18.47%), 4 (15.38%), and 11 (13.25%), respectively and a statistical difference was not observed between each group (Table 2) (P>.05).
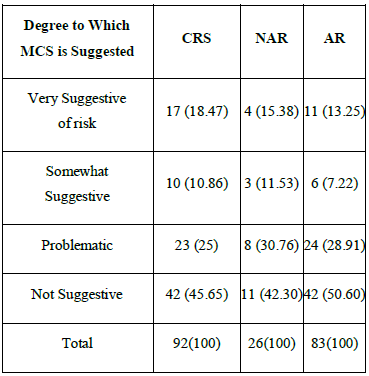
MCS: Multiple chemical sensitivity; CRS: Chronic rhinosinusitis; NAR: Non-allergic rhinitis;
AR: Allergic rhinitis
Table 2: Prevalence rates of chemical intolerance at each disease group
- Analysis of scores of 50 items on 5 scales 3.1 Chemical intolerance
The five highest scores among the total patients on the survey in this area were in the following categories: tobacco smoke
- paint or paint thinner > insecticide >cleaning products >new furnishings. The mean score of those with exposure to tobacco smoke was 4.36 ± 3.37 (Table 3). There was no significant differences in malesand females across all categories
(P>.05). NAR had the highest total score (35.81± 25.77) among CRS, NAR and AR groups (Table 5).
3.2 Other intolerances
The five highest scores among the total patients on the survey in this area were in this order: classic allergic reaction >chlorinated tap water >food or food additives >alcohol in small amounts >food cravings or feeling ill if meal missed. The mean score of those with classic allergic reactions was 3.34 ± 3.58 (Table 3). There was no significant differences in males and females across all categories (P>.05). Among the CRS, NAR and AR groups, NAR group had the highest total score (19.27±18.44) on this scale. The highest score among the 10 items in all groups was the classic allergic reaction in all groups (Table 4).
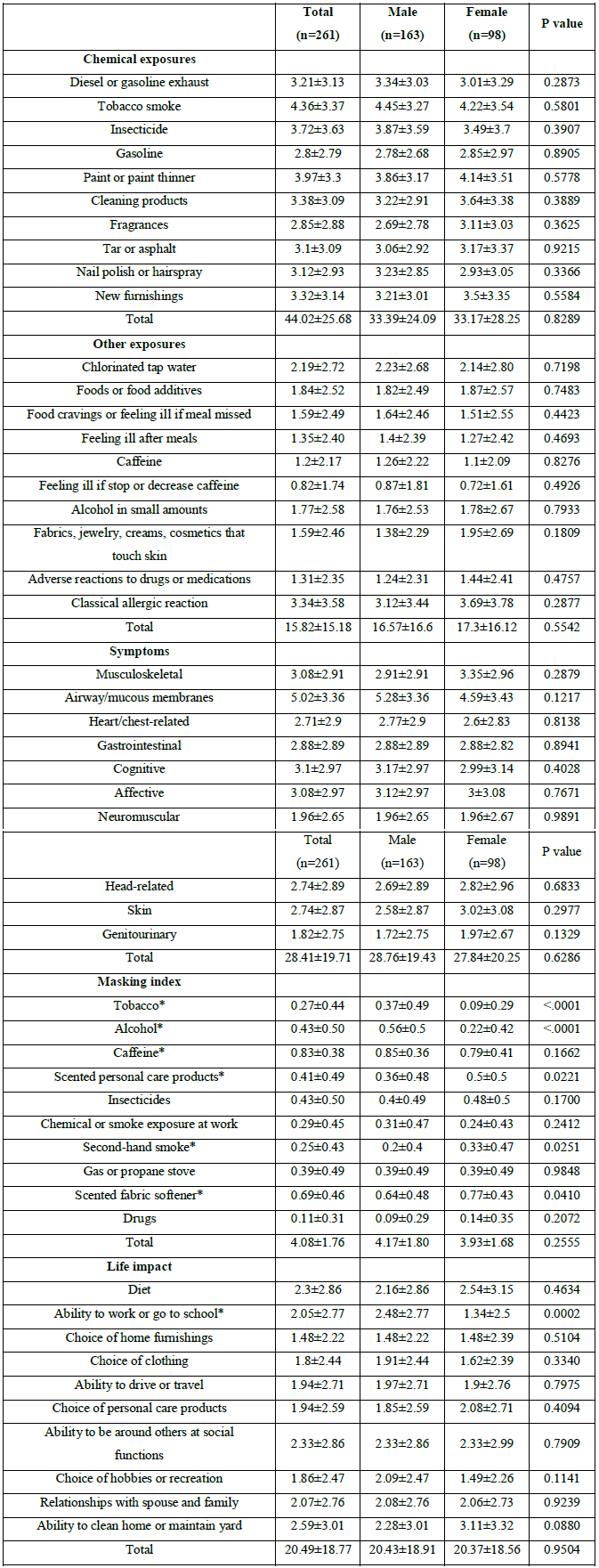
*p<0.05 as compare between male and female
Table 3: Mean scores of each scale among males and females
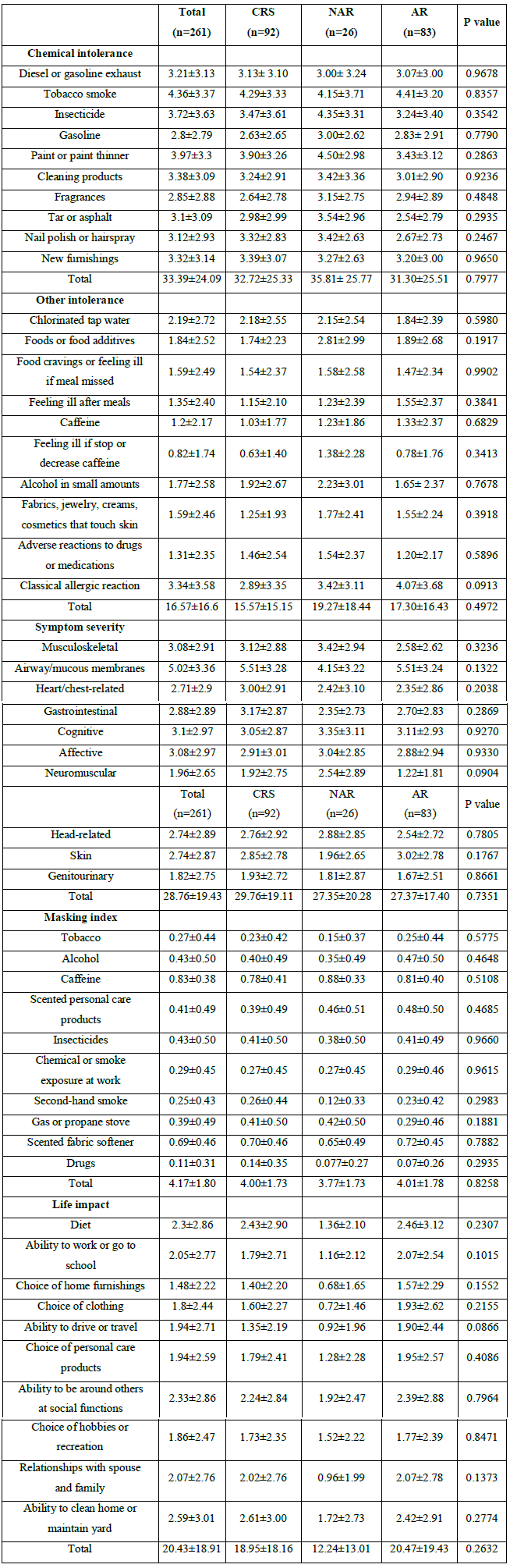
Table 4: Mean scores of each scale in 3 groups
MCS: Multiple chemical sensitivity; CRS: Chronic rhinosinusitis; NAR: Non-allergic rhinitis; AR: Allergic rhinitis
ARIA: Allergic rhinitis and its impact on asthma; i:intermittent; p: persistent; m: mild; m-s: moderate-severe+
Table 5: Chief complaints and ARIA classification according to the degree of the suggestive MCS in allergic rhinitis patients
3.3 Symptom severity
The five highest results among the total patients on the questionnaire in this area were in this order: airway/mucous membranes >cognitive >affective >musculoskeletal >gastrointestinal. The mean score of those with airway/mucous membrane symptoms was 5.02 ± 3.36. The airway/mucous membrane group had the only score, which exceeded 5.0 (Table 4). There was no significant differences in males and females across all categories (P>0.05).The highest score among the 10 items in all 3 groups was for the airway/mucous membrane (Table 4).
3.4 Masking index
The five highest results among the total patients on the questionnaire in this area were in this order: caffeine >scented fabric softener >alcohol >insecticides >scented personal care products. The mean score of those with caffeine sensitivity was 0.83 ± 0.38 (Table 4). The scores for tobacco, alcohol showed significantly higher in males than females and those for scented personal care products, second-hand smoke and scented fabric softener showed significantly higher in females than males (P<.05). The highest score among the 10 items in all 3 groups was for caffeine. But a statistical difference among disease groups was not observed (P>0.05) (Table 4).
3.5 Life impact
The five highest results among the total patients on the survey in this area were in this order: ability to clean home or maintain yard >ability to be around others at social functions >diet >relationships with spouse and family >ability to work or to go to school. The mean score of ability to clean the home or maintain the yard was 2.59 ± 3.01 (Table 3). The score for ability to work or go to school showed a significant higher in males than in females (P<0.05). The highest score among disease groups was observed in the AR group. The adverse life impact among disease groups were different in regard to the ability to clean the home or maintain the yard in CRS, ability to be around others at social functions in NAR and diet in AR group (Table 4).
3.6 Analysis of AR characteristics with the degree of suggestive chemical intolerance
The subjects were 83 patients (57 males, 26 females) and the mean age was 36.4 ± 14.4. The most common complaint symptoms were nasal obstructions and the next most common was rhinorrhea. According to the ARIA classification, the most common class was persistent/moderate severe. The result of the MAST was that house dust mites were the most common allergen.
Of 83 patients, 11 patients (13.25%) were categorized into the very suggestive of risk classification and a statistical difference between the male and female very suggestive cases was not observed (P>.05).
When we compared the chief complaint according to the degree, in the cases of very suggestive scores, rhinorrhea occurred as much as nasal obstructions. In the very suggestive cases, all have the persistent/moderate-severe classification (Table 5).
Discussion
Miller and Prihoda developed the QEESI© to assist researchers and clinicians in evaluating patients and populations for MCS [9, 10]. They reported that 7% cases in the control group were very suggestive and a higher percentile in the specific groups. Hojo et al., investigated MCS using QEESI© in a Japanese population and reported that about 4% of the general population could be classified at the very suggestive level [16-18]. The prevalence rate of the very suggestive cases in this study was 17.24% and higher than in the control groups or general populations of other studies. We suggest that it may be concerned environmental or genetic factors.
Many studies reported that the prevalence rate of MCS among middle-aged females was higher than among males [19-22]. Female predominance may be attributed to female vulnerability or more frequent exposure to the chemical irritants. The result of this study are consistent with those of previous studies, which showed that the prevalence rate of very suggestive was 16.33% in female and 9.82% in male. Many researchers have reported that various sickness and diseases, including migraine, fibromyalgia, asthma and sinusitis were associated with MCS [22-25]. Meggs and Cleveland performed a rhinolaryngoscopic examination of 10 patients with MCS [12]. They suggested that exposure to chemical irritants can induce chemical sensitivity, especially with chemical irritants that induce asthma and/or rhinitis, but the mechanisms by which individuals become sensitive to multiple diverse chemicals, part of the diagnostic criteria for MCS, are not clear. Baldwin suggested that chemical intolerance may serve to amplify these traditional immune-related disorders and/or suggests that having asthma or hay fever could make one more vulnerable to chemical intolerance [13]. We hypothesized that the nasal inflammatory disorders, such as CRS, AR, or NAR may be associated with chemical intolerance and used the QEESI© to evaluate the prevalence rate of chemical intolerance in the nasal inflammatory disorders. In this study, the prevalence rate of very suggestive cases in CRS, AR and NAR was 18.47%, 15.38% and 13.25% respectively. We suggest that nasal inflammatory disorders may be associated with the chemical intolerance.
We compared the 50 items using 5 scales among the disease groups. For chemical intolerance, tobacco smoke had the highest score in CRS and AR patients. This means that tobacco smoke may influence the symptoms of CRS and AR. In other intolerances, the classic allergic reaction was the highest score for AR patients, as expected. Mean scores of symptom severity and the masking index among disease groups were similar to total scores. In life impact the highest score among disease groups was different, but the major impact was similar. Disease groups were impacted in the area of diet, ability to be around others at social functions and the ability to clean the home or maintain the yard.
MCS and respiratory disorders, especially asthma or AR, can be closely related and many nonspecific environmental agents can trigger the symptoms of those disorders [13, 26]. We examined the chief complaints and classified the patients into 4 groups by ARIA classification [15] and compared the chief complaints and ARIA classification of AR with the degree of suggestive MCS. The chief complaint in the AR cases was nasal obstruction, but in very suggestive cases, rhinorrhea occurred as much as nasal obstruction. In the very suggestive cases, all cases were classified into the persistent/ moderate-severe classification. The reason is not clear, but it may be that patients with more severe symptoms visit the
hospital more or environmental factors may aggravate the symptoms.
Chemical intolerance may be one of the causes of nasal inflammatory disorders. We suggest that control of chemical intolerance can be helpful to treat nasal inflammatory disorders and QEESI© may be useful questionnaire for the screening of chemical intolerance in the nasal inflammatory disorders.
Funding
This work was supported by the Dong-A University research fund.
Acknowledgments
This study was performed after permission from Dr. Claudia S. Miller [University of Texas Health Science Center at San Antonio],Copyright holder of QEESI©
Disclosure
The authors have no potential conflicts of interest to disclose.
Author Contribution
Conceptualization: Kwon BW, Bae WY. Data curation: Kim SJ, Jung DW Jung NY. Formal analysis: Jo KS. Writing -
original draft: Kwon BW. Writing - review & editing: Bae WY, Jo KS.
Ethics statement
The present study protocol was reviewed and approved by the institutional review board of Dong-A University College of Medicine (Reg. No. 11-157). Informed consent was submitted by all subjects when they were enrolled.
References
- Baraniuk JN, Merck SJ. Neuroregulation of human nasal mucosa. Ann N Y AcadSci 1170 (2009): 604-609.
- Sarin S, Undem B, Sanico A, Togias A. .The role of the nervous system in rhinitis. J Allergy ClinImmunol 118 (2006): 999-1016.
- Bell IR, Miller CS, Schwartz GE, Peterson JM, Amend D. Neuropsychiatric and somatic characteristics of young adults with and without self-reported chemical odor intolerance and chemical sensitivity. Arch Environ Health 51 (1996): 9-21.
- Tai CF, Baraniuk JN. Upper airway neurogenic mechanisms.CurrOpin Allergy ClinImmunol 2 (2002): 11-19.
- Meggs WJ. Neurogenic inflammation and sensitivity to environmental chemicals. Environ Health Perspect 101 (1993): 234-238.
- Undem BJ. Inflammation-induced plasticity of the afferent innervation of the airways. Environ Health Perspect (2001): 567-571.
- Australian Government: A Scientific Review of Multiple Chemical Sensitivity: Identifying Key Research Needs; Draft Report prepared by the National Industrial Chemicals Notification and Assessment Scheme (NICNAS) and the Office of Chemical Safety and Environmental Health (OCSEH) 2010: 1-95. http://www.nicnas.gov.au/Media/Latest_News/MCS.asp
- Cullen MR. The worker with multiple chemical sensitivities: an overview. Occup Med 2 (1987): 655-661.
- Multiple chemical sensitivity: a 1999 consensus.Arch Environ Health 54 (1999): 147-149.
- Kreutzer R, Neutra RR, Lashuay N. Prevalence of people reporting sensitivities to chemicals in a population-based survey. Am J Epidemiol 150 (1999): 1-12.
- Meggs WJ, Dunn KA, Bloch RM, Goodman PE, Davidoff AL. Prevalence and nature of allergy and chemical sensitivity in a general population. Arch Environ Health 51 (1996): 275-282.
- Miller CS, Prihoda TJ. The environmental exposure and sensitivity inventory (EESI): a standardized approach for measuring chemical intolerances for research and clinical applications. ToxicolInd Health 15 (1999): 370-385.
- Miller CS, Prihoda TJ. A controlled comparison of symptoms and chemical intolerances reported by Gulf War veterans, implant recipients and persons with multiple chemical sensitivity. ToxicolInd Health 15 (1999): 386-
- Jeon BH, Lee SH, Kim HA. A validation of the Korean version of QEESI© (the quick environmental exposure and sensitivity inventory) Korean J Occup Environ Med 24 (2012): 96-114.
- Miller CS. Toxicant-induced loss of tolerance--an emerging theory of disease? Environ Health Perspect 105 (1997): S445-S453.
- Meggs WJ, Cleveland CH Jr. Rhinolaryngoscopic examination of patients with the multiple chemical sensitivity syndrome. Arch Environ Health 48 (1993): 14-18.
- Baldwin CM, Bell IR, O'Rourke MK. Odor sensitivity and respiratory complaint profiles in a community-based sample with asthma, hay fever, and chemical odor intolerance. ToxicolInd Health 15 (1999): 403-409.
- Report of the Rhinosinusitis Task Force Committee Meeting. Alexandria, Virginia, August 17, 1996. Otolaryngol Head Neck Surg 117 (1997): S1-S68.
- Hojo S, Kumano H, Yoshino H, Kakuta K, Ishikawa S. Application of Quick Environment Exposure Sensitivity Inventory (QEESI) for Japanese population: study of reliability and validity of the questionnaire. Toxicol Ind Health 19 (2003): 41-49.
- Hojo S, Yoshino H, Kumano H, Kakuta K, Miyata M, Sakabe K, Matsui T, Ikeda K, Nozaki A, Ishikawa S. Use of QEESI questionnaire for a screening study in Japan. ToxicolInd Health 21 (2005): 113-124.
- Hojo S, Ishikawa S, Kumano H, Miyata M, Sakabe K. Clinical characteristics of physician-diagnosed patients with multiple chemical sensitivity in Japan. Int J Hyg Environ Health 211 (2008): 682-689.
- Caress SM, Steinemann AC. A review of a two-phase population study of multiple chemical sensitivities. Environ Health Perspect 111 (2003): 1490-1497.
- Eis D, Helm D, Mühlinghaus T, Birkner N, Dietel A, Eikmann T, Gieler U, Herr C, Lacour M, Nowak D, et al. The German Multicentre Study on Multiple Chemical Sensitivity (MCS). Int J Hyg Environ Health 211 (2008): 658-681.
- Park J, Knudson S. Medically unexplained physical symptoms. Health Rep 18 (2007): 43-47.
- Kreutzer R, Neutra RR, Lashuay N. Prevalence of people reporting sensitivities to chemicals in a population-based survey. Am J Epidemiol 150 (1999): 1-12.
- Taylor RR, Jason LA. Chronic fatigue, abuse-related traumatization, and psychiatric disorders in a community-based sample.SocSci Med 55 (2002): 247-256.
- Staudenmayer H, Binkley KE, Leznoff A, Phillips S. Idiopathic environmental intolerance: Part 2: A causation analysis applying Bradford Hill's criteria to the psychogenic theory. Toxicol Rev 22 (2003): 247-261.
- Lacour M, Zunder T, Schmidtke K, Vaith P, Scheidt C. Multiple chemical sensitivity syndrome (MCS)-- suggestions for an extension of the U.S. MCS-case definition. Int J Hyg Environ Health 208 (2005): 141-151.
- Krouse JH. The unified airway--conceptual framework.OtolaryngolClin North Am 41 (2008): 257-266.
- Kimber I, Basketter DA, Dearman RJ. Chemical allergens--what are the issues? Toxicology 268 (2010): 139-142.
- Bousquet J, Van Cauwenberge P, Khaltaev N; Aria Workshop Group; World Health Organization. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol 108 (2001): S147-S334.
