Cervical Cancer - Its Prevalence, Risk factors, Imaging, and Treatment
Article Information
Mahrukh Ikram*, Muhammad Arslan, Iqra Fasih
Institute of Microbiology and Molecular Genetics, University of the Punjab, Lahore, Pakistan
*Corresponding author: Mahrukh Ikram, Institute of Microbiology and Molecular Genetics, University of the Punjab, Lahore, Pakistan.
All authors contributed significantly
Received: 28 June 2021; Accepted: 07 July 2021; Published: 15 July 2022
Citation: Mahrukh Ikram*, Muhammad Arslan, Iqra Fasih. Cervical Cancer - Its Prevalence, Risk factors, Imaging, and Treatment. Fortune Journal of Health Sciences 5 (2022): 426-434
View / Download Pdf Share at FacebookAbstract
Cervix uteri is a leading type of cancer exclusive to women. It is gradually spreading over different regions of the world without any prominent cause or reason behind it. This disease affects the lower part of the uterus (start of the cervix area). Most reports advocate the role of Human Papilloma Virus (HPV) infection in developing this cancer. Environmental and age-related factors also play an important role, and these areas are open for research to discover exact relationships. However, in this article, we have summarized and revealed some important statistics about cervix uteri cancer that describe its epidemiology, risk factors, relation to age, treatments, staging and similar aspects.
Keywords
Human Papilloma Virus, Low and Middle-Income Countries, Human Papilloma virus
Article Details
1. Introduction
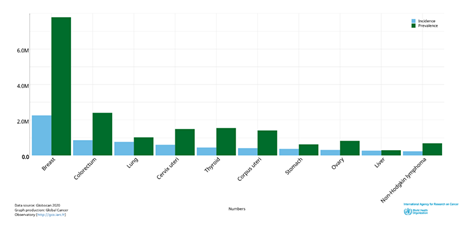
After breast, colorectal, and lung cancer, cervical cancer is the fourth most common cancer among females, and this trend is the same for the whole world. [1, 13] It is the only gynecological cancer with incidence, prevalence, and mortality rates still soaring and no signs of immediate deceleration [15]. Cervix uteri cancer mainly affects females of reproductive age [17]. In 2012, there was an estimation of 265700 deaths per year and 527600 new cases. The incidence rate of cervical cancer is relatively high in Low and Middle-Income Countries (LMICS), and thus it is the second most common cancer in developing and low-income nations. The same goes for the mortality rate, which is the third most common cancer [1, 5]. It has been seen that above 85% of new cases of cervical cancer in economically unstable countries, whereas about 90% of fatalities occur in those countries (24). The data and studies show that Human Papillomavirus (HPV) and cervical cancer shares a connection, especially with human papillomavirus persistent infection [1, 5, 6].
Estimated number of cases worldwide, females, all ages (excel, NMSC)
2. General Trend and Epidemiology of Cervix Uteri Cancer
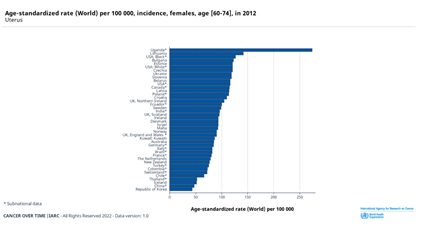
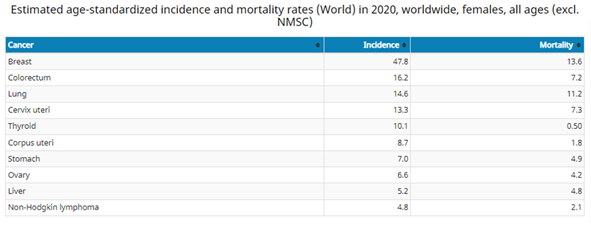
According to the research and recent data analysis, Chile, Uganda, and Czechia are the leading countries with the most reported cases of cervix uteri cancer. In Chile, this cancer is usually prevalent in young females whereas, in Czechia, older women are usually affected. Uganda is the most prominently affected in this concern for a significant number of all ages affected by this affliction. Further, as a general trend about the cervix uteri (cervix) cancer, it can be observed (Figure 1.1-1.4) that the tendency to develop cervix uteri cancer increases with advancing age, which is mostly observed for all cancer forms. Different trends and numbers of cancer cases are elaborated in the graphical figures 1.1 to 1.4, representing a clear variation trend within different countries. Figure 1.5 shows a graph and table to compare the number of cases and mortality rates of various cancer types. It can be observed that cervix uteri cancer comes at number 4 with a mortality rate of 7.3. This value is just lower than lung cancer which is a renowned fatal cancer from.
3. Risk Factors
Smoking, oral contraceptives and some sexual practices are reported to increase the prevalence of cervix uteri cancers. Thus they are likely to be termed as risk factors for cervix uteri cancer. The risk of cervix uteri cancer increases with cigarette smoking [2]. Having more than one sexual partner and sexual intercourse at a very young age (less than 16 years) can elevate the risk of cervix uteri cancer. In the case of cervical cancer, oral contraceptives are a very significant risk factor. It is a well-studied fact that there is a direct relation between the period of use of oral contraceptives and the relative risk of cervix uteri cancer. The use of oral contraceptives for five years or more than 5 years doubles the risk of cervix uteri cancer. A study also shows that oral contraceptives are an independent risk factor in causing cervix uteri malignancy [2, 6].
4. Cervical cancer staging system
Staging systems are used to find out the stage of cancer. They have many goals. They help in the formation of a treatment plan, in prognostic approaches, results of any therapy evaluation and assessment, and sharing and disseminating information between different national and international treatment centers and thus play a vital role in research and investigation. Validity, practicality, and reliability must characterize any good staging system [18]. After the 1950s, The International Classification of the Stages of Carcinoma of the Uterine Cervix states there are almost seven changes made in the stages of uterine cervix carcinoma. Surprisingly all the alterations occur in the first stage [16]. In 1954, the International Federation of Gynecology and Obstetrics (FIGO) was founded [13, 19]. This is now globally used as a cervical cancer staging system. There are different stages and sub-stages these stages help in diagnosis, prognosis, and in the decision-making of the treatment method or type [1, 19] There was an up-gradation of the cervical cancer staging system in 2018 by FIGO [3, 19].
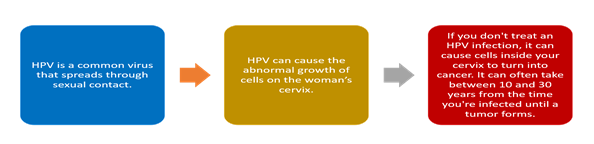
5. Cervix uteri cancer and Human Papilloma Virus relation:
It is now strongly believed that cervix uteri cancer and Human Papillomavirus (HPV) share a very strong connection. The human papillomavirus causes an infection in the uterine cervix. Infection with HPV is very much common in young girls and is well cleared by the host immune system. In some cases, HPV cause latent or persistent infection. In this case, HPV cause transformation in which it converts normal cell into oncogenic cells. This transformation occurs at the Squamous Columnar Junction (SJC). Those HPV genotypes that are known to cause oncogenic transformation are oncogenic HPV strains. Among more than 100 genotypes of HPV, there are only 15 HPV genotypes that are oncogenic. In those 15 oncogenic HPV genotypes, HPV16 and HPV 18 are those genotypes that cause most of the cervix uteri cancer [21]. Now, there are two steps of prevention that can be opted for the protection of cervix uteri cancer. There is primary prevention that HPV vaccination does. Besides primary prevention, secondary prevention helps detect and treat true precursor lesions. HPV16/18 and HPV 6/11/16/18 vaccines are used in primary prevention in most world countries. It is now a well-established concept that both primary and secondary prevention could weaken the link between HPV and cervix uteri cancer [22].
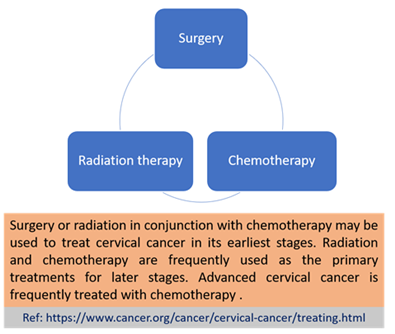
6. Treatment and management of cervix uteri cancer
If the cervix uteri cancer was diagnosed at a very early stage, then surgery is the best option as it removes cancerous cells. Radial hysterectomy, cervical conization, or total simple hysterectomy can be performed for timely treatment. The choice depends on the cancer stage and spread extent. Radiation therapy is used when metastasis occurs and surgery seems ineffective. The development of computer technology, well-developed delivery techniques, and imaging methods have made radiation therapy easier and more accessible. Radiation therapy is also used as adjuvant therapy; it is administered with other treatment and management methods [1]. Chemoradiation is also used for the treatment of local cervix uterine cancer [11]. Invasive surgery was considered the best option for the treatment of cervix uteri cancer for a long period of time, but with the advancements in biological target therapy, radio imaging technology, and radiotherapeutic approaches, there has been a drastic decline in invasive surgery usage. They all changed the whole scenario of cervix uteri cancer management [4]. The selection of the method of management and treatment of cervix uteri cancer mainly depends on the stage, patient health status, and on resources available [1].
7. Post Treatment Follow up and Recurrence of cervix uteri cancer:
Studies have shown that after primary treatment, cancer can return. This usually happens from 7-36 months. Hence, it is stressed that there should be more frequent follow-ups in this period. Recurrence usually occurs in pelvic and para-aortic. There are chances of metastases developing in a very distant region. If recurrence occurs in a local area of the body, then radiation therapy and invasive surgery can be used for the management of cervix uteri cancer [1].
8. Role of imaging in Cervical cancer
Diagnosis of cervical cancer is usually done by imaging. It is used to know about the metastatic condition, tumor extent, lymph node extension, and tumor size. Imaging determines the staging, which in turn determines the best therapeutic method that is implemented to treat cervix uteri cancer. It is done by many methods like Magnetic Resonance Imaging (MRI) and transvaginal/transrectal ultrasound (TVS/TRS), positron emission tomography-CT (PET-CT), and Computed Tomography (CT).
Every method has advantages and is used according to the requirement and accessibility. There are recent advancements made in imaging technology. Novel imaging techniques have the advantage of better quantification of characteristics of tumor, extent, metastasis, and stage [9, 17] with the help of Integrated positron emission tomography/computed tomography (PET/CT) with 2-[18F] Fluoro-2-Deoxy-D-Glucose (FDG), it is now possible to obtain anatomic imaging and glucose metabolism results. This saves cost, time, and labor as it does not use multiple devices. FDG-PET/CT is widely used for staging, re-staging, treatment optimization, and monitoring purposes [20].
9. Advancements in management of cervix uteri cancer:
With the development of science and technology, much different advancement are made in order to improve the management of cervix uteri cancer.
9.1. Immunotherapies:
One of the most recent approaches to treat cervical uteri cancer is immunotherapy. It is mainly used in patients with tumors forming metastases and undergoing metastasis. There are several clinical trials still in the progress phase that used chemotherapy and radiation therapy in combination with immunotherapy. There are several target points at which we can limit cancer. These target points include programmed death-1(PD-1), programmed death-ligand 1 (PDL-1), programmed death-ligand 2(PDL-2), and inhibition of activated T cells through cytotoxic T lymphocyte antigen-4 [10, 14].
9.1.1. US Food and Drug Administration (FDA) approved Immunotherapeutic drugs:
Recently, some immunotherapies have been approved by the Food and Drug Administration USA for the treatment of cervix uteri cancer. In 2017 Pembrolizumab was approved by US Food and Drug Administration but was used for patients with metastatic or unresectable solid tumors. After one year, it is approved by US Food and Drug Administration for those patients that suffer from recurrent cervical cancer. Later in 2019, Lenvatinib was approved by US Food and Drug Administration for advanced endometrial cancer [10, 14].
9.2. Nanoparticle-assisted drug delivery system
Whenever chemotherapeutic agents are used for cancer treatment, but there are several drawbacks. These drawbacks are the main reason for the failure to treat any cancer. Some of the flaws of chemotherapeutic agents include side effects, resistance, and toxicity. Resistance against chemotherapeutic agents occurs due to the wrong or miscalculated dosage of chemotherapeutic agents, whereas the failure of specific action leads to toxicity.
When one chemo drug is used for a long duration, then the risk of development of chemoresistance elevates. In order to prevent this, two chemo drugs are used, but they are only efficient and effective for small tumors. The advancement of science has given us many ways and methods by which the failure of chemotherapeutic drugs can be avoided. The emergence of the field of nanobiotechnology act as the savior.
Nanoparticle-assisted drug delivery systems are used to treat various cancers, including cervix uteri cancer. Multiple drugs loaded on nanoparticles serve as a better option. Zinc oxide ZnO nanoparticles bound with chemo drugs happen to have increased anticancer properties. These experiments were done in human cell lines, including human cervical adenocarcinoma (HeLa) [12].
10. During pregnancy cervical cancer management:
Management of those patients that are pregnant and are suffering from cervical cancer need more prudent management. The patient and her partner should have a thorough and detailed discussion. They should never be kept unaware of the plan. Overall, pregnant and non-pregnant patients with cervical cancer have the same management principles. Before the mid of the second trimester, treatment should be done continuously. The stage of disease determines the mode of treatment. If radiation therapy is used, then abortion of the fetus can happen [5].
11. Conclusion
Considering the reasons for its spread and its relation with HPV, one should be very cautious regarding the cervix uteri cancer. If someone gets diagnosed with this type of cancer, there should be no hesitation in going for treatment therapies. There is no hard and fast rule that this disease can affect young or older ages; thus, regular screening tests and preventive measures should be observed in every condition (especially in the countries where the risk is higher). Cervical cancer management is crucial for the patients; otherwise, it can lead to fatal conditions. Even after the successful treatment of cervix uteri cancer, patients should remain attached to the treatment centers to prevent post-treatment recurrence of the disease. This attitude can help communities survive this dangerous cancer type.
References
- Bhatla N, Aoki D, Sharma DN, et al. Cancer of the cervix uteri. International journal of gynecology & obstetrics 143 (2018): 22-36.
- Devesa SS, Young Jr JL, Brinton LA, et Recent trends in cervix uteri cancer. Cancer 64 (1989): 2184-2190.
- Wiebe E, Denny L, Thomas G. Cancer of the cervix uteri. International Journal of Gynecology & Obstetrics 119 (2012): S100-S109.
- Berek JS, Matsuo K, Grubbs BH, et al. Multidisciplinary perspectives on newly revised 2018 FIGO staging of cancer of the cervix uteri. Journal of gynecologic oncology 30 (2019).
- Bhatla N, Aoki D, Sharma DN, et al. Cancer of the cervix uteri: 2021 update. International Journal of Gynecology & Obstetrics 155 (2021): 28-44.
- Zhang S, Xu H, Zhang L, et al. Cervical cancer: Epidemiology, risk factors and screening. Chinese Journal of Cancer Research 32 (2020): 720.
- Kudva V, Prasad K, Guruvare S. Hybrid transfer learning for classification of uterine cervix images for cervical cancer screening. Journal of digital imaging 33 (2020): 619-631.
- Medhin LB, Tekle LA, Achila OO, et al. Incidence of cervical, ovarian and uterine cancer in eritrea: data from the national health laboratory, 2011-2017. Scientific Reports 10 (2020): 1-7.
- Haldorsen IS, Lura N, Blaakær J, et al. What is the role of imaging at primary diagnostic work-up in uterine cervical cancer?. Current oncology reports 21 (2019): 1-15.
- Dyer BA, Feng CH, Eskander R, et al. Current status of clinical trials for cervical and uterine cancer using immunotherapy combined with radiation. International Journal of Radiation Oncology* Biology* Physics 109 (2021): 396-412.
- Gadducci A, Guerrieri ME, Cosio S. Adenocarcinoma of the uterine cervix: pathologic features, treatment options, clinical outcome and prognostic variables. Critical reviews in oncology/hematology 135 (2019): 103-114.
- Pairoj S, Damrongsak P, Damrongsak B, et al. Antitumor activities of carboplatin–doxorubicin–ZnO complexes in different human cancer cell lines (breast, cervix uteri, colon, liver and oral) under UV exposition. Artificial Cells, Nanomedicine, and Biotechnology 49 (2021): 120-135.
- Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. The Lancet Global Health 8 (2020): e191-e203.
- Dyer BA, Feng CH, Eskander R, et al. Current status of clinical trials for cervical and uterine cancer using immunotherapy combined with radiation. International Journal of Radiation Oncology* Biology* Physics 109 (2021): 396-412.
- Charo LM, Plaxe SC. Recent advances in endometrial cancer: a review of key clinical trials from 2015 to 2019. F1000Research 8 (2019).
- Pecorelli S, Odicino F. Cervical cancer staging. The Cancer Journal 9 (2003): 390-394.
- Bourgioti C, Chatoupis K, Moulopoulos LA. Current imaging strategies for the evaluation of uterine cervical cancer. World journal of radiology 8 (2016): 342.
- Odicino F, Pecorelli S, Zigliani L, et al. History of the FIGO cancer staging system. International Journal of Gynecology & Obstetrics 101 (2008): 205-210.
- Matsuo K, Machida H, Mandelbaum RS, et al. Validation of the 2018 FIGO cervical cancer staging system. Gynecologic oncology 152 (2019): 87-93.
- Kitajima K, Murakami K, Kaji Y, et al. Established, emerging and future applications of FDG-PET/CT in the uterine cancer. Clinical radiology 66 (2011): 297-307.
- Castellsagué X. Natural history and epidemiology of HPV infection and cervical cancer. Gynecologic oncology 110 (2008): S4-S7.
- Petry KU. HPV and cervical cancer. Scandinavian Journal of Clinical and Laboratory Investigation 74 (2014): 59-62.
- Jalil AT, Karevskiy A. The cervical cancer (CC) epidemiology and human papillomavirus (HPV) in the middle east. International Journal of Environment, Engineering and Education 2 (2020): 7-12.
- Bhatla N, Aoki D, Sharma DN, et al. Cancer of the cervix uteri. International journal of gynecology & obstetrics 143 (2018): 22-36.