Cecal Volvulus a rare cause of Intestinal obstruction: Our experience and literature review
Article Information
Fiordaliso Michelea*, Ngjelina Jonela, De Marco Flavia Antoniab, Panaccio Paoloc, Farrah Ribhia, Ahmad Shadia, Karaorman Mevlüta, Kore Drinia
aDepartment of Surgery, Erbach General Hospital, Germany
bDepartment of Medicine, Friedrichshafen General Hospital, Germany
cDepartment of Surgery, Renzetti Hospital. Lanciano, Italy
*Corresponding author: Fiordaliso Michele, Department of Surgery, Erbach General Hospital, Germany
Received: 04 June 2021; Accepted: 15 June 2021; Published: 21 June 2021
Citation: Fiordaliso Michele, Ngjelina Jonel, De Marco Flavia Antonia, Paolo Panaccio, Farrah Ribhi, Shadi Ahmad, Mevlüt Karaorman, Kore Drini. Cecal Volvulus a rare cause of Intestinal obstruction: Our experience and literature review. Journal of Surgery and Research 4 (2021): 323-335.
View / Download Pdf Share at FacebookAbstract
Cecal volvulus represents 25-40% of all colonic volvulus. Symptoms include abdominal distension, constipation, nausea and vomiting where it may be intermittent. Abdominal X-rays and computed tomography (CT) may help with diagnosis and recommended treatment is resection of mobile caecum. Although rarely identified as a source of abdominal pain, cecal volvulus has clinical significance as it can lead to a number of serious complications including bowel obstruction, perforation and ischemia. We report here on our experience and also examine the relevant literature to differentiate cecal volvulus from other forms of bowel obstruction. General surgeons should be aware of this disease and consider it in the differential diagnosis of acute abdomen.
Keywords
Cecal volvulus, Colon volvulus, Cecopexy, Cecal necrosis, Bowel obstruction, Cecal ischemie
Cecal volvulus articles; Colon volvulus articles; Cecopexy articles; Cecal necrosis articles; Bowel obstruction articles; Cecal ischemie articles
Cecal volvulus articles Cecal volvulus Research articles Cecal volvulus review articles Cecal volvulus PubMed articles Cecal volvulus PubMed Central articles Cecal volvulus 2023 articles Cecal volvulus 2024 articles Cecal volvulus Scopus articles Cecal volvulus impact factor journals Cecal volvulus Scopus journals Cecal volvulus PubMed journals Cecal volvulus medical journals Cecal volvulus free journals Cecal volvulus best journals Cecal volvulus top journals Cecal volvulus free medical journals Cecal volvulus famous journals Cecal volvulus Google Scholar indexed journals Colon volvulus articles Colon volvulus Research articles Colon volvulus review articles Colon volvulus PubMed articles Colon volvulus PubMed Central articles Colon volvulus 2023 articles Colon volvulus 2024 articles Colon volvulus Scopus articles Colon volvulus impact factor journals Colon volvulus Scopus journals Colon volvulus PubMed journals Colon volvulus medical journals Colon volvulus free journals Colon volvulus best journals Colon volvulus top journals Colon volvulus free medical journals Colon volvulus famous journals Colon volvulus Google Scholar indexed journals Cecopexy articles Cecopexy Research articles Cecopexy review articles Cecopexy PubMed articles Cecopexy PubMed Central articles Cecopexy 2023 articles Cecopexy 2024 articles Cecopexy Scopus articles Cecopexy impact factor journals Cecopexy Scopus journals Cecopexy PubMed journals Cecopexy medical journals Cecopexy free journals Cecopexy best journals Cecopexy top journals Cecopexy free medical journals Cecopexy famous journals Cecopexy Google Scholar indexed journals Cecal necrosis articles Cecal necrosis Research articles Cecal necrosis review articles Cecal necrosis PubMed articles Cecal necrosis PubMed Central articles Cecal necrosis 2023 articles Cecal necrosis 2024 articles Cecal necrosis Scopus articles Cecal necrosis impact factor journals Cecal necrosis Scopus journals Cecal necrosis PubMed journals Cecal necrosis medical journals Cecal necrosis free journals Cecal necrosis best journals Cecal necrosis top journals Cecal necrosis free medical journals Cecal necrosis famous journals Cecal necrosis Google Scholar indexed journals Bowel obstruction articles Bowel obstruction Research articles Bowel obstruction review articles Bowel obstruction PubMed articles Bowel obstruction PubMed Central articles Bowel obstruction 2023 articles Bowel obstruction 2024 articles Bowel obstruction Scopus articles Bowel obstruction impact factor journals Bowel obstruction Scopus journals Bowel obstruction PubMed journals Bowel obstruction medical journals Bowel obstruction free journals Bowel obstruction best journals Bowel obstruction top journals Bowel obstruction free medical journals Bowel obstruction famous journals Bowel obstruction Google Scholar indexed journals Cecal ischemie articles Cecal ischemie Research articles Cecal ischemie review articles Cecal ischemie PubMed articles Cecal ischemie PubMed Central articles Cecal ischemie 2023 articles Cecal ischemie 2024 articles Cecal ischemie Scopus articles Cecal ischemie impact factor journals Cecal ischemie Scopus journals Cecal ischemie PubMed journals Cecal ischemie medical journals Cecal ischemie free journals Cecal ischemie best journals Cecal ischemie top journals Cecal ischemie free medical journals Cecal ischemie famous journals Cecal ischemie Google Scholar indexed journals colonoscopy articles colonoscopy Research articles colonoscopy review articles colonoscopy PubMed articles colonoscopy PubMed Central articles colonoscopy 2023 articles colonoscopy 2024 articles colonoscopy Scopus articles colonoscopy impact factor journals colonoscopy Scopus journals colonoscopy PubMed journals colonoscopy medical journals colonoscopy free journals colonoscopy best journals colonoscopy top journals colonoscopy free medical journals colonoscopy famous journals colonoscopy Google Scholar indexed journals barium enema articles barium enema Research articles barium enema review articles barium enema PubMed articles barium enema PubMed Central articles barium enema 2023 articles barium enema 2024 articles barium enema Scopus articles barium enema impact factor journals barium enema Scopus journals barium enema PubMed journals barium enema medical journals barium enema free journals barium enema best journals barium enema top journals barium enema free medical journals barium enema famous journals barium enema Google Scholar indexed journals
Article Details
1. Introduction
Volvulus of the cecum is an axial twist or a folding of the bowel upon its mesentery. Clinical signs of cecal volvulus are not specific.Abdominal CT scan, barium enema and colonoscopy have been shown to be superior to plain abdominal radiographs in establishing a diagnosis but they are still not specific enough for making a definitive diagnosis [1]. Surgery is often necessary for both definitive diagnosis and management.
Table 1: Patients with cecal volvulus.
3. Literature Review
The series comprises all 41 (Table 1) patients with cecal volvulus. There were 24 females and 17 males, the mean age of the female patients being 59 years (range 14-89 years) and that of the males 58 years (range 10-91 years). Five patients were excluded from Andersson's study where the cecum volvulus was found only at autopsy. In all patients there was a history of abdominal pain.
Twelve patients had previously been subjected to abdominal surgery (appendectomy or cholecystectomy). In a few patients there was a possible causal connexion and these case histories warrant special comment:
Case 3. A 61-year-old woman had surgery for a cecal volvulus 8 years before. Cecopexy had been performed with catgut as suture material. She was again admitted 8 years later with similar symptoms. Cecopexy was again performed but this time silk was used. Afterwards the patient was free from abdominal symptoms until her death from an unrelated cause 14 years later [2].
Case 4. A 19-year-old girl had been subjected to appendectomy 7 years previously. Delivering the appendix had been unusually difficult and the surgeon had been forced to mobilize part of the cecum. Volvulus of the colon developed 7 years later [2].
Case 33. A 71-year-old woman, a few hours after colonoscopy, complained of severe abdominal pain. After radiological examination the patient underwent subtotal colectomy due to a parasigmoidal abscess and cecal gangrene due to a volvulus [3].
We have little doubt that the aetiology of this patient's caecal volvulus was overinsufflation of air, which is sometimes inevitable when fluid has to be aspirated frequently to maintain a good view. Deflation during withdrawal of the instrument should always be performed but may not be complete in those cases in which only limited colonoscopy has been carried out.
Case 34. A 19-year-old woman, 26 weeks pregnant, underwent urgent right hemicolectomy due to a cecal volvulus and subsequent gangrene. Volvulus of the coecum is the second cause of colonic obstruction during pregnancy after sigmoid colon volvulus and its incidence in pregnancy is 1/2500–1/3500 [4]. The incidence of coecal volvulus increases with the duration of gestation and is greatest at times of rapid uterine size changes, especially from 16 to 20 weeks, when the uterus becomes an intra-abdominal organ; from 32 to 36 weeks, as the fetus enters the pelvis; and in the puerperium, when the uterine size changes rapidly again [11]. As pregnancy results in marked displacement of the coecum, which may predispose to relapse of the volvulus, resection is the best procedure to avoid recurrence [12,13].
Case 35. A 66-year-old patient suffering from chronic intestinal pseudoobstruction (CIPO) underwent urgent right hemicolectomy due to cecal volvulus [5]. There are no reports on the aetiology or incidence of colonic volvulus in adult patients with CIPO in the literature. Colonic (sigmoid) volvulus is reported briefly in an adult with familial visceral myopathy. In children there are only isolated case reports of colonic volvulus in combination with CIPO [14]. The same predisposing factors in adults are reported in children, namely a dilated and redundant colon, previous abdominal surgery and abnormal peritoneal/mesenteric fixation [15,16].
Case 40. Anamnesis of a 70-year-old woman recorded a ventral hernia after bariatric surgery due to obesity. She underwent urgent ileocolic resection and closure of the abdominal hernia due to cecal volvulus. Is possible that due to the long-standing herniation of the colon from the abdominal cavity, resulted in elongation of the mesentery combined and increased caecal mobility due to losing fixation points causing her to be at increased risk developing caecal volvulus [10].
There were two patients in whom the volvulus may have been related to a distal obstructing lesion. In one case such a lesion consisted of a rectal cancer and in another the lesion was cancer of the sigmoid colon. Last, we described 4 patient cases where cecal volvulus is ascribable to intestinal malrotation: in these patients, common mesentery was found.
3.1 Our experience
Case 41. A 63-year-old woman arrived in the emergency department with pain in her right iliac fossa , associated with nausea and a slight fever. The exam could only show definite tenderness on palpation in the right iliac fossa and positive Blumberg’s sign. In her medical history, she reported a laparoscopic appendectomy, underwent in our hospital. On her arrival, leukocytes were 15000 mm3 and C-reactive protein 50 mg/l. A radiological examination showed an intestinal obstruction, confirmed by a CT scan of the abdomen, where a cecal volvulus was described as a possible cause. The patient was admitted in our General Surgery Department, where she underwent to a laparotomy exposing cecal volvulus and subsequent necrosis of the intestinal walls (Figures 1,2). After the detorsion of the torsional colon , warm soaked laparotomy pads were applied to the affected colon, but the patient underwent right colectomy. Pathology result was reported as necrotic and hemorrhagic colon specimens due to ischemia or venous thrombosis.The restoration of intestinal continuity was completed with a hand sewn side-to-side ileocolic anastomosis, double-layered thread. During surgery, excessive motility of the caecum was noticed as the possible cause of volvulus. In the description of her previous appendectomy, it was underlined that the cecum was immobilized due to inflammatory adhesions. The patient was discharged ten days after surgery, with her gastrointestinal function completely recovered. Ultrasound scan showed no intra-abdominal collection.
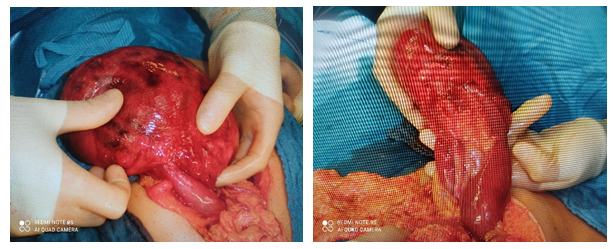
Figures 1,2: Caecumdilatation and necrosis in the surgical field during the explorativelaparotomy.
4. Discussion
Volvulus of the cecum is an axial twist or a folding of the bowel upon its mesentery. This results in acute intestinal obstruction which may or may not be complicated by occlusion of the mesenteric vessels. The condition was first described by Rokitansky [17] in 1837. Cecal volvulus is an infrequently encountered clinical condition and an uncommon cause of intestinal obstruction [18]. It is responsible for approximately 1-1.5% of all intestinal obstructions. Its incidence is 2.8-7.1 cases per million annually . Cugnenc et al. reported in a series an average age of occurrence of cecal volvulus at 61.8 years and there is no predisposition related to sex established [19]. Cecal volvulus occurs in case of inadequate right colon fixation or congenital abnormalities in which the right colon does not properly fuse with the lateral peritoneum [20]. Based on reports from necropsy reviews, sufficient cecal mobility for volvulus and bascule formation is found in 11% and 25% of adults, respectively [20]. In addition of cecal fixation abnormalities, the cecal volvulus can occurs secondary to adhesions from abdominal surgery, chronic constipation, pregnancy or prolonged immobility [21]. The cecal volvulus is observed during pregnancy with an incidence of 1/3000 (4), occasionally associated with giant uterine leiomyomas [22] . However, the large difference between incidence of mobile caecum and caecal volvulus suggests that factors other than anatomical susceptibility are at play [1] and additional conditions such as history of prior abdominal surgery [23], high fiber intake [24], adynamic ileus and chronic constipation [25] are known to predispose to the condition. Cecal volvulus represents the 34-50% of total colon volvolus cases [26,27]. Two rotation modalities are observed: the first one consists in a clockwise or anticlockwise rotation of the caecum, of the last looped ileum and the proximal ascending colon; the second type in the cranial and anterior direction of the bottom of the caecum. The first one can be defined “volvulus” in the strict sense of the word, being a volvulus by definition a rotation around a fixed point (Figure 3). The second case (Figure 4) is rather a tilting of the caecum [23,24]. In the first case, the intestinal obstruction is localized about the ileocecal valve; in the second rarer situation, about the colocecal connection. Whereas tilting of the caecum predisposes to diastasis of the caecum rather than necrosis, cecal volvulus may evolve into necrosis, as in any other case where an intestinal tract is affected by volvulus.
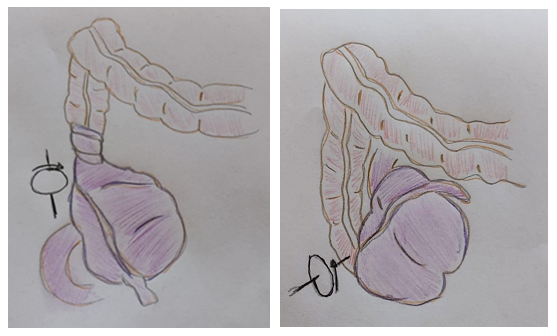
Figure 3: Axial cecal volvulus. Figure 4: Cecal bascule.
The patterns of clinical presentation are broadly categorised as recurrent intermittent, acute obstruction, and acute fulminant patterns [29]. The patients with Mobile caecum syndrome have a chronic intermittent abdominal pain with spontaneous resolution after the passage of flatus. Physical examination may show mild right sided abdominal tenderness or no abnormalities. This clinical presentation is generally not associated with bowel necrosis however may be an identifiable predecessor in 50% of patients presenting with acute volvulus [31-32]. The patients with Acute obstruction have cramping abdominal pain and vomiting that do not resolve spontaneously. The physical findings generally include tenderness of the abdomen, with or without a palpable abdominal mass, and high pitched bowel sounds. With recognition and timely treatment, this presentation is associated with comparatively low incidence of bowel necrosis. The patients with Acute fulminant volvulus generally have toxic appearance with abdominal tenderness associated with peritonitis. Patients with this presentation frequently have bowel necrosis. In cecal necrosis, the symptomatology may overlap with that of most appendicitis cases [32], making impossible a differential diagnosis based on clinical evidence. Fever, continuous pain in the right iliac fossa, muscular resistance to palpation, positive Blumberg’s sign, alteration of the digestive function such as nausea, vomiting and lack of appetite may be detected. The anamnestic data of pain which did not start from the epigastric area subsequently spreading to the right iliac fossa, as well as an elderly patient, should anyway lead to the suspicion that the disease might not be referable to appendicitis. A similar symptomatology may however be associated with diverticulitis of the caecum, acute inflammation at the ileo-ceco-colonic junction, cecum cancer, diverticulitis in a right displaced sigmoid colon, ileocecal intussusception [33], a perforated appendix diverticulum [34], epiploic appendagitis [35], right adnexitis, a perforated duodenal diverticulum. Laboratory analysis may show leukocytosis and increased C-reactive protein.There is an apparent increased propensity for acute caecal volvulus presentation during periods of concurrent acute medical illnesses, as 12%–28% of the reported patients with acute volvulus are already hospitalised for a variety of medical illnesses at the time of diagnosis. [23,36]. Barium enema is 88% accurate for volvulus and enables visualization of the distal colon to exclude contributory abnormalities [1]. It has occasional success in reduction of volvulus [23]. However, it is time consuming and has potential for contrast extravasation and thus is unsuitable for critically ill patients [29,37,38]. The ‘‘beak sign’’ or a smooth tapering cut off at the efferent limb of the obstruction is the most common confirmatory finding visualised during barium enema [39]. Computed tomography (CT) scan of the abdomen with contrast agent should be the first-choice diagnostics. The ‘‘coffee bean’’, ‘‘bird beak’’, and ‘‘whirl’’ signs are three of the common CT findings associated with acute caecal volvulus. [40] The ‘‘coffee bean’’ sign (Figure 5) generally refers to an axial view of a dilated caecum (Figure 5 filled with air and fluid that may be visualised anywhere within the abdominal cavity. The ‘‘bird beaks’’ are images (Figure 6) correlating with the progressively tapering efferent and afferent bowel loops terminating at the site of torsion. The ‘‘whirl sign’’ is a description applied to the CT image of a soft tissue mass with internal architecture containing swirling strands of soft tissue and fat attenuation. The presence of intramural bowel gas (pneumatosis intestinalis), the absence of opacification of the ileocolic artery or its branches and the thickening of the cecal wall [41,42], are signs of ischemic of the caecum. These findings may be absent, whereas pericecal effusion is always present. In absence of perforation, it may be rather scarce. The appendix is often found in normal conditions and regularly vascularized. Thickening of the last iliac fossa and edema of the pericecal tissue, on the other hand, are frequent findings. In absence of parietal alterations and vascular anomalies, CT may not lead to identify caecum infarction with certainty, but can anyway point out that surgery would be advisable, by showing the presence of a serious disease affecting the ileocolic-ceco tract. At present, there is no specific serum marker for colonic ischemia. Diagnostic US has been reported to be helpful in such cases [43].
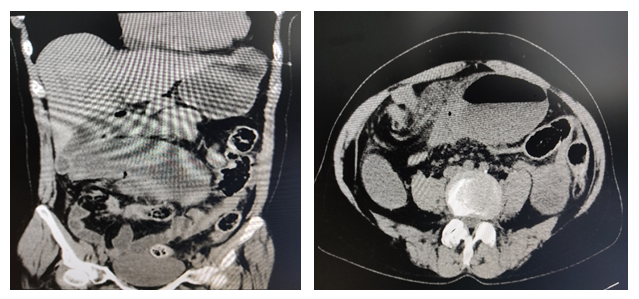
Figure 5 (left): Cecal volvulus located in the left upper quadrant. Topogram reveals markedly air-distended cecum in shape of coffee bean.
Figure 6(right): Axial CT scan shows cecal volvulus in 63-year-old woman. “Whirl sign” (red arrow) is composed of spiraled loops of distal ileum and enhancing engorged vessels with decompressed descending colon (white arrow).
Flexible sigmoidoscopy is commonly performed for the confirmation and initial management of sigmoid volvulus, however the utility of endoscopic therapy in acute caecal volvulus diagnosis and treatment is generally considered limited, as the success rate of colonoscopic reduction of caecal volvulus has been about 30% [44,45].
Only urgent surgical care is decisive in order to avoid further evolution into perforation, widespread peritonitis and septic shock. Among the surgical options, we have:
- right hemicolectomy [32] or caecum resection, followed by ileocolic anastomosis,
- operative detorsion Manual reduction of volvulus by caeliotomy (mortality 0%-25%; recurrence 0%-70%).
- caecopexy Fixation of right colon by suturing of caecum and/or ascending colon to lateral parietal peritoneum (operative mortality 0%-30%; recurrence 0%-40%) [1].
A terminal ileostomy and suturing the colonic abutment or performing ileostomy and colostomy subsequently, are preferable to avoid anastomosis in case of widespread intestinal ischemia [46].
In case of isolated infarction of the caecum, it was occasionally reported the removal of the necrotic tissue, followed breach suture [47], or percutaneous cecostomy tube placement. Resection of the necrotic area followed by breach suture- rather than a complete resection of the caecum - could be a simpler solution, in particular in presence of parcellar necrosis; nevertheless, this option should only be adopted after careful consideration of the most probable cause of necrosis and a scrupulous tomographic examination of cecal vascularization. In fact, it must be considered that in the case of important compromise of cecal arteries, the pathological process affecting part of the caecum could later spread to adjacent tissues, resulting in fistulization and peritonitis. In this case, the “insistent” caecum preservation would be unreasonable, as its resection would not cause any clinically relevant functional alterations. Cecostomy by means of a Petzer catheter should not be considered, given the possibility of parietal and pericecal infection, as well as protracted discomfort for the patient and the lack of advantages over direct suture [23,48]. In addition to that, given the frequent obstruction of the catheter, its benefits in terms of intraluminal decompression are merely theoretical. In our review, detorsion without fixation of the cecum was performed in 13 patients. Detorsion with ensuing cecopexy was done in 14 patients. In the majority of these patients lateral wall cecopexy was carried out. Cecopexy with cecostomy was done in 3 patients. Finally right hemicolectomy with end to end ileotransverse colostomy was performed in 11 patients.
5. Conclusion
Cecal volvulus is the second most common large bowel volvulus after sigmoid colon. It is postulated that caecal volvulus occurs in individuals who have an inherently mobile caecum due to poor embryological attachment of the caecum and ascending colon to the posterior parietal peritoneum in the right paracolic gutter, in combination with risk factors such as chronic constipation, bowel adhesions or recent abdominal surgery. The clinical findings and laboratory abnormalities associated with caecal volvulus are predominantly determined by the pattern, severity, and duration of the intestinal obstruction. Abdominal X-ray and abdominal CT scan are the essential radiological procedures in the diagnosis of volvulus of the cecum . The only effective treatment for cecal volvulus is surgical intervention. In our opinion, the most appropriate operative strategy for a given patient can be determined only by the operating surgeon after taking into consideration the surgical expertise, patient’s physiological status, viability of the involved intestines, the potential perioperative morbidity and mortality, and the risk of volvulus recurrence.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Sources of funding
No source of funding or sponsors.
Ethical approval
Approval from the ethical committee was not required for this study.
Human and animal rights
The study including human participants has been performed in accordance with the ethical standards of the Declaration of Helsinki and its later amendments.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in- Chief of this journal on request.
Authors contribution
Fiordaliso Michele, Ngjelina Jonel: Study design, data collection,writing.
Kore Drini, Shadi Ahmad: Surgeons, who performed the operation
De Marco Antonia Flavia, Paolo Panaccio, Farrah Ribhi: Data collection.
Kore Drini, Mevlüt Karaorman: Data collection, writing.
All authors have approved the final article.
Registration of research studies
N/A.
Guarantor
Michele Fiordaliso
References
- Consorti ET, Liu TH. Diagnosis and treatment of caecal volvulus. Postgrad Med J 81 (2005): 772- 776.
- Andersson, Bergahl L, Van Der Linden W. Volvulus of the Cecum Ann Surg 181 (1975): 6
- Anderson JR, Spence RA, Wilson BG. Gangrenous caecal volvulus after colonoscopy. Br Med J 286 (1983): 439-440.
- Youssef N, Khalid R, Sanaa L, et al. Coecal volvulus: An acute complication of pregnancy J Emerg Trauma Shock 3 (2010): 426-427.
- Tatterton M, El-Khatib C. Caecal volvulus in a patient with chronic intestinal pseudo-obstruction Ann R Coll Surg Engl 93 (2011): e131-e132.
- Clifford M, Johnstone M, Powell K, Phillip M. Caecal volvulus in an adolescent African male: a case report and brief review of the literature Pan Afr Med J 6 (2014): 17-92.
- Simon AZ, Alex H, Hasan M, et al. Caecal volvulus following abdominoplasty: a tale of caution BMJ Case Rep 23 (2014).
- Abdoul A, Houssam B, Tarek S, et al. Acute cecal volvulus: A diagnostic and therapeutic challenge in emergency: A case report Annals of Medicine and Surgery 48 (2019): 69-72.
- Mohammad Y, Mohammed K, Alfredo T, et al. Caecal volvulus following left-side laparoscopic retroperitoneal nephroureterectomy BMJ Case Rep 12 (2019): e228878.
- Ying Y, Anthony F, Markus T. Caecal volvulus in an incisional hernia. Journal of Surgical Case Reports 10 (2020): 1-3.
- Perdee PW, Johnson HW, Stafford PW. Intestinal obstruction complicating pregnancy. Am J Surg 164 (1992): 384-388.
- Harer WB, Harer WE. Volvulus complicating pregnancy and puerperium. Obstet Gynecol 12 (1958): 367-376.
- Lal SS, Kadian S, Goyal A, et al. Cecal volvulus in pregnancy. Is delay in diagnosis avoidable. Asian J Surg 28 (2005): 52-54.
- Jones SC, Dixon MF, Lintott DJ, et al. Familial visceral myopathy. A family with involvement of four generations. Dig Dis Sci 37 (1992): 464-469.
- Osuka A, Ikegami R, Watanabe Y. Splenic flexure volvulus in a child with chronic idiopathic pseudo-obstruction syndrome. Pediatr Surg Int 22 (2006): 833-835.
- Altaf MA, Werlin SL, Sato TT et al. Colonic Volvulus in Children With Intestinal Motility Disorders. J Pediatr Gastroenterol Nutr 49 (2009): 59-62.
- Rokitansky C. Intestinal Strangulation. Arch Gen Med 14 (2002): 18-37.
- Habre J, Sautot-Vial N, Marcotte C, et al. Caecal volvulus. Am J Surg 196 (2008): 48-49.
- Cugnenc PH, Gayral F, Larrieu H, et al. Volvulus aigu du cæcum: à propos de 10 observations. Chirurgie 108 (1982): 279-283.
- Wolfer JA, Beaton LE, Anson BJ. Volvulus of the cecum. Anatomical factors in its etiology. Surg Gynecol Obstet 9 (1942): 882-894.
- Howard DG, Catto J. Cecal volvulus. A case for nonresectional therapy. Arch Surg 115 (1980): 273-277.
- De Vries HS, Samial RK, Maresch BJ et al. Cecal volvulus caused by a large uterine leiomyoma. Int J Surg Case Rep 10 (2015): 97-99.
- O'Mara CS, Wilson THJSGL, Stonesifer GL, et al. Cecal volvulus: analysis of 50 patients with long-term follow-up. Ann Surg 189 (1979): 724-31.
- Pulvirenti E, Palmieri L, Toro A, et al. Is laparotomy the unavoidable step to diagnose caecal volvulus? Ann R Coll Surg Engl 92 (2010): 27-29.
- Radin DR, Halls JM. Cecal volvulus: a complication of colonoscopy. Gastrointest Radiol 11 (1986): 110- 111.
- Ballantyne GH, Brandner MD, Beart RW Jr e al. Volvulus of the colon. Incidence and mortality. Ann Surg 202 (1985): 83-92.
- Gilbert RF. Cecal infarction secondary to a distal obstructing fecaloma: association with drug abuse. South Med J 73(1980): 1296-1297.
- Tirol FT. Cecocolic torsion: classification, pathogenesis, and treatment.JSLS 9 (2005): 328-334.
- Friedman JD, Odland MD, Bubrick MP. Experience with colonic volvulus. Dis Colon Rectum 32 (1989): 409-416.
- Rogers RL, Harford FJ. Mobile cecum syndrome. Dis Colon Rectum 27 (1984): 399-402.
- Printen KJ. Mobile cecal syndrome in the adult. Am Surg 42 (1976): 204-205.
- Dirican A, Unai B, Bassulu N et al. Isolated cecal necrosis mimicking acute appendicitis: a case series. J Med Case Rep 3 (2009): 7443.
- Panaccio P, Fiordaliso M, Testa D, et al. Minimally Invasive Treatment of Sporadic Burkitt's Lymphoma Causing Ileocaecal Invagination. Case Rep Surg 30 (2018).
- Fiordaliso M, De Marco AF, Costantini R. A case of Type 2 appendiceal diverticulum perforated and a review of the literature. Int J Surg Case Rep 77 (2020): 450-453.
- Fiordaliso M, Ngjelina J, Flavia FA, et al. Torsion of Appendices Epiploicae (Appendagitis) Presenting as Appendicitis: Laparoscopic Diagnosis and Therapy. Indian Journal of Surgery 40 (2021): 12262.
- Theuer C, Cheadle WG. Volvulus of the colon. Am Surg 57 (1991): 145-150.
- Madiba TE, Thomson SR. The management of cecal volvulus. Dis Colon Rectum 45 (2002): 264-267.
- Rabinovici R, Simansky DA, Kaplan O, et al. Cecal volvulus. Dis Colon Rectum 33 (1990): 765-769.
- Young WS. Further radiological observations in caecal volvulus. Clin Radiol 31 (1980): 479-483.
- Moore CJ, Corl FM, Fishman EK. CT of cecal volvulus: unravelinf the image. AJR 177 (2001): 95-98.
- Hoeffel C, Crema HD, Belkacem A et al. Muti-detector row CT: spectrum of diseases involving the ileocecal area. Radiographics 26 (2006): 1373-1390.
- Simon AM, Birnbaum BA, Jacobs JE. Isolated infarction of the cecum: CT findings in two patients. Radiology 214 (2000): 513-516.
- Ranschaert E, Verhille R, Marchal G, et al. Sonographic diagnosis of ischemic colitis. J Belg Radiol. 77 (1994): 166-168.
- Ballantyne GH, Brandner MD, Beart RW Jr, et al. Volvulus of the colon. Incidence and mortality. Ann Surg 202 (1985): 83-92.
- Anderson MJ, Okike N, Spencer RJ. The colonoscope in cecal volvulus: report of three cases. Dis Colon Rectum 21 (1978): 71-74.
- Milev OG, Milanov LL. Isolated cecal necrosis mimicking a perforated peptic ulcer: a case report. Am J Med Case Rep 4 (2016): 349-353.
- Kafadar MT, Bardakçi O, Çetinkaya I. Isolated partial cecal necrosis as a differential diagnosis of right lower quadrant pain: a common presentation with an un common diagnosis. J Emerg Med Case Rep 2018; 9: 38-40.
- Weiss BD. Cecal volvulus: a diagnostic and therapeutic challenge. Postgrad Med 72 (1982): 189-194.
