Cauda Equina Syndrome During Labour - A Diagnostic Challenge and Proposed Management Algorithm
Article Information
Nicholas B Jones BSc, MBChB1*, Jonathon Richards MBChB, FRACS1, Christopher Hoffman MBChB, FRACS1, Shay Mandler MD, Cert Spec1
1All Department of Orthopaedics -Wellington Regional Hospital, Wellington, New Zealand.
*Corresponding Author: Nicholas Jones, Orthopaedic Clinic, Wellington Regional Hospital, 39 Riddiford St, Newtown Wellington 6021, New Zealand.
Received: 29 February 2024; Accepted: 11 March 2024; Published: 19 March 2024
Citation: Nicholas B Jones BSc(Hons), MBChB; Jonathon Richards MBChB, FRACS (Ortho); Christopher Hoffman MBChB, FRACS (Ortho); Shay Mandler MD, Cert Spec (Orth). Cauda Equina Syndrome During Labour - A Diagnostic Challenge and Proposed Management Algorithm. Journal of Spine Research and Surgery. 6 (2024): 26-30.
View / Download Pdf Share at FacebookAbstract
Aim:
The incidence of lumbar disc herniation during pregnancy is rare (1:10,000). Of all lumbar disc herniation’s, only 2% will develop acute Cauda Equina Syndrome (CES). It is a diagnostic challenge to identify CES during labour due to overlapping symptoms that mimic and obscure CES symptoms in a stressful therapeutic environment. We present a case report and brief literature review with a proposed algorithm for management.
Method:
We reviewed the case of a nulliparous 35 year old woman who developed CES during labour due to an acute extruded disc. CES symptoms developed during labour and were initially attributed to the obstetric process. Baby was delivered via emergency caesarean section for prolonged labour and foetal distress. Post delivery persistent saddle paresthesia, urinary retention and radicular leg pain prompted orthopaedic review. An MRI was performed demonstrating a large disc extrusion at the level of L5/S1.
Results:
Emergent decompression was performed post partum day 7. Improving pain and neurologic deficits were seen initially but some ongoing perineal parathesia and urinary frequency.
Conclusion:
Maintaining a high index of suspicion for persistent saddle anaesthesia, urinary retention and radicular pain post partum would aide in early referral for Orthopaedic review and advanced imagining in CES. The hope is this will help prevent persistent neurological deficits in young women and case reporting will aide in understanding what role if any CES has in prolonged labour.
Keywords
Cauda Equina Syndrome; Labour; Diagnostic Challenge; lumbar disc herniation
Article Details
Introduction
Lumbar disc herniation during pregnancy is uncommon with a prevalence of 1 in 10,000 cases. [1] Of those presenting with lumbar disc herniation only 2% will develop cauda equina syndrome (CES). [2] Cauda equina syndrome secondary to lumbar disc herniation during labour is even more uncommon. [3] Cauda equina syndrome is a clinical diagnosis supported by examination and imaging with common symptoms including low back pain, unilateral or bilateral radicular pain, lower limb weakness, saddle paresthesia and bowel and/or bladder dysfunction. [2] Delayed diagnosis and decompression is associated with an increased risk of permanent dysfunction and morbidity such as bowel and/or bladder dysfunction, motor and/or sensory disturbances. [4,5]
Pregnancy, and especially labour, shares symptoms that are consistent with CES such as bowel and/or bladder dysfunction, saddle anaesthesia and low back pain. [6,7] This makes CES a diagnostic dilemma for which the obstetric and anaesthetic team should maintain a high index of suspicion, especially if the symptoms are progressive in nature.
To our knowledge there is only one other case of CES during labour published. [3] We present this case report and suggest an initial management algorithm in the hope that further cases will be reported and the algorithm adapted accordingly.
Case Presentation
A 35 year old woman (gravidity 1, parity 0) was referred to the Orthopaedic service with persistent perineal and perianal numbness, faecal urgency and a single episode of urinary incontinence post partum day 6.
The patient was initially seen in the obstetric clinic at 39+5 weeks gestation with coccyx pain in keeping with term pregnancy and two episodes of reduced foetal movements. She was admitted under obstetrics for observation and induction of labour due a faintly positive kleihaur test. Approximately 13 hours into induction the patient reported the need to pass urine but was unable to void. Approximately 2 hours later she reported severe abdominal pain and an in and out urinary catheter was placed with 1200mls of urine drained and instant relief. An epidural anaesthetic was later sited and indwelling urinary catheter placed at that point. Labour did not progress and the patient delivered by emergency low caesarean section for prolonged foetal decelerations on cardiotocography and raised foetal lactate. She was discharged post partum day 3 with some ongoing saddle anaesthesia but was continent of bowel and bladder.
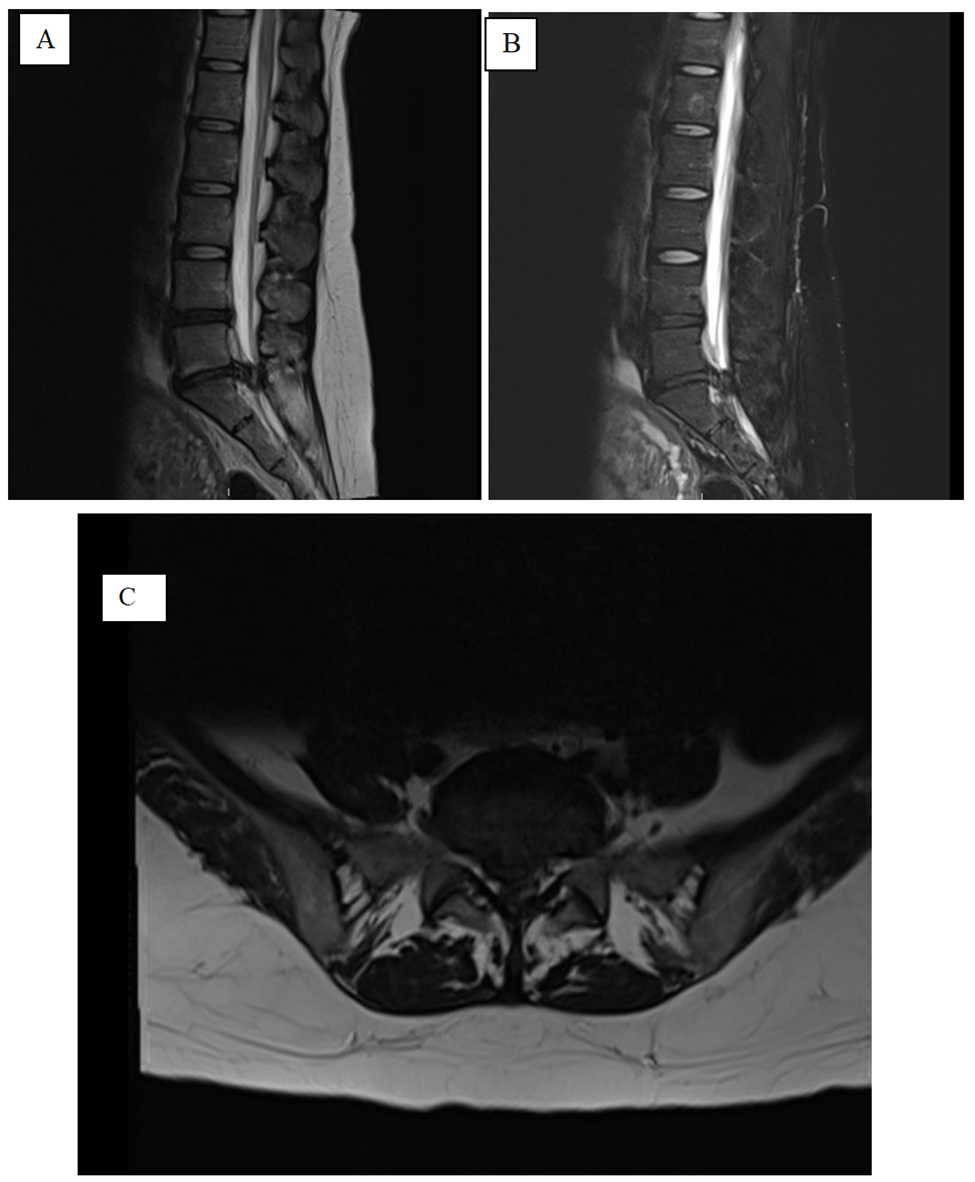
She represented to the obstetric clinic post partum day 6 with persistent perineal and perianal altered sensation, faecal urgency but no incontinence, and urinary frequency with one time incontinence and a sense of incomplete emptying. She had perineal and buttock pain in keeping with trial of vaginal delivery but new radicular leg pain when mobilising. The orthopaedic service was consulted and she was noted to be in urinary retention with a post void bladder scan of 300 milliliters. On examination she had normal resting anal tone but reduced contraction strength, altered bilateral perianal sensation, altered left L3 and L4 dermatomal sensation but ASIA grade 5 power and normal reflexes and tone bilaterally in the lower limbs. She proceeded to have an urgent MRI which demonstrated a large central disc protrusion at L5-S1 causing bunching of the cauda equina and she underwent L5-1 decompression and discectomy acutely.
Following laminectomy there was resolution of radicular leg pain, improving perineal and perianal altered sensation, and improving bladder function. At last clinic review 6 months post-surgery, saddle anaesthesia was improved but on going, no radicular leg pain, some urinary frequency but no retention or incontinence and she was going to work on this with the pelvic floor physiotherapy team via the obstetric department.
Discussion
Back pain is a common complaint during pregnancy due to the shift in the centre of gravity anteriorly as abdominal girth in the sagittal plane increases. [6,8] This results in further lumbar lordosis and anterior pelvic tilt, increasing the axial load of the lumbar spine and expelling water from the disc causing further column compression. [6] The diagnosis of lumbar disc herniation, of which back pain is a common complaint, is made in 1:10 000 pregnancies. [1,8] Less than 2% of lumbar disc herniation go on to develop CES. [2] Back pain during labour is also very common and it in isolation is not very specific to CES. [2,6] Known risk factors for disc herniation include high body mass index and increasing age both of which are increasing amongst the obstetric population. [2,8,9,10] It is likely the incidence of lumbar disc herniation in the obstetric population will increase and therefore CES during pregnancy and labour. Despite this, there is only one documented case of CES developing during labour itself prior to our case and a high index of suspicion for CES will be vital in appropriate diagnosis and management. [3]
Cauda equina syndrome is a clinical diagnosis supported by advanced imaging. [2] The key features include low back pain, unilateral or bilateral radicular pain, lower limb weakness, saddle anaesthesia and bowel and/or bladder dysfunction. [2] Cauda equina syndrome in those with lumbar disc herniation is the result of spinal stenosis secondary to the disc herniation and compression of the nerve roots distal to the conus medullaris [1,2] The time to decompression of the nerve root is thought to be directly related to the degree of ongoing morbidity. [5] Urinary symptoms in CES can be further subcategorized into two clinical syndromes:
- CES with retention, characterized by painless urinary retention with overflow incontinence
- CES with maintenance of some sphincter control despite altered sensation of the need to void and therefore loss of urge, and/or poor urinary stream. [2]
Our patient maintained sphincter control during labour but had altered sensation resulting in the inability to sense bladder distension and void prior to the in and out urinary catheter placed. She then had deterioration of this with incomplete emptying and overflow incontinence with elevated post void bladder scans. It was only once the bladder was severely dilated that she had the sensation of abdominal pain rather than the urge to void. In addition to urinary symptoms, faecal incontinence because of CES are common complaints secondary to reduced perianal sensation, reduced resting anal tone, and reduced voluntary anal contraction. [2] Faecal incontinence during labour and postpartum is not uncommon and like the other symptoms of CES must not be considered in isolation. [11] Our patient presented with faecal urgency rather than frank incontinence which is in keeping with CES with maintenance of some sphincteric control.
Furthermore, findings of lower limb reduced sensation, reduced motor power and reduced reflexes distal to the level of compression are common. [2] Whilst pregnancy and labour can be associated back pain and abnormal neurology post partum the incidence is thought low at ~1%. [12] Amongst post partum neurologic deficits, compressive or traction neuropathies affecting the lateral femoral cutaneous nerve is most common. [13] When there is enough clinical suspicion in the absence of definitive diagnosis an MRI scan is the imaging modality of choice. [2] This will help guide the degree of compression, level of compression and assist with preoperative planning for decompression. [2] Our patient demonstrated some altered sensation in the left L3 and L4 dermatomes that did not match our MRI findings with no discernable motor weakness or altered reflexes.
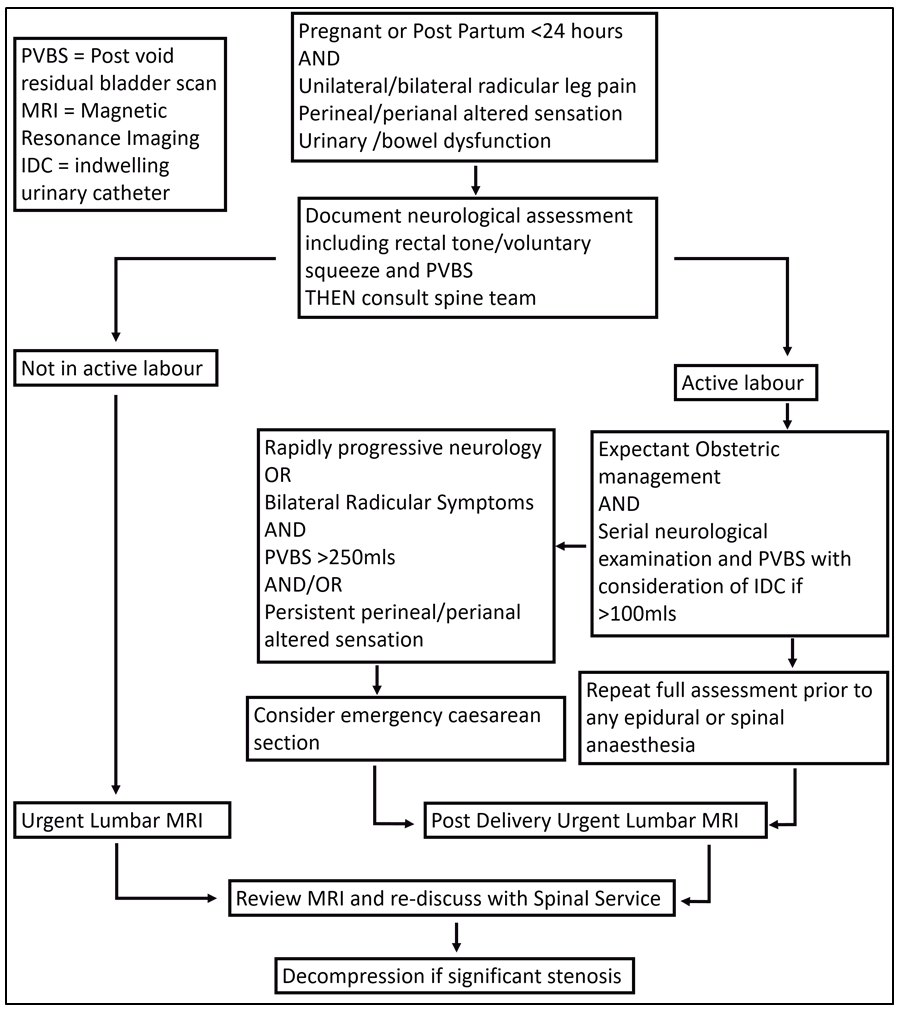
As was the case for our patient, persistent altered perineal and perianal sensation, radicular pain, and altered sphincteric function remain the best way of detecting CES. [2] The obstetric and anaesthetic teams appropriately counselled the patient on reporting ongoing or worsening symptoms and she presented for review, orthopaedic assessment and management. MRI is not contraindicated in pregnancy but during labour the reality of achieving a clinically useful scan is unlikely. [14] Therefore, MRI scan during labour would almost never be achievable. If there is enough suspicion of CES during labour then decisions need to be made about the mode of delivery and speed with which to correlate with MRI scan and subsequent surgical intervention.
The case and discussion highlight how difficult it is to discern the symptoms of acute lumbar disc herniation and CES from those common during active labour. The rising use of epidural anaesthesia further clouds the sensitivity of clinical assessment and between this and the rising morbidity of obstetric patients the index of suspicion must be raised amongst obstetric, anaesthetic, and spinal services. To this end we propose an initial algorithm to guide assessment and investigation accepting the obvious limitation of very few reported cases in the hope that further case reports or series may allow this to be adapted.
We have described the case of cauda equina syndrome during labour and the subsequent management under an orthopaedic spinal service. We have highlighted the difficulty in discerning the symptoms of active labour from those of CES. A high index of suspicion and prompt spinal service consultation enables best practice care with pregnant or post-partum patients with radicular leg pain, altered perineal/perianal sensation and urinary or bowel sphincteric dysfunction. We propose an algorithm to guide obstetric and spinal teams on dealing with high-risk patients to enable this and encourage further case reporting to help adapt this algorithm moving forward.
Declarations
I (We) accept full responsibility for the conduct of the study, had access to the data, and controlled the decision to publish.
Funding
No sources of funding required.
Conflict of interest
No conflict of interests.
References
- LaBan MM, Perrin JCS, Latimer FR. Pregnancy and the herniated lumbar disc. Arch Phys Med Rehabil 64 (1983).
- Gitelman A, Hishmeh S, Morelli BN, et al. Cauda equina syndrome: a comprehensive review. Vol. 37, American journal of orthopedics (Belle Mead, N.J.) (2008).
- Jones CS, Patel S, Griffiths-Jones W, et al. Presentation of cauda equina syndrome during labour. BMJ Case Rep (2015).
- Ahn UM, Ahn NU, Buchowski JM, et al. Cauda equina syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes. Spine (Phila Pa 1976), 25 (2000).
- Hogan WB, Kuris EO, Durand WM, et al. Timing of Surgical Decompression for Cauda Equina Syndrome. World Neurosurg 132 (2019).
- Bhardwaj A, Nagandla K. Musculoskeletal symptoms and orthopaedic complications in pregnancy: Pathophysiology, diagnostic approaches and modern management. Vol. 90, Postgraduate Medical Journal. (2014).
- Timothy J, Anthony R, Tyagi A, et al. A case of delayed diagnosis of the cauda equina syndrome in pregnancy. Australian and New Zealand Journal of Obstetrics and Gynaecology 39 (1999).
- Whiles E, Shafafy R, Valsamis EM, et al. The Management of Symptomatic Lumbar Disc Herniation in Pregnancy: A Systematic Review. Vol. 10, Global Spine Journal. (2020).
- Edwards P, Wright G. Obesity in pregnancy. Vol. 30, Obstetrics, Gynaecology and Reproductive Medicine. (2020).
- Curtin P, Rice J. Cauda equina syndrome in early pregnancy: A case report. Acta Obstet Gynecol Scand 86 (2007).
- Fathallah N, Spindler L, Zeitoun JD, et al. Anal incontinence after childbirth. Colon and Rectum 12 (2018).
- Wong CA, Scavone BM, Dugan S, et al. Incidence of postpartum lumbosacral spine and lower extremity nerve injuries. Obstetrics and Gynecology 101 (2003).
- O’Neal MA, Chang LY, Salajegheh MK. Postpartum spinal cord, root, plexus and peripheral nerve injuries involving the lower extremities: A practical approach. Vol. 120, Anesthesia and Analgesia. (2015).
- Patenaude Y, Pugash D, Lim K, et al. The Use of Magnetic Resonance Imaging in the Obstetric Patient. Journal of Obstetrics and Gynaecology Canada 36 (2014).