Cardiac Magnetic Resonance in times of COVID-19: A Disease with Many Cardiac Faces
Article Information
Leydimar Anmad Shihadeh MD1#, Maria Jose Romero-Castro MD1#, Andrea Moreno-Arciniegas MD1,5, Ana Pastor MD5, Beatriz Fuertes MD5, Blanca Zorita MD5, Daniel Prieto5, Maximiliano German Amado-Escañuela MD1, Belén Díaz MD1,2,5, Jose María Castellano MD PhD2,3,5, Leticia Fernández-Friera MD, PhD1,2,3,4,5
1Cardiac Imaging Unit, Hospital Universitario HM Montepríncipe-CIEC, Madrid, Spain
2Universidad CEU San Pablo, Madrid, Spain
3Centro Nacional de Investigaciones Cardiovasculares Carlos III (CNIC), Madrid, Spain
4CIBER de enfermedades CardioVasculares (CIBERCV), Madrid, Spain
5Cardiology Department, HM Hospitales-Centro Integral de Enfermedades Cardiovasculares (HM CIEC), Madrid, Spain
*Corresponding Author: Leticia Fernández-Friera, Director, Advanced Cardiac Imaging Unit, Cardiology Department, HM Hospitales. Avenida de Montepríncipe 25, 28660, Boadilla del Monte, Madrid. Centro Nacional de Investigaciones Cardiovasculares Carlos III (CNIC). Melchor Fernández Almagro 3, 28029 Madrid, España
Received: 22 November 2020; Accepted: 29 December 2020; Published: 13 January 2021
Citation:
Leydimar Anmad Shihadeh, Maria Jose Romero-Castro, Andrea Moreno-Arciniegas, Ana Pastor, Beatriz Fuertes, Blanca Zorita, Daniel Prieto, Belén Díaz, Jose María Castellano, Leticia Fernández-Friera. Cardiac Magnetic Resonance in times of COVID-19: A Disease with Many Cardiac Faces. Archives of Clinical and Medical Case Reports 5 (2021): 75-83.
View / Download Pdf Share at FacebookAbstract
Although cardiac magnetic resonance (CMR) may proof useful in the diagnosis of myocardial injury triggered by COVID-19, limited experience has yet been published. We report several cases presenting its utility at various COVID-19 disease stages in diagnosing different cardiac manifestations. The current COVID-19 crisis will undoubtedly transform CMR imaging Units.
Keywords
Covid-19; Cardiac magnetic resonance; Cardiomyopathy; Imaging
Covid-19 articles; Cardiac magnetic resonance articles; Cardiomyopathy articles; Imaging articles
Covid-19 articles Covid-19 Research articles Covid-19 review articles Covid-19 PubMed articles Covid-19 PubMed Central articles Covid-19 2023 articles Covid-19 2024 articles Covid-19 Scopus articles Covid-19 impact factor journals Covid-19 Scopus journals Covid-19 PubMed journals Covid-19 medical journals Covid-19 free journals Covid-19 best journals Covid-19 top journals Covid-19 free medical journals Covid-19 famous journals Covid-19 Google Scholar indexed journals Cardiac magnetic resonance articles Cardiac magnetic resonance Research articles Cardiac magnetic resonance review articles Cardiac magnetic resonance PubMed articles Cardiac magnetic resonance PubMed Central articles Cardiac magnetic resonance 2023 articles Cardiac magnetic resonance 2024 articles Cardiac magnetic resonance Scopus articles Cardiac magnetic resonance impact factor journals Cardiac magnetic resonance Scopus journals Cardiac magnetic resonance PubMed journals Cardiac magnetic resonance medical journals Cardiac magnetic resonance free journals Cardiac magnetic resonance best journals Cardiac magnetic resonance top journals Cardiac magnetic resonance free medical journals Cardiac magnetic resonance famous journals Cardiac magnetic resonance Google Scholar indexed journals Cardiomyopathy articles Cardiomyopathy Research articles Cardiomyopathy review articles Cardiomyopathy PubMed articles Cardiomyopathy PubMed Central articles Cardiomyopathy 2023 articles Cardiomyopathy 2024 articles Cardiomyopathy Scopus articles Cardiomyopathy impact factor journals Cardiomyopathy Scopus journals Cardiomyopathy PubMed journals Cardiomyopathy medical journals Cardiomyopathy free journals Cardiomyopathy best journals Cardiomyopathy top journals Cardiomyopathy free medical journals Cardiomyopathy famous journals Cardiomyopathy Google Scholar indexed journals PTA articles PTA Research articles PTA review articles PTA PubMed articles PTA PubMed Central articles PTA 2023 articles PTA 2024 articles PTA Scopus articles PTA impact factor journals PTA Scopus journals PTA PubMed journals PTA medical journals PTA free journals PTA best journals PTA top journals PTA free medical journals PTA famous journals PTA Google Scholar indexed journals imaging articles imaging Research articles imaging review articles imaging PubMed articles imaging PubMed Central articles imaging 2023 articles imaging 2024 articles imaging Scopus articles imaging impact factor journals imaging Scopus journals imaging PubMed journals imaging medical journals imaging free journals imaging best journals imaging top journals imaging free medical journals imaging famous journals imaging Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Sclerosis articles Sclerosis Research articles Sclerosis review articles Sclerosis PubMed articles Sclerosis PubMed Central articles Sclerosis 2023 articles Sclerosis 2024 articles Sclerosis Scopus articles Sclerosis impact factor journals Sclerosis Scopus journals Sclerosis PubMed journals Sclerosis medical journals Sclerosis free journals Sclerosis best journals Sclerosis top journals Sclerosis free medical journals Sclerosis famous journals Sclerosis Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals SARS-COV-2 articles SARS-COV-2 Research articles SARS-COV-2 review articles SARS-COV-2 PubMed articles SARS-COV-2 PubMed Central articles SARS-COV-2 2023 articles SARS-COV-2 2024 articles SARS-COV-2 Scopus articles SARS-COV-2 impact factor journals SARS-COV-2 Scopus journals SARS-COV-2 PubMed journals SARS-COV-2 medical journals SARS-COV-2 free journals SARS-COV-2 best journals SARS-COV-2 top journals SARS-COV-2 free medical journals SARS-COV-2 famous journals SARS-COV-2 Google Scholar indexed journals tomography articles tomography Research articles tomography review articles tomography PubMed articles tomography PubMed Central articles tomography 2023 articles tomography 2024 articles tomography Scopus articles tomography impact factor journals tomography Scopus journals tomography PubMed journals tomography medical journals tomography free journals tomography best journals tomography top journals tomography free medical journals tomography famous journals tomography Google Scholar indexed journals
Article Details
Abbreviations:
ARDS- Acute Respiratory Distress Syndrome; CMR- Cardiac Magnetic Resonance; TTE- Transthoracic Echocardiography; LGE- Late gadolinium enhancement; LV- Left ventricle; LVEF- Left ventricular ejection fraction
1. Introduction
Cardiac Magnetic Resonance (CMR) provides valuable clinical information in the characterization of myocardial injury secondary to COVID-19 infection. CMR not only provides reliable function quantification, but it can also detect acute inflammatory changes and necrotic damage [1]. Moreover, CMR results may have prognostic implications and hence guide clinical management of COVID-19 patients. However, information on the clinical use of CMR to date is limited, possibly due to a misperception of increased risk of infection to health workers, despite not involving direct contact with patients, as do other imaging modalities as, for example, echocardiography. Given that the health crisis will last, CMR Imaging Units will have to adapt the way they operate and redefine indications in times of COVID. Initial reports identified myocarditis as the main cardiac lesion triggered by COVID-19 and, less frequently, cases of a Tako-Tsubo-like syndrome [2,3]. Early diagnosis has proven key in initiating appropriate medical treatment, including aggressive anti-inflammatory therapy with corticosteroids and IL-6 inhibitors [4] or antiplatelet management. Here, we present several COVID-19 clinical cases where CMR plays a role in the differential diagnosis of various forms of cardiac damage at different stages of the disease, both during hospitalization and at follow up after discharge, with prognostic implications. Furthermore, the risk of misdiagnosis of non-COVID cardiomyopathies is yet another challenge we should be attentive to, as represented by two of the following cases. Demographic data, clinical symptoms, PCR test results, blood testing, imaging modalities, and clinical management for each are shown in Table 1.
AZT: Azithromycin; AMX: Amoxiclavulanic; ARDS: Acute respiratory distress syndrome; CT: Computed tomography; BPI: Bilateral pulmonary infiltrates. EKG: Electrocardiogram; HCQ: Hydroxychloroquine; LV: Left ventricular. NA: No available.
Table 1: Demographic data, symptoms, PCR and blood testing, imaging modalities results and clinical management for each case.
2. Cases
2.1 CMR in hospitalized COVID-19 patients (acute phase)
2.1.1 Case 1: A 70-year-old man with positive PCR for COVID-19 was admitted to the Intensive Unit Care with acute respiratory distress syndrome (ARDS) and moderately reduced left ventricular (LV) ejection fraction (LVEF) on transthoracic echocardiography (TTE). During hospitalization, the patient had atypical chest pain and elevated troponin levels. CMR was performed at 2 weeks showing normal LVEF, absence of edema, and negative late gadolinium enhancement (LGE) (Figure 1A-C). These results indicate a transient myocardial dysfunction possibly induced by excessive catecholaminergic stimulation or cytokine storm with full recovery of LVEF within a short period of time, suggestive of stress cardiomyopathy.
2.1.2 Case 2: A 35-year-old male with positive Ig-G anti-COVID-19 antibodies, presented with acute chest pain worsening with decubitus. TTE showed a normal LVEF with inferolateral hypokinesis. Troponin levels were increased. CMR showed increased mild signal intensity on T2-STIR sequences in the basal segment of the inferolateral wall. On LGE, there was subepicardial delayed enhancement in the inferior and inferolateral walls at the basal and mid segments (Figure 1D-F). Diagnosis was compatible with acute myocarditis.
2.1.3 Case 3: A 21-year-old man consulted for dyspnea, chest pain and ageusia. Test results were positive for Ig-G anti-COVID-19 antibodies, negative PCR and positive troponins. ECG was normal and TTE showed severe left ventricular dysfunction. CMR was performed at day 7 of admission, which showed normal LVEF (online video 1), mild involvement of the apical lateral wall with subepicardial hyperintensity on T2-STIR and LGE, coincident with mild pericardial effusion (Figure 1G-I). Although these findings suggest mild subacute inflammation as the main diagnosis, they cannot explain the severity of the acute event. Therefore, additional cardiac damage may be explained by other mechanisms such as sepsis or excessive catecholaminergic stimulation.
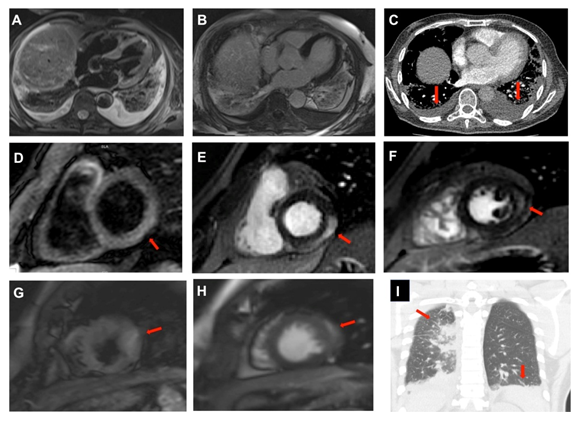
Figure 1: Imaging in hospitalized COVID-19 patients (acute phase). Top Panels (Case 1). T2-STIR (A) and LGE (B) CMR images without pathological cardiac findings. Chest CT showing bilateral pulmonary infiltrates and pleural effusion (arrows) (C); Middle Panels (Case 2). T2-STIR showing mild epicardial increased signal intensity in the basal inferolateral wall (D), coincident with subepicardial enhancement in the inferior and inferolateral walls on LGE (arrows) (E-F); Bottom Panels (Case 3). T2-STIR images showing mild subepicardial hyperintensity at the apical lateral wall (G) coincident with subepicardial enhancement on LGE (arrows) (H). Chest CT showing bilateral pleural effusion and upper right lung consolidation (arrows) (I).
2.2 CMR in a COVID-19 patient recently discharged from the Hospital (subacute phase)
2.2.1 Case 4: Two weeks after hospital discharge, a 41-year-old man with positive PCR and previous ARDS, presented in the Emergency Room with atypical chest pain and positive troponin levels. Due to a poor acoustic window on TTE, a CMR study was requested. CMR showed a normal-size LV with global hypokinesia causing mild dysfunction (LVEF of 50%), and absence of edema and LGE (Figure 2A-C). In this case, CMR allowed accurate quantification of LV volume and function, overcoming a poor-quality TTE. Although the initial clinical suspicion was myocarditis, CMR did not show any evidence of acute inflammation or fibrosis. Coronary artery disease hence needs to be ruled out as a cause of the episode.
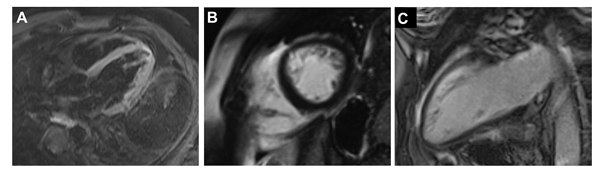
Figure 2: CMR imaging in a COVID-19 patient recently discharged from the Hospital (subacute phase) (Case 4). STIR (A) and LGE (B-C) images with normal myocardial signal.
2.3 CMR diagnosis of non-COVID-19 cardiomyopathies in times of COVID-19
2.3.1 Case 5: A 29-year-old man with Alport syndrome on hemodialysis was admitted to the Intensive Care Unit with ARDS under the suspicion of COVID-19 cardiac injury. Initial testing showed increased cardiac enzymes, normal ECG and biventricular dysfunction on TTE with limited visualization. CMR accurately quantified biventricular volumes and function, showing severe LV dysfunction and dilatation (online video 2), compatible with chronic cardiomyopathy. Tissue characterization with T1 and T2 mapping sequences were performed showing prolonged native T1 values (1386 ± 18 ms, normal range 1232 ± 51 ms), with normal T2 mapping and T2-STIR. LGE was not performed due to severe renal failure. Prolonged native T1 mapping with normal T2 mapping and T2-STIR images suggest the presence of diffuse myocardial fibrosis, possibly due to uremic cardiomyopathy secondary to the underlying chronic kidney disease (Figure 3A-C). During hospitalization, both PCR and antiCOVID-19 test results were negative.
2.3.2 Case 6: A 70-year-old man was referred to a routine CMR for aortic insufficiency evaluation in our Center. CMR incidentally showed changes in signal intensity at posterior lung parenchyma, suggestive of ground glass pattern and subepicardial /intramyocardial fibrosis in the basal inferolateral on LGE (Figure 3D-F). On clinical history the patient reported a recent history of COVID-19 infection in clinical remission, compatible with pulmonary and cardiac CMR incidental findings.
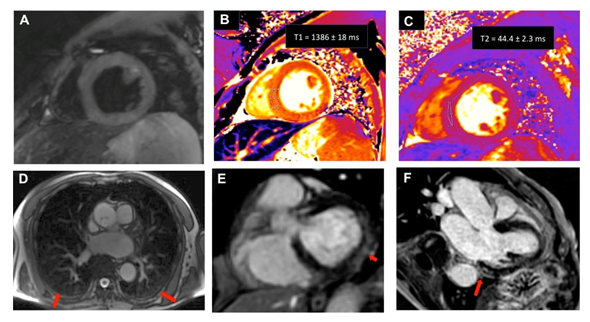
Figure 3: CMR diagnosis of non COVID-19 cardiomyopathies in times of COVID-19. Top Panels (Case 5). T2-STIR images with normal signal intensity (A). T1 (B) and T2 mapping (C) images showing prolonged native T1 (1386 ± 18 ms, normal range 1232 ± 51 ms), and normal T2 mapping (44.4 ± 2.3 ms, normal range from 39.9 to 50.1 ms). Botton Panels (Case 6). Pulmonary CMR incidental findings at posterior lung parenchyma. (arrows) (D). LGE images showing subepicardial/intramyocardial enhancement in the basal inferolateral wall (E-F).
3. Discussion
COVID-19 era entails an important diagnostic challenge for cardiac imaging. CMR may help in the characterization of myocardial injury at different phases of the disease, as we have shown in cases 1 to 4, including acute/subacute myopericarditis and stress cardiomyopathy, in agreement with previous studies [5,6]. Interestingly, two patients presented with significant left ventricular dysfunction in the acute phase followed by a rapid LVEF recovery without evidence of myocardial scarring on follow-up-CMR, probably in the context of systemic inflammation, hypoxic damage, and a coexisting procoagulant state. Thus, CMR may be particularly useful in providing a differential diagnosis for COVID-19 cardiac damage and hence, guide clinical management [7]. As shown in cases 4 and 5, CMR overcome echocardiographic limitations, such as poor echocardiographic window or limited echo quality by the inconvenience of performing an echo in a COVID setting, because it provides accurate LVEF quantification. Furthermore, CMR can improve diagnostic accuracy by tissue characterization over troponin levels, which may proof to be less specific in a complex, multisystemic disease such as COVID-19 (as shown by the poor correlation between troponin levels and CMR findings). It is important to note that chronic cardiac diseases unrelated to COVID-19 may be underdiagnosed during the current health crisis, as was the case in 5. Under normal circumstances, diagnosis may have been clear but clinical suspicion of COVID-19 infection challenges its assessment. Finally, CMR must be able to diagnose extracardiac and cardiac incidental findings compatible with COVID-19 infection, past or current. Case 6 shows the presence of pulmonary involvement compatible with previous COVID-19 infection and myocardial fibrosis in probable relation to the disease. The wide variety presented in these cases reflects the importance of CMR in the COVID-19 era. CMR units should keep in mind that any patient might be potentially infected and hence, safety and protection measurements must be implemented. Also, specialists must receive proper equipment and training to ensure safety in managing patients. In this context, the Society of CMR has recently provided guidance for the practice of CMR during the COVID-19 era [3]. Recommendations include the use of a single scanner and implementing shortened protocols. Organizational changes to attend both COVID and non-COVID patients and updated in CMR protocols of each CMR Unit are needed. Carrying out CMR scans for COVID patients at specific time during the day, selecting ambulatory cases, carrying out exhaustive sanitizing of facilities between scans, applying shorter acquisition protocols which should ideally be planned in advance, as well as carrying out remote imaging supervision and offline CMR analysis are among some of the measures that we have implemented in our Center.
In conclusion, the current COVID-19 pandemic has imposed a new reality, which has affected all areas of healthcare, including the CMR field. We have observed different CMR patterns of cardiac involvement at different phases of COVID-19 infection, each representing different diagnostic challenges. CMR can help understanding the cardiac involvement of this novel disease in terms of diagnosis, clinical management and will most probably be key in understanding mid-long term cardiac damage.
4. Take-Home Messages
- CMR has an important role in characterizing the various presentations of cardiac involvement of COVID-19, which may inform clinical treatment and prognosis.
- A wide differential diagnosis should be considered while characterizing myocardial injury in COVID-19 patients, including transient LV dysfunction secondary to direct and indirect, systemic mechanisms.
- CMR acquisition protocols, patients and staff safety and pre-procedural planning must be revised and updated to meet the challenges imposed by the COVID era.
- Extracardiac findings, such as pulmonary infiltrations on CMR, are key in asymptomatic patients in the diagnosis of current or past covid-19 infection.
5. Learning Objectives
- These clinical cases demonstrate the various clinical presentations of cardiac damage in COVID-19, characterized by CMR, both during hospitalization and ambulatory settings.
- CMR studies inform diagnosis, clinical management, and prognosis, and will be key in understanding longer-term cardiac involvement of COVID-19.
- Cardiac imaging Units need to adapt to meet the challenges imposed by COVID-19, including case selection, adapted acquisitions protocols, and safety procedures to guarantee patient and healthcare professional safety.
Funding
LFF has received funding from the Instituto de Salud Carlos III, Spain (PI15/02019). LFF, AM y ASM have received funding from Comunidad de Madrid (AORTASANA-CM; B2017/BMD-3676), Fondo Social Europeo (FSE).
Conflict of Interest
None of the authors have conflict of interest relevant to the subject material in this paper without financial relationships.
References
- Doherty JU, Kort S, Mehran R, et al. ACC/AATS/AHA/ASE/ASNC/HRS/SCAI/SCCT/SCMR/STS 2019 appropriate use criteria for multimodality imaging in the assessment of cardiac structure and function in nonvalvular heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of .... Journal of the American College of Cardiology 73 (2019): 488-516.
- Atri D, Siddiqi HK, Lang J, et al. COVID-19 for the cardiologist: a current review of the virology, clinical epidemiology, cardiac and other clinical manifestations and potential therapeutic strategies. JACC: Basic to Translational Science (2020).
- Han Y, Chen T, Bryant J, et al. Society for Cardiovascular Magnetic Resonance (SCMR) guidance for the practice of cardiovascular magnetic resonance during the COVID-19 pandemic. Journal of Cardiovascular Magnetic Resonance: Official Journal of the Society for Cardiovascular Magnetic Resonance 22 (2020): 26.
- Coyle J, Igbinomwanhia E, Sanchez-Nadales A, et al. A Recovered Case of COVID-19 Myocarditis and ARDS Treated with Corticosteroids, Tocilizumab, and Experimental AT-001. JACC: Case Reports (2020).
- Long B, Brady WJ, Koyfman A, et al. Cardiovascular complications in COVID-19. The American Journal of Emergency Medicine (2020).
- Minhas AS, Scheel P, Garibaldi B, et al. Takotsubo Syndrome in the Setting of COVID-19 Infection. JACC: Case Reports (2020).
- Huang L, Zhao P, Tang D, et al. Cardiac involvement in recovered COVID-19 patients identified by magnetic resonance imaging. JACC: Cardiovascular Imaging (2020).
