Bioclinical Performance of Liver Cirrhosis and Hepatocarcinoma Diagnosis versus Abdominal Ultrasound-Hepatic Histopathology at Kinshasa University Clinics between 1990 and 2004
Article Information
Malenga Mpaka Serge1,2, Longo-Mbenza Benjamin1,3, Lelo Tshikwela Miche2, Pakasa Muyulu Nestor4, Tshimpi Wola Yaba Antoine5, Mbendi Nlombi Charles5, Kisoka Lusunsi Christian1, Mawalala Malengele Héritier1,2
1Department of Public Health, Lomo University of Research, Kinshasa, Democratic Republic of Congo
2Department of Radiology, University Clinics of Kinshasa, Kinshasa, Democratic Republic of Congo
3Cardiology Service, Department of Internal Medicine, University Clinics of Kinshasa, Kinshasa, Democratic Republic of Congo
4Department of Anatomopathology, University Clinics of Kinshasa, Kinshasa, Democratic Republic of Congo
5Service of Hepato-gastro-enterology, Department of Internal Medicine, University Clinics of Kinshasa, Kinshasa, Democratic Republic of Congo
*Corresponding Author: Longo-Mbenza Benjamin. Department of Public Health, Lomo University of Research, Kinshasa, Democratic Republic of Congo
Received: 15 April 2023; Accepted: 24 April 2023; Published: 22 August 2023
Citation: Malenga Mpaka Serge, Longo-Mbenza Benjamin, Lelo Tshikwela Miche, Pakasa Muyulu Nestor, Tshimpi Wola Yaba Antoine, Mbendi Nlombi Charles, Kisoka Lusunsi Christian, Mawalala Malengele Héritier. Bioclinical Performance of Liver Cirrhosis and Hepatocarcinoma Diagnosis versus Abdominal Ultrasound-Hepatic Histopathology at Kinshasa University Clinics between 1990 and 2004. Journal of Radiology and Clinical Imaging. 6 (2023): 173-181
View / Download Pdf Share at FacebookAbstract
Introduction: Hepatic cirrhosis is the final stage in the natural history of chronic liver diseases. Hepatocarcinoma is a form of cancer that develops from the cellular anarchy of the liver. The objective of this study was to measure the diagnostic performance of bioclinical and abdominal ultrasound information suspecting liver cirrhosis and hepatocarcinoma in front of liver biopsy as a reference test for the diagnosis of liver cirrhosis and hepatocarcinoma.
Materials and Methods: The Departments of Gastroenterology, Radiology, and Pathological Anatomy, Faculty of Medicine of Kinshasa, served as a framework for this work which adopted a secondary analysis of clinical, biological and ultrasound information. Sensitivity, specificity, concordance, predictive values, ROC curves and statistical analyzes specified the levels of diagnostic performance of the bioclinical workup of liver cirrhosis and hepatocellular carcinoma.
Results: Among 200 patients, including 142 men and 58 women with a mean age of 47 ± 15 years, 67% (n=) and 43.5% (n=) had cirrhosis and hepatocarcinoma respectively on histopathology. The increase in transaminases, but anemia, hypoalbuminemia and abdominal ultrasound had better diagnostic performance of liver cirrhosis histopathology. Only abdominal ultrasound had an excellent sensitivity for histopathological diagnosis while clinical hepatomegaly, sensitive liver and transaminases had poor diagnostic performances of histopathological hepatocarcinoma.
Conclusion: Abdominal ultrasound is becoming an essential non-invasive examination in the histopathological diagnosis of liver cirrhosis and hepatocellular carcinoma at the University Clinics of Kinshasa, DR Congo.
Keywords
Hepatic cirrhosis; Hepatocarcinoma; Abdominal ultrasound; Hepatic histopathology
Hepatic cirrhosis articles; Hepatocarcinoma articles; Abdominal ultrasound articles; Hepatic histopathology articles
Hepatic cirrhosis articles Hepatic cirrhosis Research articles Hepatic cirrhosis review articles Hepatic cirrhosis PubMed articles Hepatic cirrhosis PubMed Central articles Hepatic cirrhosis 2023 articles Hepatic cirrhosis 2024 articles Hepatic cirrhosis Scopus articles Hepatic cirrhosis impact factor journals Hepatic cirrhosis Scopus journals Hepatic cirrhosis PubMed journals Hepatic cirrhosis medical journals Hepatic cirrhosis free journals Hepatic cirrhosis best journals Hepatic cirrhosis top journals Hepatic cirrhosis free medical journals Hepatic cirrhosis famous journals Hepatic cirrhosis Google Scholar indexed journals Hepatocarcinoma articles Hepatocarcinoma Research articles Hepatocarcinoma review articles Hepatocarcinoma PubMed articles Hepatocarcinoma PubMed Central articles Hepatocarcinoma 2023 articles Hepatocarcinoma 2024 articles Hepatocarcinoma Scopus articles Hepatocarcinoma impact factor journals Hepatocarcinoma Scopus journals Hepatocarcinoma PubMed journals Hepatocarcinoma medical journals Hepatocarcinoma free journals Hepatocarcinoma best journals Hepatocarcinoma top journals Hepatocarcinoma free medical journals Hepatocarcinoma famous journals Hepatocarcinoma Google Scholar indexed journals Abdominal ultrasound articles Abdominal ultrasound Research articles Abdominal ultrasound review articles Abdominal ultrasound PubMed articles Abdominal ultrasound PubMed Central articles Abdominal ultrasound 2023 articles Abdominal ultrasound 2024 articles Abdominal ultrasound Scopus articles Abdominal ultrasound impact factor journals Abdominal ultrasound Scopus journals Abdominal ultrasound PubMed journals Abdominal ultrasound medical journals Abdominal ultrasound free journals Abdominal ultrasound best journals Abdominal ultrasound top journals Abdominal ultrasound free medical journals Abdominal ultrasound famous journals Abdominal ultrasound Google Scholar indexed journals Hepatic histopathology articles Hepatic histopathology Research articles Hepatic histopathology review articles Hepatic histopathology PubMed articles Hepatic histopathology PubMed Central articles Hepatic histopathology 2023 articles Hepatic histopathology 2024 articles Hepatic histopathology Scopus articles Hepatic histopathology impact factor journals Hepatic histopathology Scopus journals Hepatic histopathology PubMed journals Hepatic histopathology medical journals Hepatic histopathology free journals Hepatic histopathology best journals Hepatic histopathology top journals Hepatic histopathology free medical journals Hepatic histopathology famous journals Hepatic histopathology Google Scholar indexed journals ROC curve articles ROC curve Research articles ROC curve review articles ROC curve PubMed articles ROC curve PubMed Central articles ROC curve 2023 articles ROC curve 2024 articles ROC curve Scopus articles ROC curve impact factor journals ROC curve Scopus journals ROC curve PubMed journals ROC curve medical journals ROC curve free journals ROC curve best journals ROC curve top journals ROC curve free medical journals ROC curve famous journals ROC curve Google Scholar indexed journals hepatocellular carcinoma articles hepatocellular carcinoma Research articles hepatocellular carcinoma review articles hepatocellular carcinoma PubMed articles hepatocellular carcinoma PubMed Central articles hepatocellular carcinoma 2023 articles hepatocellular carcinoma 2024 articles hepatocellular carcinoma Scopus articles hepatocellular carcinoma impact factor journals hepatocellular carcinoma Scopus journals hepatocellular carcinoma PubMed journals hepatocellular carcinoma medical journals hepatocellular carcinoma free journals hepatocellular carcinoma best journals hepatocellular carcinoma top journals hepatocellular carcinoma free medical journals hepatocellular carcinoma famous journals hepatocellular carcinoma Google Scholar indexed journals Democratic Republic of Congo articles Democratic Republic of Congo Research articles Democratic Republic of Congo review articles Democratic Republic of Congo PubMed articles Democratic Republic of Congo PubMed Central articles Democratic Republic of Congo 2023 articles Democratic Republic of Congo 2024 articles Democratic Republic of Congo Scopus articles Democratic Republic of Congo impact factor journals Democratic Republic of Congo Scopus journals Democratic Republic of Congo PubMed journals Democratic Republic of Congo medical journals Democratic Republic of Congo free journals Democratic Republic of Congo best journals Democratic Republic of Congo top journals Democratic Republic of Congo free medical journals Democratic Republic of Congo famous journals Democratic Republic of Congo Google Scholar indexed journals white blood cell articles white blood cell Research articles white blood cell review articles white blood cell PubMed articles white blood cell PubMed Central articles white blood cell 2023 articles white blood cell 2024 articles white blood cell Scopus articles white blood cell impact factor journals white blood cell Scopus journals white blood cell PubMed journals white blood cell medical journals white blood cell free journals white blood cell best journals white blood cell top journals white blood cell free medical journals white blood cell famous journals white blood cell Google Scholar indexed journals True Positivity Index articles True Positivity Index Research articles True Positivity Index review articles True Positivity Index PubMed articles True Positivity Index PubMed Central articles True Positivity Index 2023 articles True Positivity Index 2024 articles True Positivity Index Scopus articles True Positivity Index impact factor journals True Positivity Index Scopus journals True Positivity Index PubMed journals True Positivity Index medical journals True Positivity Index free journals True Positivity Index best journals True Positivity Index top journals True Positivity Index free medical journals True Positivity Index famous journals True Positivity Index Google Scholar indexed journals False Positive Index articles False Positive Index Research articles False Positive Index review articles False Positive Index PubMed articles False Positive Index PubMed Central articles False Positive Index 2023 articles False Positive Index 2024 articles False Positive Index Scopus articles False Positive Index impact factor journals False Positive Index Scopus journals False Positive Index PubMed journals False Positive Index medical journals False Positive Index free journals False Positive Index best journals False Positive Index top journals False Positive Index free medical journals False Positive Index famous journals False Positive Index Google Scholar indexed journals
Article Details
1. Introduction
Hepatic cirrhosis is a chronic inflammatory process and accompanied by an accumulation of fibrosis and an alteration in the architecture of the liver [1,2]. Hepatocellular carcinoma or hepatocellular carcinoma (HCC) is a form of cancer that develops from cell anarchy of the liver (hepatocyte) and is the most common primary liver cancer occurring in patients with cirrhosis and chronic liver disease [3.4]. And hepatic cirrhosis is predominant among the important causes of hepatocellular carcinoma like excess alcohol, smoking and viral infections (Hepatitis B and Hepatitis C)[5]. Worse still, hepatic cirrhosis is the culmination of a chronic inflammatory process leading to a deposit of fibrosis and an alteration of the architecture of the liver and frequently provoked by toxic agents (excess alcohol, viral hepatitis, disorders metabolic disorders (hemochromatosis and Wilson's disease) and mechanical disorders such as biliary obstruction[6-10]. In the Democratic Republic of Congo (DRC) studies of hepatic cirrhosis are still evaluated according to clinical expression at the University Clinics of Kinshasa (communication presented Longo Mbenza and Malenga): 75% of cases of hepatic cirrhosis due to excess alcohol against 25% of cases of hepatic cirrhosis due to viral hepatitis[11]. The introduction of abdominal ultrasound in the DRC was facilitated in 1990 by the following pioneers: Longo Mbenza Benjamin, Matusila Anatole, Manono Roger, Bongo Bahati, Lelo Michel, Ndoma Emmanuel and Molua Antoine. Indeed the introduction of ultrasound in the DRC has profoundly upset the diagnostic strategies of hepatic cirrhosis and hepatocellular carcinoma in order to follow in the footsteps of researchers working in developed and rich countries.[12,13]. The diagnostic performance of abdominal ultrasound focused on the full parenchyma of the abdomen (liver, spleen, kidneys, lymph nodes and vessels) is well established to date in the detection of hepatic cirrhosis and hepatocellular carcinoma against the reference test according to liver biopsy[14]. The lack of scientific publication relating to the performance of symptomatology, clinical biology and the performance of abdominal ultrasound as a reference test (Gold Standard) in the detection of hepatic cirrhosis and hepatocarcinoma justified the initiative of this study. The objective of this study was to identify the main qualities of the bioclinical and ultrasound data likely to be measured in terms of diagnostic performance of hepatic cirrhosis and hepatocellular carcinoma and to discriminate between the latter diagnoses after histopathological study of liver biopsies.
2. Methods and materials
2.1 Nature, framework and period of the study
The present mixed study adopted a secondary analysis of information from the pathology department of the University of Kinshasa, the gastroenterology department of the Cliniques Universitaires de Kinshasa and the radiology department of the Cliniques Universitaires de Kinshasa in a consecutive series of all patients examined between January 1, 1990 and December 31, 2004.
Sampling of the study population was exhaustive and convenient.
The bioclinical data collected were as follows: sex, age, ascites, melena, lower limb edema (OMI), collateral circulation, sloping dullness, flow sign, icicle sign, hepatomegaly, irregular surface of the liver, sharp edge, abdominal pain. , abdominal bloating, physical asthenia, jaundice, fever, palpated liver, tender liver, firm consistency, hemoglobin, hematocrit, white blood cell, ESR, prothrombin, SGOPT/AST, SGPT/ALT, total bilirubin, direct bilirubin, indirect bilirubin, fibrinogen.
The ultrasound data (ultrasound hepatomegaly, irregular outline, heterogeneous echostructure of the liver, macronodular aspect of the liver on ultrasound) were observed and obtained using an ACUSON XP 10 ultrasound scanner (Philadelphia, USA) using 3.5 Mhz transducers, of 5 Mhz and 7.5 Mhz according to the corpulence and the thinness of the patients.
2.2 Operational definitions
Histopathological studies have defined hepatic cirrhosis by a set of irreversible lesions associating fibrosis, nodular regeneration process and profound modification of the vascularization of the parenchyma.[15].
Whereas hepatocarcinoma was defined by lesions that were more heterogeneous, as they were traversed by partitions or foci of fibrosis, remodeled by necrotic and haemorrhagic foci, sometimes calcified, which gave them a very varied color, vascularized mainly by the arterial network. It invades the lumen of the portal veins (intrahepatic veins and the trunk of the portal vein), suprahepatic veins, bile ducts[16.17].
Abdominal ultrasound defined hepatic cirrhosis by disharmonious changes in liver size, finely bumpy hepatic contours, macronodules easier to visualize than micronodules (1 to 3 mm), liver parenchyma being homogeneous or heterogeneous, then that the hepatocarcinoma was defined in its nodular form by its round or polylobed form, hypo or hyperechoic with peripheral hypoechoic halo which was evocative, in its infiltrative form by a range of poorly limited heterogeneous echostructure, the vascular extension especially the invasion portal manifested by the presence of intraluminal echogenic material in the enlarged portal branch, the wall remaining visible in the form of a hyperechoic border, biliary extension by dilation of the intrahepatic bile ducts,lymph node extension at the level of the hepatic and coeliomesenteric pedicle.
2.3 Statistical analyzes
The evaluation of bioclinical methods and clinical diagnoses of hepatic cirrhosis and hepatocarcinoma was carried out by their internal validity, measurement of agreement (efficiency or concordance) and decisional choice using ROC curves ( Receiver Operating Curves)[18.19]. This diagnostic value of the bioclinical tests was measured in comparison with the real diagnosis provided by the reference test or Gold Standard represented by abdominal ultrasound using four-box tables (contingencies or Latin square)[20].
Internal validity was considered as the ability to correctly make the histopathological diagnosis of hepatic cirrhosis and hepatocellular carcinoma in the form of the following indices: sensitivity, specificity, medical decision indices by predictive values, and external validity (the reproducibility of several diagnostic tests, the reference rate, the proportion of agreement, indicating the probability of obtaining the same results)[20].
The cost-effectiveness estimate of the clinical trials explored referred to the proportion of clinician-referred patients participating in the cost to themselves, family, or employee.
In relation to this notion, the importance of the groups of True Positive, False Positive and False Negative patients was an element that entered into the estimation of the predictive efficacy of a clinical test (or clinical diagnosis). For this reason, the following indices have been defined:
the True Positivity Index (VPI) was equal to the number of patients referred divided by the number of True Positive patients (expression of the cost-effectiveness ratio of a disease predictor test). The higher the number of True Positive patients, the more the IVP decreased and the more the predictive clinical test explored was effective for the diagnosis of the disease;
the False Positive Index (FPI) was equal to the number of referred patients divided by the number of False Positive patients. Unlike IVP, IFP expressed an unfair burden on patients who were unnecessarily referred and on the support system (Family, Friends, Business). The higher the number of False Positive patients, the lower the IFP and the lower the specificity of the clinical test for the diagnosis of the disease.
The agreement was described as excellent for a K coefficient between 0.81 and 1, good for values 0.61 to 0.80, average for values 0.41 to 0.60, poor between 0.21 and 0.40, and bad between 0 and 0.29
[21-23].
The statistical tests were concluded with a type I risk of 0.05. Confidence intervals were calculated with the same 5% risk (95% CI)
The data entered on a personal computer with the EPI INFO version 6.04 software were represented by their means + standard deviations for the quantitative variables and by their absolute frequencies (n) and their relative frequencies or proportions (in percentage) for the variables. qualitative.
The comparison of the proportions was carried out by means of Yates Corrected if it was necessary.
The comparison of the means was carried out by using the Student's t-test for the normally distributed continuous variables and by using the Kruskall-Wallis H-test for the asymmetric continuous variables.
The association between two qualitative variables in univariate analysis was determined by calculating the odds ratio or Odd Ratio (OR) with its 95% confidence interval (95% CI) and the Mantel-Haenszel Chi-Square test. OR was a measure of the strength or intensity of the statistical association between two variables.
The value of p<0.05 was considered as the threshold of statistical significance.
3. Results
A total of 200 patients including 142 men and 58 women were examined with a sex ratio of 3 Men:1 Woman: 71% men and 29% women.
The mean age was 47.4±15.1 years (extreme 16 years and 82 years).
Given that the number of 87 cases of hepatic cirrhosis and 61 cases of hepatocarcinoma diagnosed on histopathological study were respectively consistent on abdominal ultrasound, the ultrasound approach to the liver was considered as the reference test in front of their sensitivity of 100% and specificity of 100%.
3.1 Diagnostic performance of the bioclinical approach
The icicle sign(13.4% n=18 versus 7.6% n=5)and the irregular surface of the liver( 50% n=47 versus 35.2% n=19)on clinical examination were indifferent to distinguish the presence of bioclinical hepatic cirrhosis and the absence of cirrhosis (p>0.05), whereas ascites (57.5% n=77 versus 25.8% n=18 p<0.0001), the maelena(12.7% n=17 versus 3% n=2 p <0.05),edema of the lower limbs(37.3% n=50 versus 9.1% n=6 p<0.0001),collateral circulation(32.8% n=40 versus 10.6% n=7 p<0.001), dullness slopes(37.3% n=50 versus 19.7% n=13 p<0.01),the wave sign(26.9% n=36 versus 10.6% n=7 p<0.01),hepatomegaly(83% n=78 versus66.7%n=36 p<0.05) and the sharp edges of the liver(57.4% n=54 versus 27.8% n=15 p<0.001)were the respective and significant discriminators of the presence of histopathological hepatic cirrhosis.
Patients with histopathological cirrhosis were older (49.7 ±14.7 years) than their colleagues without histopathological cirrhosis (42.7±15.1 years), the difference being statistically very significant (p<0.001).
Table 1: Histopathological hepatic cirrhosis and continuous parameters
|
Variables |
Presence |
Absence |
P |
|
Pre-hepatic dullness (cm) |
8.7±4 |
10.5±3.8 |
<0.05 |
|
Hemoglobin (gr%) |
9.4±2.7 |
10.2±3.1 |
0.08 |
|
Hematocrit(%) |
28.7±7.3 |
33.2±11.7 |
<0.05 |
|
Prothrombin(%) |
60.8±20.1 |
74.7±16.5 |
<0.001 |
|
Albuminemia (%) |
26.3±13.3 |
74.7±16.5 |
<0.05 |
|
SGOT |
76.3±72.4 |
89.9±148.7 |
0.09 |
|
SGPT |
49.8±75.6 |
65.8±102 |
NS |
At identical mean values (p>0.05) of hemoglobin, SGOT, and SGPT, the mean values of hematocrit, prothrombin and albuminemia of cirrhotics were more reduced (p<0.001) than those of patients without histopathological cirrhosis (Table 1).
Table 2: Ultrasound data according to the presence of histopathological hepatocarcinoma
|
Variables |
Presence |
Absence |
P |
|
Hepatomegaly ultrasound |
57 (96.6) |
56 (46.7) |
<0.000001 |
|
Irregular contours on ultrasound |
51 (83.6) |
61 (43.9) |
<0.000001 |
|
Echostructure liver heterogeneous |
55 (90.2) |
72 (51.8) |
<0.000001 |
|
Macronodular appearance From liver to ultrasound |
45 (73.8) |
26 (18.7) |
<0.000001 |
Table 2 shows that hepatomegaly (enlarged liver volume), irregular contours, heterogeneous echostructure of the liver, macronodular appearance of the liver on ultrasound were the very significant discriminators (p<0.000001) of the presence of histopathological hepatocarcinoma.
Table 3: Clinical data according to the presence of histopathological hepatocellular carcinoma
|
Variables |
Presence |
Absence |
P |
|
Abdominal pain |
46 (75.4) |
80 (57.6) |
<0.01 |
|
Bloat abd. |
25 (41) |
25 (41) |
NS |
|
Physical asthenia |
21 (34.4) |
64 (46) |
NS |
|
Jaundice |
9 (14.8) |
36 (25.9) |
NS |
|
Fever |
13 (21.3) |
29 (20.9) |
NS |
|
Melena |
3 (4.9) |
16 (11.5) |
NS |
|
Collateral circulation |
24 (39.3) |
27 (19.4) |
<0.01 |
|
Liver palpated |
58 (95.1) |
90 (64.7) |
<0.00001 |
|
sensitive liver |
54 (93.1) |
62 (68.9) |
<0.001 |
|
Clinical hepatomegaly |
54 (93.1) |
60 (66.7) |
<0.0001 |
|
firm consistency liver |
34 (58.6) |
20 (22.2) |
<0.00001 |
|
Irregular surface liver |
41 (70.7) |
25 (27.8) |
<0.000001 |
|
Sharp edge |
39 (67.2) |
30 (33.3) |
<0.0001 |
Clinically, abdominal pain, collateral circulation, palpated liver, tender liver, clinical hepatomegaly, firm consistency, irregular liver surface and sharp edge respectively and very significantly discriminated the presence of the histopathological hepatocarcinoma of the absence of histopathological hepatocarcinoma (Table 3).
Table 4: Biological data according to the presence of hepatocarcinoma on liver ultrasound
|
Variables |
Presence |
Absence |
P |
|
Age (years) |
47.7±15.5 |
47.2±15 |
NS |
|
Hemoglobin (g%) |
9.8±2.7 |
9.6±2.9 |
NS |
|
Hematocrit (%) |
30.4±6.9 |
30.4±10.2 |
NS |
|
White blood cell (/mm) |
9441.3±4263.8 |
8903.9±7275.6 |
NS |
|
VS (mm/H) |
75.2±34.9 |
54.9±40.1 |
<0.01 |
|
Prothrombin (%) |
67.1±21.3 |
63.7±19.3 |
NS |
|
SGOT (IU/L) |
108.4±151.6 |
69.3±72.3 |
NS |
|
SGPT (IU/L) |
67.6±95.5 |
50.1±80.6 |
NS |
|
Total bilirubin (mg/dl) |
4.9±6.2 |
7.6±17.7 |
NS |
|
Direct bilirubin (mg/dl) |
3.3±3.7 |
6.6±9.2 |
NS |
|
Indirect bilirubin (mg/dl) |
1.9±2.8 |
2.4±3.6 |
NS |
|
Fibrinogen (mg/dl) |
255.4±222.7 |
48.9±86.3 |
<0.0001 |
Only mean values of blood fibrinogen and blood sedimentation rate were able to discriminate the presence of histopathological hepatocellular carcinoma from the absence of hepatocellular carcinoma, the other biological parameters being irrelevant (Table 4).
4.4 Diagnostic Validity
4.4.1 Validity of the clinical diagnosis of hepatic cirrhosis
The diagnostic validity of bio-clinical cirrhosis against abdominal ultrasound being the reference test was characterized as follows: sensitivity = 88.5%, specificity = 49.5%, positive predictive value (PPV) = 57, 4%, negative predictive value (NPV) 84.8%, positive agreement proportion = 53.4%, negative agreement proportion = 45.5%, positive likelihood ratio = 1.78%, negative likelihood ratio = 0.22%, reference rate= 67%, reproductive (rough agreement) = 67%, KAPPA coefficient= 0.37 and Youden's india= 0.4.
4.4.2 Validity of hepatic semiology
Taking the increase in liver volume on abdominal ultrasound as a reference, clinical hepatomegaly (increase in volume revealed on clinical examination of the liver) provided valid information because of its excellent sensitivity.93.9%,of its good specificityby 61.9%, very high predictive values(PPV=85.3% and NPV=81.2%),likelihood ratios (LR+ tending to infinity and LR- equal to 0) very good gross agreement/accuracy reproducibility: the KAPPA coefficient was0.59.
To compare ultrasound hepatomegaly, the semiological sign of irregular surface of the liver on clinical examination carried weak valid information in comparison with the heterogeneous echostructure of the liver on ultrasound and taken as a reference test.
Sensitivity = 57.5%, specificity = 81.6%, positive predictive value = 86.3% and VPN= 48.7%, likelihood ratios (LR+ equal to 3.2 and LR- equal to 0.51) , KAPPA coefficient is 0.35 and Youden index is 0.4.
4.4.3 Diagnostic validity of clinical and ultrasound semiology in the diagnosis of hepatocellular carcinoma Clinical semiology
Table 5: Clinical semiology of the liver, hepatocarcinoma on ultrasound being the reference test
Table 5 presents the diagnostic validity of certain clinical signs relating to the liver, echographic hepatocarcinoma being the reference test.
As an interpretation, only the clinical signs clinical hepatomegaly and tender liver have excellent sensitivity and high cost. The reproducibility is good for the irregular surface of the liver, but the Kappa coefficient is mediocre for all the clinical signs explored, but the Negative Predictive Value is very high for all of these signs.
Table 6: Cost-effectiveness and statistical strength between clinical semiology and Hepatocarcinoma on ultrasound
|
Clinical semiology |
Cost-effectiveness |
OR (95% CI) |
|
Collateral circulation |
PVI = 8.3 |
2.7** |
|
PFI = 7.4 |
(1.4 - 5.2) |
|
|
Sharp edge |
PVI = 5.1 |
4.1**** |
|
PFI = 6.7 |
(2 - 8.3) |
|
|
Irregular surface |
PVI = 4.9 |
6.2**** |
|
PFI = 8 |
(3 - 13.1) |
|
|
firm consistency |
PVI = 5.9 |
4.9**** |
|
PFI = 10 |
(2.3 - 10.9) |
|
|
Clinical hepatomegaly |
PVI = 3.7 |
6.7**** |
|
PFI = 3.3 |
(2.4 - 23.5) |
|
|
sensitive liver |
PVI = 3.7 |
6*** |
|
PFI = 3.2 |
(2.1 - 21.3) |
|
|
Abdominal pain |
PVI = 4.3 |
2.3** |
|
PFI = 2.5 |
(1.2 - 4.5) |
Table 6 summarizes the cost-effectiveness estimate and the statistical strength/intensity between the signs explored and hepatocellular carcinoma.
The statistical strength is highly significant and higher for clinical hepatomegaly, tender liver, and irregular liver surface. But the IVP and IFP values are more reduced for clinical hepatomegaly, sensitive liver and abdominal pain.
3.2.4 Decisional choice in the prediction of hepatic cirrhosis on ultrasound after dosage of transaminases.

Figure 1: ROC curve illustrating prediction on ultrasound by SGOT levels at different thresholds: ≥ 30.2 IU/ml, ≥ 24 IU/ml, ≥ 45 IU/ml, ≥ 48 IU/ml, ≥ 55 IU/ml, ≥ 60 IU/ml, ≥ 65 IU/ml, ≥ 75 IU/ml and ≥ 85 IU/ml
Figure 1 shows that SGOT transaminases do not possess good ROC capability for hepatic cirrhosis on ultrasound in the study population.
There was a very significant positive linear relationship between sensitivity and 1-specificity where the ROC curve confirms the prediction of hepatic cirrhosis on abdominal ultrasound according to the threshold SGPT level threshold (Figure 2).
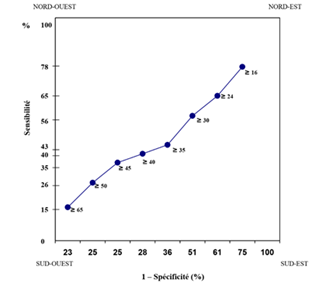
Figure 2: ROC curve illustrating the prediction of hepatic cirrhosis on ultrasound by SGPT levels at different thresholds: ≥ 16IU/ml, ≥ 24 IU/ml, ≥ 30 IU/ml, ≥ 35 IU/ml, ≥ 40 IU/ml , ≥ 45 IU/ml, ≥ 50 IU/ml and ≥ 65 IU/ml.
Indeed, there was an increase directly proportional to the increase in the value of sensitivity and the decrease in false positives of hepatic cirrhosis on abdominal ultrasound: SGPT ≥ 65 IU/ml better predicted the ultrasound diagnosis of hepatic cirrhosis ( figure 2).
4. Discussion
The present study analyzed the diagnostic performance of bioclinical data in the face of hepatic cirrhosis and hepatocarcinoma.
Abdominal ultrasound has been the reference test because of its very high sensitivity.[24]and the increasingly rare indication of liver biopsy with histopathological study[21-23.25]. The opportunity of ultrasound in hepatic pathology is moreover recognized as the scan of the poor[12,13].
The diagnostic validity of liver ultrasound is also recognized in the diagnosis of amoebic liver abscesses in other African countries.[15.26]. But such is not the case for the diagnostic validity of bioclinical data in the face of hepatic cirrhosis and primary liver cancer, anomalies most frequently encountered in Kinshasa.[12].
4.1 Demographic Data
In this study population, the vulnerability of men is very marked in this set of cases of hepatic cirrhosis and hepatocarcinoma:
The sex ratio was 3 male: 1 female. This vulnerability of the male sex is also reported in Italian patients with hepatic cirrhosis.[27].
Excessive alcohol consumption is more reported in men than in women[28]. The predominance of primary liver cancer in the male sex is established[28.29].
Men seem more exposed to cirrhogenic risk than women, but in a cirrhotic population, the risk of neoplastic transformation seems identical in both sexes.[29].
As demonstrated elsewhere in Africa, patients suffering from hepatic cirrhosis and primary liver cancer either young adults[11-13]. In Europe, on the contrary, patients are older around 60 years old.[27].
4.2 Discriminating Bioclinical Parameters of Hepatic Cirrhosis
Prehepatic dullness, hematocrit drop, hypoalbuminemia, hypothrombinemia, ascites, maelena, lower limb edema, collateral circulation, sloping dullness, flood sign, sharp edges of the liver and clinical hepatomegaly retain their classic discriminating values for cirrhosis of the patients examined[30]. On the other hand, SGOT and SGPT transaminases, the ice cube sign and the irregular surface of the liver have no discriminating power of hepatic cirrhosis.
Disturbance of liver tests (SGOT and SGPT) has already been reported in cirrhotic Africans from Bangui in the Central African Republic.[31].
4.3 Discriminating Bioclinical Parameters of Primary Liver Cancer
There are no significant liver test abnormalities in patients with hepatocellular carcinoma. Only elevation of fibrinogen, sedimentation rate, tender liver, collateral circulation, hepatomegaly, irregular surface of the liver, firm consistency of the liver and sharp edge of the liver are discriminating signs of primary cancer. liver. This suggests the malignant transformation of hepatic cirrhosis in the majority of cases.
This work therefore underlines the discriminating nature of all the sonographic characteristics of the liver in the face of hepatic cirrhosis such as sonographic hepatomegaly, the irregular outline of the liver on sonography and the macronodular appearance on sonography.[32].
The coupling of Doppler to ultrasound would have allowed the definition of portal hypertension and thrombosis of the portal vein[30]in case of hepatic cirrhosis and/or primary liver cancer.
4.4 Diagnostic Validity of Bioclinical Data
To our knowledge, there is no study that has analyzed the validity of hepatic semiology and routine hepatic blood biology in the diagnosis of cirrhosis and primary liver cancer, liver ultrasound being the reference test.
4.5 In patients with hepatic cirrhosis
The bioclinical diagnosis of hepatic cirrhosis has poor specificity, low reproducibility (accuracy) and a very high cost despite its very good sensitivity. Only clinical hepatomegaly has very good sensitivity, good specificity, very high positive and negative predictive values in flow, a moderate KAPPA coefficient and a very high cost.
The irregular surface of the liver on clinical examination seems useless in the diagnosis of cirrhosis because of a low sensitivity and a very low KAPPA coefficient.
4.6 In patients with primary liver cancer
Only the clinical signs, clinical hepatomegaly and tender liver, have excellent sensitivity and high cost (benchmark rate) in the diagnosis of primary liver cancer.
4.7 Boundaries
The nature of the present cross-sectional study is limited by the lack of the time variable, necessary in a causal association.
Conclusion
Routine hepatic blood laboratory and clinical diagnosis seems limited in the definite diagnosis of hepatic cirrhosis and hepatocarcinoma. Abdominal ultrasound should be mandatory in the diagnostic evaluation of chronic liver conditions such as hepatic cirrhosis and hepatocellular carcinoma.
State of knowledge on the subject
- Abdominal ultrasound becomes an essential non-invasive examination in the histopathological diagnoses of hepatic cirrhosis and hepatocarcinoma
- The diagnostic performance of abdominal ultrasound focused on the full parenchyma of the abdomen is well established to date in the detection of hepatic cirrhosis and hepatocarcinoma against the reference test according to liver biopsy.
Importance and scientific knowledge provided
- Contrary to the results reported by the literature coming from several countries, the innovation, the importance and the scientific knowledge were respectively approached by the uniqueness, the rigor and the mathematical model applied by this first Congolese study.
- The importance of the present study was underlined during the introductory section relating to the problematic as opposed to the problematic of the bioclinical performance of the diagnosis of hepatic cirrhosis and hepatocellular carcinoma against abdominal ultrasound-hepatic histopathology in a hospital environment in Kinshasa, which is often poor. Indeed, the availability of abdominal ultrasound validly replaces liver biopsy, an invasive technique that is often not interpreted by the absence of pathologists in Kinshasa, the capital of the DR Congo and even in all the provinces of the DR Congo.
- The scientific knowledge produced by this study will be a factual force to be used in the early and precise diagnosis, in the training of specialists in medical imaging / radiodiagnosis, in the prevention and improvement of the therapeutic management of hepatic cirrhosis.
Acknowledgments
We would like to pay tribute to our masters who participated in the realization of this work, but who unfortunately left us before its finalization.
They are Professor Mbendi Nsukini Sébastien from the Department of Internal Medicine, Professors Kalengayi Mbowa Raphaël and Pakasa Muyulu from the Department of Anatomo-Pathology, Professor Mulumba Madishala Paul from the Department of Parasitology.
Declarations of interest:
The authors declare that they have no conflicts of interest.
Funding:
This study received no specific funding from any public, commercial or non-profit agency. All authors certify compliance with the criteria of the International Committee of Medical Journal Editors regarding their contribution to the article.
References:
- Dietrich CG, Götze O, Geier A. Molecular changes in hepatic metabolism and transport in cirrhosis and their functional importance. World J Gastroenterol 22 (2016): 72-88.
- Blachier M, Leleu H, Peck-Radosavljevic M, et al. The burden of liver disease in Europe: a review of available epidemiological data. J Hepatol 58 (2013): 593-608.
- Ferlay J, Shin HR, Bray F, et al, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127 (2010): 2893-2917.
- Verslype C, Rosmorduc O, Rougier P. ESMO Guidelines Working Group. Hepatocellular carcinoma: ESMO-ESDO Clinical Practice Guidelines for diagnosis, treatment and follow-up.Ann Oncol 23 (2012): 41-48.
- Zhang X, Kang C, Li N, et al.Identification of special key genes for alcohol-related hepatocellular carcinoma through bioinformatic analysis. PeerJ 7 (2019): 6375.
- Jang JW. Current status of liver diseases in Korea: Liver cirrhosis. The Korean Journal of Hepatology (2010): 40-49.
- Sivanathan V, Kittner JM, Sprinzl MF, et al. Etiology and complications of liver cirrhosis: data from a German centre.Dtsch Med Wochenschr 139 (2014): 1758-1762.
- Zhou B, Carrillo-Larco RM, Danaei G, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. The Lancet 398 (2021): 957-980.
- Seki E, Brenner DA. Recent advancement of molecular mechanisms of liver fibrosis. J Hepatobiliary Pancreat Sci 22 (2015): 512-518.
- Olave M, Gurung A, Mistry P, et al. Etiology of cirrhosis in the young. Human pathology 96 (2020).
- Mpaka SM, Natuhoyila AN, Tshikwela ML, et al. Liver Cirrhosis Investigation Using Abdominal Ultrasound as Gold Standard Test and Some Bioclinical Markers with Different Levels of Diagnostic Accuracy in Chronic Liver Disease Patients between 1990 and 2004 at Teaching Hospital of Kinshasa, Democratic Republic of the Congo.Open Access Library Journal 8 (2021): 1-15.
- Bahati M. Profile of hepatic pathology observed in ultrasound at Saint Joseph Hospital in Kinshasa. Congo med. (1997): 120-125.
- Djibril M, M'ba B, Bagny A. Nutritional profile of cirrhotics. J Rech Sci Univ Lomé 10 (2008): 45-58.
- Helenon O, Biclet P. Liver Tumor Imaging. 15(2022).
- Somé EN, Guingané NA, Lompo TI, et al. Cirrhosis of the liver: epidemiological and diagnostic aspects at the Yalgado Ouédraogo university hospital center. African Journal of Social Sciences and Public Health 3 (2021): 53-64.
- Nakashima T, Kojiro M. Hepatocellular Carcinoma and Liver Cirrhosis. In: Nakashima T, Kojiro M, editors.Hepatocellular Carcinoma: An Atlas of Its Pathology. 1987. Tokyo. Springer 10 (2020): 185-204.
- Clavière C, Bronowicki JP, Huszrack H, et al. Role of sex steroids and their receptors in the pathophysiology of hepatocellular carcinoma. Gastroenterol clink boil 22 (1998): 73-86.
- Sweets JA. ROC analysis applied to the evaluation of medical imaging techniques. Invest Radiol 47 (1979): 109-121.
- Greiner M, Pfeiffer D, Smith RD. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev Vet Med 45 (2000): 23-41.
- Delacour H, Servonnet A, Perrot A, et al. The ROC curve (receiver operating characteristic): principles and main applications in clinical biology. Ann Biol Clin 63 (2005): 10.
- VR, FC, AH, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology 128 (2005).
- Colloredo G, Guido M, Sonzogni A, et al. Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: the smaller the sample, the milder the disease. J Hepatol 39 (2003): 239-244.
- Bedossa P, Dargère D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 38 (2003): 1449-1457.
- Takayasu K, Moriyama N, Muramatsu Y, et al. The diagnosis of small hepatocellular carcinoma: efficacy of various imaging procedures in 100 patients.AJR Am J Roentgenol 155 (1990): 49-54.
- Sandrin L, Fourquet B, Hasquenoph JM, et al.Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol 29 (2003): 1705-1713.
- Bouglouga O, Lawson-Ananissoh LM, Bagny A, et al. Etiological profile of hepatomegaly at the CHU campus of Lomé (Togo). The Pan African Medical Journal 23 (2016).
- D'Onofrio M, Martone E, Brunelli S, et al.Accuracy of ultrasound in the detection of liver fibrosis in chronic viral hepatitis. Radiol Med 110 (2005): 341-348.
- Yassibanda S, Koffi B, Yangue N. Hepatomegaly at the hospital of the qmitie of Bangui. Mali medical 15 (2004): 1-7.
- Allah Louadio E, Lohoues Kouakou M, Assi C, et al. What indications for hepatic biopsy puncture in 1990-2000 in a medical and hepato-gastroenterology department in an African environment about 57 cases .Rev int Med 2 (2000): 126-132.
- Claudon M, Dietrich CF, Choi BI, et al. Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver - update 2012: A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol 39 (2013): 187-210.
- Ouavene JO, Koffi B, Mobima T, et al. Cirrhosis of the liver at the friendship hospital of Bangui epidemiological, clinical, ultrasound aspects and diagnostic problems. undefined (2014).
- Di Lelio A, Cestari C, Lomazzi A, et al. Cirrhosis: diagnosis with sonographic study of the liver surface.Radiology 172 (1989): 389-392.
