Bilateral Radial Head Fracture with Unilateral Terrible Triad Injury in a Military
Article Information
Mourad Bennani1*, Mouad Guenbdar1, Taoufik Cherrad1, Hassan Zejjari1, Jamal Louaste1, Larbi Amhajji1
1Moulay Ismail Military Hospital, Morocco
*Corresponding Author: Mourad Bennani, Moulay Ismail Military Hospital, Morocco.
Received: 07 October 2022; Accepted: 02 November 2022; Published: 28 February 2023
Citation: Mourad Bennani, Mouad Guenbdar, Taoufik Cherrad, Hassan Zejjari, Jamal Louaste, Larbi Amhajji. Bilateral Radial Head Fracture with Unilateral Terrible Triad Injury in a Military. Archives of Clinical and Medical Case Reports 7 (2023): 89-94.
View / Download Pdf Share at FacebookAbstract
Background: The combination of coronoid process fracture, radial head fracture, and elbow dislocation has earned the moniker “terrible triad” by virtue of its challenging treatment and historically poor outcomes. Bilateral radial head fracture with unilateral terrible triad injury is an unprecedented presentation. It raises questions regarding the mechanism of injury, the surgical indication and the rehabilitation program.
Case Presentation: We report a case of a 29-year-old man presenting a unilateral terrible triad injury of the right elbow and a left radial head fracture after he fell off his motorcycle. The patient underwent open reduction and internal fixation of the radial head with repair of the lateral collateral ligament for the right elbow while the left radial head fracture was treated by a short-term immobilization in a posterior splint. We have reached good results 2 years after the injury: The Mayo Elbow Performance Score was 100 for both elbows.
Conclusion: The few available data suggest that bilateral elbow injury involving a terrible triad occurs mainly in male young patient as a result of a high energy trauma. Bilateral radial head fracture with unilateral terrible triad injury is unprecedented. Well adapted surgical indication followed by optimal rehabilitation program are the two keys to obtain good results.
Keywords
Bilateral Elbow Injury; Mason II Fracture; Rehabilitation Program; Terrible Triad Injury; Treatment Indication
Bilateral Elbow Injury articles; Mason II Fracture articles; Rehabilitation Program articles; Terrible Triad Injury articles; Treatment Indication articles
Bilateral Elbow Injury articles Bilateral Elbow Injury Research articles Bilateral Elbow Injury review articles Bilateral Elbow Injury PubMed articles Bilateral Elbow Injury PubMed Central articles Bilateral Elbow Injury 2023 articles Bilateral Elbow Injury 2024 articles Bilateral Elbow Injury Scopus articles Bilateral Elbow Injury impact factor journals Bilateral Elbow Injury Scopus journals Bilateral Elbow Injury PubMed journals Bilateral Elbow Injury medical journals Bilateral Elbow Injury free journals Bilateral Elbow Injury best journals Bilateral Elbow Injury top journals Bilateral Elbow Injury free medical journals Bilateral Elbow Injury famous journals Bilateral Elbow Injury Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals Covid-19 articles Covid-19 Research articles Covid-19 review articles Covid-19 PubMed articles Covid-19 PubMed Central articles Covid-19 2023 articles Covid-19 2024 articles Covid-19 Scopus articles Covid-19 impact factor journals Covid-19 Scopus journals Covid-19 PubMed journals Covid-19 medical journals Covid-19 free journals Covid-19 best journals Covid-19 top journals Covid-19 free medical journals Covid-19 famous journals Covid-19 Google Scholar indexed journals Mason II Fracture articles Mason II Fracture Research articles Mason II Fracture review articles Mason II Fracture PubMed articles Mason II Fracture PubMed Central articles Mason II Fracture 2023 articles Mason II Fracture 2024 articles Mason II Fracture Scopus articles Mason II Fracture impact factor journals Mason II Fracture Scopus journals Mason II Fracture PubMed journals Mason II Fracture medical journals Mason II Fracture free journals Mason II Fracture best journals Mason II Fracture top journals Mason II Fracture free medical journals Mason II Fracture famous journals Mason II Fracture Google Scholar indexed journals Rehabilitation Program articles Rehabilitation Program Research articles Rehabilitation Program review articles Rehabilitation Program PubMed articles Rehabilitation Program PubMed Central articles Rehabilitation Program 2023 articles Rehabilitation Program 2024 articles Rehabilitation Program Scopus articles Rehabilitation Program impact factor journals Rehabilitation Program Scopus journals Rehabilitation Program PubMed journals Rehabilitation Program medical journals Rehabilitation Program free journals Rehabilitation Program best journals Rehabilitation Program top journals Rehabilitation Program free medical journals Rehabilitation Program famous journals Rehabilitation Program Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Terrible Triad Injury articles Terrible Triad Injury Research articles Terrible Triad Injury review articles Terrible Triad Injury PubMed articles Terrible Triad Injury PubMed Central articles Terrible Triad Injury 2023 articles Terrible Triad Injury 2024 articles Terrible Triad Injury Scopus articles Terrible Triad Injury impact factor journals Terrible Triad Injury Scopus journals Terrible Triad Injury PubMed journals Terrible Triad Injury medical journals Terrible Triad Injury free journals Terrible Triad Injury best journals Terrible Triad Injury top journals Terrible Triad Injury free medical journals Terrible Triad Injury famous journals Terrible Triad Injury Google Scholar indexed journals Thromboelastography articles Thromboelastography Research articles Thromboelastography review articles Thromboelastography PubMed articles Thromboelastography PubMed Central articles Thromboelastography 2023 articles Thromboelastography 2024 articles Thromboelastography Scopus articles Thromboelastography impact factor journals Thromboelastography Scopus journals Thromboelastography PubMed journals Thromboelastography medical journals Thromboelastography free journals Thromboelastography best journals Thromboelastography top journals Thromboelastography free medical journals Thromboelastography famous journals Thromboelastography Google Scholar indexed journals
Article Details
Abbreviations:
CT- Computed Tomography; LCL- Lateral Collateral Ligament; MCL- Medial Collateral Ligament; MEPS- Mayo Elbow Performance Score; ORIF- Open Reduction and Internal Fixation; ROM- Range of Motion
1. Background
Radial head fractures account for 3% of all fractures and approximately 33% of all elbow fractures [1]. A complex elbow dislocation with associated radial head and coronoid process fractures was named the terrible triad by Hotchkiss [2]. This is the first description of a bilateral radial head fracture with unilateral terrible triad. This unprecedented pattern of injury in a high-demanding patient raises high demands on the surgeon’s mastery of the anatomic complexity of the elbow as well as the surgical indications and rehabilitation issues.
2. Case Presentation
A 29-year-old military man, right-handed without medical history fell from his motorbike on a highway and landed on both outstretched hands. He was taken to the emergency room in the local hospital immediately with pain in both elbows and dislocation of the right elbow joint. He underwent manipulative reduction and the elbow was fixed in flexion with plaster. Then he was transferred to our hospital. Physical examination revealed significant swelling with total functional impotence in the right elbow. In the left elbow, clinical findings have shown painful rotation of the forearm, especially with palpation of the radial head without block to forearm rotation or ligamentous instability. In both sides, neurovascular examination was normal, the subtle palpation along the interosseus membrane was painless, and the distal radioulnar joints examination was unremarkable concerning tenderness or instability. Anteroposterior and lateral radiographs of both elbows were performed as well as computed tomography (Figure 1). On the left side, we found a radial head fracture. It was a simple displaced anterolateral fragment less than 30% of the articular surface, which corresponds to a Mason II fracture [3]. The right elbow X ray showed a displaced radial head fracture and a small triangular osseous fragment anterior to the ulnohumeral articulation visible in the lateral radiograph. In the scan: we noted a subluxation of the ulnohumeral articulation, 2 displaced articular fragments of the radial head which matched up with a type II fracture in Mason classification, and a fracture of the coronoid tip which does not extend past the sublime tubercle. It was outlined as a type I fracture in the Regan and Morrey classification [4]. Thus the diagnosis of the terrible triad was made for the right elbow. 24 hours after the injury, the patient was taken to the operating room. The left elbow was aspirated under aseptic precautions and local anaesthetic was injected at the fracture site. Passive motion attained an arc of flexion of 10–140° and 70/80 pronosupination without block or instability. So, we have been content to a conservative treatment with a posterior elbow splint at 90° of flexion and neutral rotation of the forearm. Under general anaesthesia, the right elbow was instable and dislocated at 45–50% of extension. A Kocher approach was used to access to the radial head fracture, which was reduced and fixed by a 2.7 mm screw and a Kirshner pin placed in the “safe zone”. The lateral collateral ligament (LCL) was avulsed from its origin on the lateral epicondyle, so it was reattached with transosseous sutures in 90° of flexion. The elbow was then revaluated and fluoroscopically examined for stability. It remained congruous from 0° to full flexion and no postero-lateral rotatory or valgus instability were noted. We did not fix the coronoid tip fragment. The incision was closed in layers, and a drainage tube was used. After dressing the wound, the right elbow was immobilized in a splint at 90° of flexion, with the forearm in full pronation. Postoperative X-rays showed a good reduction and perfect concentricity of the ulnohumeral and radiocapitellar joints. (Figure 2). The patient was discharged home the next day after he was instructed to use ice and pain medication as needed and given an appointment for rehabilitation. Clinical and radiographic evaluation was performed at 1, 2, 3, 6, 12 and 24 months after discharge. At each follow-up range of motion (ROM) in flexion/extension and supination/pronation was recorded. For the left elbow, active and active-assisted physiotherapy were initiated early after 2 weeks of immobilization. Varus and valgus stresses as well as resistive exercises was authorized after the clinical examination at one month ruled out any instability. For the right elbow, the plaster splint was replaced by a resting splint after 3 weeks with the elbow at 90° of flexion and the forearm in pronation for additional 3 weeks to protect the LCL between exercises. Passive stretching was initiated at 6 weeks and strengthening at 8 weeks. At 6 months follow-up, the patient was pain-free. Full ROM was restored on the left elbow. On the right, we recorded 10° loss of extension and 25° loss of pronosupination (Figure 3). No residual instability was noted on both sides. 2 years after the accident the patient pursues normally his military duty. The Mayo Elbow Performance Score (MEPS) [5] is 100 for both elbows without any radiological signs of osteoarthritis or heterotopic ossification. (Figure 4).
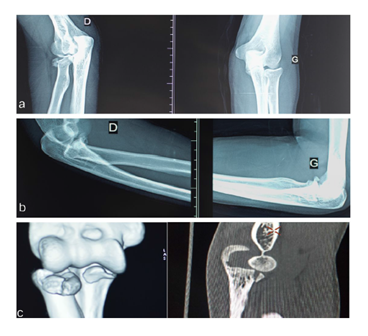
Figure 1: (a,b) frontal and lateral radiographs of the right (D) and left (G) elbows. (G): displaced anterolateral fragment less than 30% of the articular surface. (D): two displaced articular fragments with fracture of the tip of coronoid. (c) Computed tomography of the right elbow.
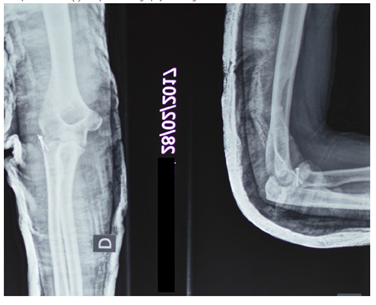
Figure 2: Post-operative radiography of the right elbow.

Figure 3: At 6 months follow-up, full range of motion on the left elbow. On the right elbow: 10° loss of extension and 25° loss of pronosupination.
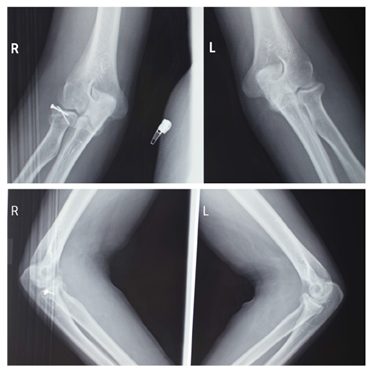
Figure 4: 2 years follow-up, frontal and lateral radiographs of the right (R) and left (L) elbows without signs of osteoarthritis or heterotopic ossifications.
3.Discussion and Conclusions
The elbow consists of bones, ligaments, tendons, and muscles that interact to allow for a stable, pain-free arc of motion. The anatomic features of the elbow that contribute to stability have been examined in various studies and can be divided into two main categories: primary and secondary. The primary stabilizers of the elbow are the ulnohumeral articulation, the medial collateral ligament (MCL), and the LCL. The secondary stabilizers include the radial head, joint capsule, and the common flexor and extensor origins [6]. The radial head provides an important anterior and valgus buttress to the elbow. The LCL functions as an important restraint to varus and posterolateral rotatory instability [7]. The MCL functions as an important restraint to valgus and posteromedial rotatory instability [8]. Beyond 30° of flexion, the coronoid process provides substantial resistance to posterior subluxation or dislocation [9]. Complex elbow dislocation with associated radial head and coronoid process fractures was named the terrible triad by Hotchkiss [2] in 1996 because of historically poor outcomes. In our knowledge, bilateral elbow joint injury involving a terrible triad was reported in three papers. Guoqing Zha et al [10] reported a case of severe injury of bilateral elbow joints with unilateral terrible triad and suspected terrible triad complicated with olecranon fracture in a 26 years male patient. Xiao-Yang Qi et al and Gabriela Soare et al [11, 12] both reported a severe injury of bilateral terrible triad of the elbow respectively in a 34- and 39- years old males.
All The reported cases have in common with ours the gender, the young age of the patients and the high energy trauma. The mechanism of injury for isolated radial head and terrible triad are different. Radial head fracture occurs after falling on outstretched hand with partly flexed elbow and pronated forearm. With the majority of force across the elbow passing through the radiocapitellar joint [13]. The terrible triad injury is also caused by a fall on an outstretched hand, but a posteriorly directed force resulting from the fall on an extended elbow levers the ulna out of the trochlea. O’Driscoll et al [14] postulated that, in a fall with the arm extended, the elbow becomes fixed, and the body produces a valgus and posterolateral rotatory moment. Sequentially, the capsuloligamentous structures of the elbow begin to fail from lateral to medial. The anterior bundle of the MCL is postulated to be the last to fail; therefore, an elbow can theoretically dislocate without a complete tear of this structure. As the elbow slides out of joint, fractures of the radial head and coronoid process frequently occur. We can assume that the injury was more severe in the right elbow because of the right-hand dominance. When falling off his motorcycle, the patient tried to protect his body with the right arm. As the elbow was extended at the impact, the trauma caused it to dislocate. The patient then quickly interposed his left arm while losing height. The rest of the shock wave was absorbed by a left elbow in slight flexion, which caused a radial head fracture. Conventional radiography with antero-posterior and lateral views is usually adequate for detection of radial head fractures. Recent studies have shown that three-dimensional computed tomography imaging improves the characterization of the radial fracture but with less proposed variability in treatment [15]. Radiographs of terrible triad injuries can be deceptive. In some cases, the elbow is reduced and there are small fragments of bone anterior to the ulnohumeral joint on a lateral radiograph and a radial head/neck fracture is noted on the anteroposterior view. The small triangular anterior fragment is a piece of the fractured coronoid tip and is a sign that a more substantial injury has occurred. Lateral radiographs are also used to determine the height of the coronoid fracture; however, the pattern and extent of the fracture are often difficult to characterize on plain radiographs. Computed tomography (CT) with 3D is routinely used in patients with terrible triad injuries to identify fracture patterns, comminution, and displacement, which may not be evident on plain radiographs. Several classifications have been introduced to describe radial head fractures, nearly all derived from the classification introduced by Mason in 1954[3]. The classification distinguishes undisplaced fractures (type I), displaced fractures (type II), and fractures that are displaced with comminution (type III). But Mason did not define or quantify displacement. Broberg and Morrey modified Mason classification [16], quantifying displacement as 2 mm or greater articular step-off or gap, and indicating that fracture fragments representing less than 30% of the articular surface should not be considered type II but type I. Two classification systems outline the fracture patterns seen in coronoid process injuries. The first, proposed by Regan and Morrey [4], was based on the height of the coronoid fragment. A type I fracture involved an “avulsion” of the tip of the coronoid process, type II involved a single or comminuted fracture representing ≤ 50% of the coronoid process, and type III involved a single or comminuted fracture of > 50% of the coronoid. A second classification scheme was recently reported by O’Driscoll et al [17] and is based on the location of the fracture in reference to local anatomy. The classification divides the coronoid process into the tip, the anteromedial facet, and the base. Tip fractures are most frequently seen in association with terrible triad injuries. They do not usually extend past the sublime tubercle; therefore, the ulnar attachment site of the MCL is usually intact [18]. The major goal of treatment of radial head fractures is to allow early range of motion in an effort to prevent stiffness. Whether Mason II fractures need open reduction and internal fixation (ORIF) is controversial. Good results with few complications are usually achieved with ORIF of partially displaced fractures of the radial head. However, since Akesson and colleagues [19] first reported good long-term results of nonsurgically treated 2 to 5 mm displaced Mason II fractures, the indication for surgery is again in question. Furthermore, the same author reported that most of the degenerative changes remained asymptomatic.
Morrey and colleagues [20] have found the aspiration of the joint with injection of local anesthetic of value to determine whether a minimally displaced fracture is amenable to nonoperative management. Gentle passive motion should attain an arc of flexion of 10 to 130 degrees, and 70/70 pronosupination to proceed with nonoperative treatment. In the light of the above, we recommended the conservative treatment to our patient. The purposes of treatment of the terrible triad is to recover the congruency of the elbow joint, restore stability, and allow early joint mobility to avoid complications. Patients with a stable elbow after reduction may be considered for nonsurgical treatment, but stability and final elbow function after nonsurgical treatment may not be predictable. The nonsurgical treatment plan requires that imaging show a small nondisplaced or minimally displaced radial head or neck fracture that does not cause a mechanical block to forearm rotation or elbow flexion/extension. The coronoid fracture must also be a small tip fragment as confirmed by CT scans. Most terrible triad elbow injuries are managed surgically. The best surgical protocol to treat terrible triad injuries of the elbow remains unclear but a general consensus exists that the primary goal of surgery is to re-establish sufficient stability of the joint to permit early mobilization. Radial head fracture fixation versus replacement is dictated in part by the number and character of the fracture fragments. Fixation of radial head fractures with more than 3 parts (shaft and 2 articular fragments) is prone to early failure of fixation, nonunion, and limited forearm rotation when the fracture heals [21]. There is consensus that the LCL origin should be reattached to the lateral epicondyle in all elbow injuries; however, there continues to be some debate as to whether or not the MCL should be reattached to the medial epicondyle. Pugh et al [22] described an algorithm used in 34 patients in which the MCL was repaired if there was residual instability after addressing the coronoid, radial head, and lateral collateral ligament. We did not fix the coronoid fragment; debate still exists regarding best treatment of small or much comminute coronoid fragments. In a cohort level IV study, 14 consecutive patients with acute terrible triad injuries that included two Regan-Morrey type I and 12 Regan-Morrey type II coronoid fractures were treated by Loukia et al [23] with a surgical protocol that included radial head repair or prosthetic replacement and repair of the LCL followed by intraoperative fluoroscopic examination through a range of 20° to 130° of elbow flexion to confirm concentric reduction of the ulnohumeral joint. Using this protocol, intraoperative stability was confirmed in all cases without any attempt at coronoid or anterior capsular repair. The results of this study suggested that terrible triad injuries can be successfully managed without fixation of Regan-Morrey type I and II coronoid fractures if the radial head and LCL are addressed. Randomised-controlled trials should be conducted to determine optimal management strategies. Various approaches have been reported to treat the terrible triad of the elbow. The posterior approach is advocated in most literature because both the medial and lateral sides of the elbow can be exposed with a lower risk of injury to the cutaneous nerves compared with medial and lateral incisions [18]. However, this approach has some deficiencies such as long skin incision, wide dissection, severe soft tissue damage, and the risk of hematoma formation, heterotopic ossification, even flap necrosis [21]. Factors in selecting an approach include fracture and instability pattern, soft-tissue injury, and surgeon experience. We chose a lateral deep approach (Kocher approach) to access to the radial head and the disrupted LCL. The elbow is an unforgiving articulation with significant bony congruity and a tendency to develop inflammation and stiffness [24].
Rehabilitation of bilateral asymmetric elbow injury in a military young man is a great challenge. It may accentuate therapeutic pertinences as well pitfalls. Bilateral immobilisation made day-to-day activities difficult if not impossible. So, familial help is obligatory especially in the early post-operative period. Rehabilitation must be initiated early and should progress in parallel for both elbow keeping in mind that the rehabilitation program after surgical treatment of a terrible triad differ largely from that in isolated stable radial head fracture. With nonoperative simple type II radial head fractures, a very short immobilization period of up to a week is recommended. Early active / active assisted ROM helps to prevent stiffness, brawny oedema, and adhesion formation of the capsule and annular ligament as well as promote healing and increase tensile strength of the involved bony and soft tissue structures [25]. Passive stretching and strengthening can be initiated at 4 to 6 weeks. In the terrible triad injury, the effort to restore ranges of motion should not compromise the elbow stability. So, rehabilitation program depends on the stability of the elbow following the completion of the surgical procedure. In patient with LCL insufficient and MCL intact elbow. We must avoid varus positioning of the arm in the first 6 weeks. Active assisted motion is encouraged while passive motion is avoided. Rotation of the forearm should be performed in flexion and the elbow extended in pronation. We begin passive stretching and strengthening at 6 weeks. For a military, it would be of the most importance to complete by a work-hardening program before regaining his duty. Elbow full range of motion is not essential for performance of all the activities of daily living. The functional arc of flexion and extension used in performing most daily activities is 30° to 130°, and 50° of pronation and supination are required to perform 90% of daily activities [26]. However, some daily activities (e.g., reaching to the opposite side of the head), as well as many recreational and vocational activities, may require greater motion [27]. Moreover, we firmly believe that even a minor functional limitation in one elbow can lead to significant global disability in the daily living of a military.
Declarations
Ethical Approval and Consent to Participate
Not applicable.
Consent for Publication
A written informed consent for publication was obtained.
Availability of Supporting Data
All data generated or analysed during this study are included in this published article and its supplementary information files.
Competing Interests
The authors declare that they have no competing interests.
Funding
None of the authors of the manuscript receive funding, grants, or in-kind support in support of the research or the preparation of the manuscript.
Authors’ Contributions
Mourad Bennani- Conceptualization. Writing - Original Draft. Taoufik Cherrad- Writing - Review & Editing. Mouad Guenbdar- Visualization. Hassan Zejjari- Resources. Jamal Louaste- Visualization. Larbi Amhajji- Supervision.
Acknowledgements
Not applicable.
References
- Lapner M, King GJ. Radial head fractures. J Bone Joint Surg 95A (2013): 1136.
- Hotchkiss RN. Fractures and dislocations of the elbow, in Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD (eds): Rockwood and Green’s Fractures in Adults, ed 4. Philadelphia, PA: Lippincott-Raven 1 (1996): 929-1024.
- Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg 42 (1954): 123-132.
- Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71 (1989): 1348-1354.
- Morrey BF, An KN, Chao EYS. Functional evaluation of the elbow. In: Morrey BF, ed. The Elbow and Its Disorders. 2nd ed. Philadelphia, PA: WB Saunders Co (1993): 95.
- O’Driscoll SW, Jupiter JB, King GJ, et al. The unstable elbow. Instr Course Lect 50 (2001): 89-102.
- Dunning CE, Zarzour ZD, Patterson SD, et al. Ligamentous stabilizers against posterolateral rotatory instability of the elbow. J Bone Joint Surg Am 83 (2001): 1823-1828.
- Pichora JE, Fraser GS, Ferreira LF, et al. Theeffect of medial collateral ligament repairtension on elbow joint kinematics andstability. J Hand Surg [Am] 32 (2007): 1210-1217.
- Mezera K, Hotchkiss RN. Fractures and dislocations of the elbow, in Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD (eds): Rockwood and Green’s Fractures in Adults, ed 5. Philadelphia, PA: Lippincott-Raven (2001): 921-952.
- Guoqing Z, Xiaofeng N, Weiguang Y, et al. Severe injury of bilateral elbow joints with unilateral terrible triad of the elbow and unilateral suspected terrible triad of the elbow complicated with olecranon fracture: one case report. Int J Clin Exp Med 8 (2015): 14214-14220.
- Gabriela S, Cosmin CB, Gheorghe IP, et al. Bilateral terrible triad injury of the elbow – a case report. Romanian Journal of Emergency Surgery 1 (2019): 1.
- Xiao-Yang Q, Xu-Sheng Q, Yi-Xin C. Severe injury of bilateral terrible triad of the elbow joints: a case report. Int J Clin Exp Med 11 (2018): 10021-10028.
- McGinley JC, Hopgood BC, Gaughan JP, et al. Forearm and elbow injury: the influence of rotational position. J Bone Joint Surg 85A:2403, 2003.
- O’Driscoll SW, Morrey BF, Korinek S, An KN: Elbow subluxation and dislocation: A spectrum of instability. Clin Orthop Relat Res 280 (1992): 186-187.
- Guitton TG, Brouwer K, Lindenhovius ALC, et al. Diagnostic accuracy of two-dimensional and threedimensional imaging and modeling of radial head fractures. J Hand Microsurg 6 (2014): 13.
- Broberg MA, Morrey BF. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res (1987): 109-119.
- O’Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: Pearls and pitfalls. Instr Course Lect 52 (2003): 113-134.
- Mathew PK, Athwal GS, King GJ. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg 17 (2009): 137-151.
- Akesson T, Herbertsson P, Josefsson PO, et al. Primary nonoperative treatment of moderately displaced two-part fractures of the radial head. J Bone Joint Surg Am 88 (2006): 1909-1914.
- Antuña S, Alvarez EDT, Barco R, et al. Radial Head Fracture: General Considerations, Conservative Treatment, and Radial Head Resection. Morrey's the Elbow and its Disorders (Fifth Edition) (2018): 375-387.
- Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am 84 (2002): 1811e1815.
- Pugh DM, Wild LM, Schemitsch EH, et al. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am 86 (2004): 1122e1130.
- Papatheodorou LK, Rubright JH, Heim KA, et al. Terrible Triad Injuries of the Elbow: Does the Coronoid Always Need to Be Fixed? Clin Orthop Relat Res 472 (2014): 2084-2091.
- Morrey B. The posttraumatic stiff elbow. Clin Orthop Rel Res 431 (2005): 26.
- King GJW. Fracture of the head of radius. In: Green DP, et al (ed). Green’s Operative Hand Surgery, Vol. 1. 5th ed. Philadelphia, PA: Elsevier Churchill Livingston (2005): 845-887.
- Regan WD, Morrey BF. Physical examination of the elbow. In: Morrey BF, Sanches-Sotelo J, eds. The elbow and its disorders. 4th ed. Philadelphia: Saunders-Elsevier (2009): 67-79.
- Morrey B, Askew L, Chaoi E. A biomechanical study of normal functional elbow motion. J Bone Joint Surg 63 (1981): 872.
