Bilateral Fracture Femur in a Patient with Renal Tubular Acidosis -Type 1 (Osteopetrosis Type) Platting or Nailing? A Case Report
Article Information
Atef Ibrahim Awad1*, Waleed Meligy2, Ehab Elshal3, Hany Elhalafawy4, Elsayed Elhamy Negm5
1Consultant of orthopaedics at AFHSR, Khamis Mushait, Saudi Arabia
2Specialist of orthopaedics AFHSR Khamis Mushait, Saudi Arabia
3Assistant professor of orthopaedics, Alazhar University, Assuit, Egypt
4Specialist orthopedic surgery at UAE, Cairo University, Egypt
5Lecturer of Orthopaedics, Faculty of Medicine, Tanta University, Egypt
*Corresponding Author:Atef Ibrahim Awad, Consultant of orthopaedics at AFHSR, Khamis Mushait, Saudi Arabia.
Received: September 13, 2023;Accepted: September 22, 2023; Published: September 29, 2023
Citation: Atef Ibrahim Awad, Waleed Meligy, Ehab Elshal, Hany Elhalafawy, Elsayed Elhamy Negm. Bilateral Fracture Femur in a Patient with Renal Tubular Acidosis -Type 1 (Osteopetrosis Type) Platting or Nailing? A Case Report. Journal of Orthopedics and Sports Medicine. 5 (2023): 388-390.
View / Download Pdf Share at FacebookAbstract
Diaphyseal Renal tubular is an uncommon medical disorder that comprises four variant types. It affects the skeletal system in different ways, most commonly osteomalacia and rarely osteopetrosis. Renal tubular acidosis with bone disease is representing a challenge to orthopaedic surgeon when facing fracture fixation which is more obvious in osteopetrotic bone disease. Our case represents bilateral femoral shaft fracture that had been fixed by two different surgeons with 2 different ways of fixation (weight bearing versus load sharing implants).
Keywords
Renal tubular acidosis; Fracture femur; Osteopetrosis; Plate; IM Nail
Osteopetrosis articles Osteopetrosis Research articles Osteopetrosis review articles Osteopetrosis PubMed articles Osteopetrosis PubMed Central articles Osteopetrosis 2023 articles Osteopetrosis 2024 articles Osteopetrosis Scopus articles Osteopetrosis impact factor journals Osteopetrosis Scopus journals Osteopetrosis PubMed journals Osteopetrosis medical journals Osteopetrosis free journals Osteopetrosis best journals Osteopetrosis top journals Osteopetrosis free medical journals Osteopetrosis famous journals Osteopetrosis Google Scholar indexed journals Renal tubular acidosis articles Renal tubular acidosis Research articles Renal tubular acidosis review articles Renal tubular acidosis PubMed articles Renal tubular acidosis PubMed Central articles Renal tubular acidosis 2023 articles Renal tubular acidosis 2024 articles Renal tubular acidosis Scopus articles Renal tubular acidosis impact factor journals Renal tubular acidosis Scopus journals Renal tubular acidosis PubMed journals Renal tubular acidosis medical journals Renal tubular acidosis free journals Renal tubular acidosis best journals Renal tubular acidosis top journals Renal tubular acidosis free medical journals Renal tubular acidosis famous journals Renal tubular acidosis Google Scholar indexed journals Osteopetrotic bone articles Osteopetrotic bone Research articles Osteopetrotic bone review articles Osteopetrotic bone PubMed articles Osteopetrotic bone PubMed Central articles Osteopetrotic bone 2023 articles Osteopetrotic bone 2024 articles Osteopetrotic bone Scopus articles Osteopetrotic bone impact factor journals Osteopetrotic bone Scopus journals Osteopetrotic bone PubMed journals Osteopetrotic bone medical journals Osteopetrotic bone free journals Osteopetrotic bone best journals Osteopetrotic bone top journals Osteopetrotic bone free medical journals Osteopetrotic bone famous journals Osteopetrotic bone Google Scholar indexed journals Orthopedic surgery articles Orthopedic surgery Research articles Orthopedic surgery review articles Orthopedic surgery PubMed articles Orthopedic surgery PubMed Central articles Orthopedic surgery 2023 articles Orthopedic surgery 2024 articles Orthopedic surgery Scopus articles Orthopedic surgery impact factor journals Orthopedic surgery Scopus journals Orthopedic surgery PubMed journals Orthopedic surgery medical journals Orthopedic surgery free journals Orthopedic surgery best journals Orthopedic surgery top journals Orthopedic surgery free medical journals Orthopedic surgery famous journals Orthopedic surgery Google Scholar indexed journals Bone diseases articles Bone diseases Research articles Bone diseases review articles Bone diseases PubMed articles Bone diseases PubMed Central articles Bone diseases 2023 articles Bone diseases 2024 articles Bone diseases Scopus articles Bone diseases impact factor journals Bone diseases Scopus journals Bone diseases PubMed journals Bone diseases medical journals Bone diseases free journals Bone diseases best journals Bone diseases top journals Bone diseases free medical journals Bone diseases famous journals Bone diseases Google Scholar indexed journals Osteopetrotic bone articles Osteopetrotic bone Research articles Osteopetrotic bone review articles Osteopetrotic bone PubMed articles Osteopetrotic bone PubMed Central articles Osteopetrotic bone 2023 articles Osteopetrotic bone 2024 articles Osteopetrotic bone Scopus articles Osteopetrotic bone impact factor journals Osteopetrotic bone Scopus journals Osteopetrotic bone PubMed journals Osteopetrotic bone medical journals Osteopetrotic bone free journals Osteopetrotic bone best journals Osteopetrotic bone top journals Osteopetrotic bone free medical journals Osteopetrotic bone famous journals Osteopetrotic bone Google Scholar indexed journals Tubular defects articles Tubular defects Research articles Tubular defects review articles Tubular defects PubMed articles Tubular defects PubMed Central articles Tubular defects 2023 articles Tubular defects 2024 articles Tubular defects Scopus articles Tubular defects impact factor journals Tubular defects Scopus journals Tubular defects PubMed journals Tubular defects medical journals Tubular defects free journals Tubular defects best journals Tubular defects top journals Tubular defects free medical journals Tubular defects famous journals Tubular defects Google Scholar indexed journals Kidney disease articles Kidney disease Research articles Kidney disease review articles Kidney disease PubMed articles Kidney disease PubMed Central articles Kidney disease 2023 articles Kidney disease 2024 articles Kidney disease Scopus articles Kidney disease impact factor journals Kidney disease Scopus journals Kidney disease PubMed journals Kidney disease medical journals Kidney disease free journals Kidney disease best journals Kidney disease top journals Kidney disease free medical journals Kidney disease famous journals Kidney disease Google Scholar indexed journals
Article Details
Introduction
Renal tubular acidosis (RTA) occurs when the kidneys are unable to maintain normal acid-base homeostasis because of tubular defects in acid excretion or bicarbonate ion reabsorption [1]. RTA can happen at any age, although it is more commonly seen in adults [2]. The three major forms of RTA are distal RTA (type 1; characterized by impaired acid excretion), proximal RTA (type 2; caused by defects in reabsorption of filtered bicarbonate), and hyperkalemic RTA (type 4; caused by abnormal excretion of acid and potassium in the collecting duct). Type 3 RTA is a rare form of the disease with features of both distal and proximal RTA [1]. Untreated type 1 RTA causes children to grow more slowly and adults to develop progressive kidney disease and bone diseases [3]. The association between renal tubular acidosis (RTA) and osteopetrosis has been reported in literature [4].
Case presentation
Female patient 33 years old, known to have type 1 Renal tubular acidosis being followed up by nephrologists, presented to us by closed fracture of right femoral shaft that had been managed by open reduction and internal fixation using a locked broad DCP (Figure 1,2) [5-8].
Two years later, patient presented with closed fracture of left femoral shaft managed by open reduction and internal fixation with locked intramedullary nail (Figure 3).
Both fractures healed completely, 18 months after plate fixation of the right femur and 8 months following nail fixation of the left femur (Figure 4,5).

Figure 1: Preoperative and 3-month postoperative x rays of Right Femur.

Figure 2: Serial postoperative x-rays of the Right femur at 12 Months, and 18 Months.

Figure 3: Preoperative x-rays of the Left femur.
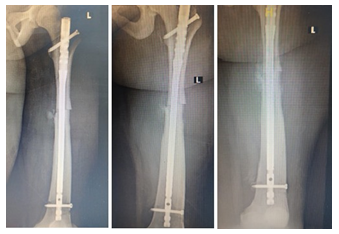
Figure 4: follow up x-rays of the Left Femur.

Figure 5: Final x-rays of the Left Femur showed complete fracture union after 8 months.
Discussion
Renal tubular acidosis (RTA) comprises a group of disorders in which excretion of hydrogen ions or reabsorption of filtered HCO3 is impaired, leading to chronic metabolic acidosis [9].
The most common type of RTA, Type 1 RTA or Distal RTA (dRTA), which is a rare chronic genetic disorder characterized by an inability of the distal nephron to secrete hydrogen ions in the presence of metabolic acidosis [9].
The association between renal tubular acidosis (RTA) and
osteopetrosis has been reported in literature [4-8].
Our case is known RTA type 1 with osteopetrotic bony changes that can be appreciated by thick cortices, narrow medullary canals of long bones, transverse fracture patterns, acromegaly, anaemia and hearing deficit.
In our case, the right femoral shaft fracture, the first surgeon tried to fix the fracture with locked intramedullary nail as the medullary canal was not fully obliterated as in the full blown picture of marble bone disease with no medullary canal. He faced challenges in entry point to find a way to the medullary canal then he changed his decision to open reduction and internal fixation with platting (locked broad DCP).
This type of fixation was not the proper one as per the biomechanical principles of locked plate fixation of long bones being stiff and achieving absolute stability not following the rules of plate span ratio, plate screw density. Eventually full union happened after 18 months.
Chhabra et al. [10] found relatively more failure of load-bearing implants and summarized two primary factors attributed to failure regardless of treatment approach: one is the increased mechanical demands placed on implants because of the prolonged time to union, the other is the biochemical inability of osteopetrotic bone to hold the screws securely.
In the second fracture that happened 2 years later, the second surgeon planned to do locked intramedullary nail and faced complete obliteration of the medullary canal at the isthmus then he opened the fracture site and did retrograde reaming creating the medullary canal. The distal part of the femur had a near normal medullary canal. The second fracture fully united after 8 months.
Conclusion
Renal tubular acidosis with osteopetrotic bone changes is a challenging orthopaedic condition especially when facing long bone fracture fixation.
Although intramedullary fixation or plate fixation, both are troublesome and the fracture fixed by both techniques unites eventually, but a clear difference in time of union between both techniques is clinically observed even with open intramedullary nailing.
Conflict of Interest:
Authors did not have any conflict of interest.
References
- Palmer BF, Kelepouris E, Clegg DJ. Renal Tubular Acidosis and Management Strategies: A Narrative Review. Adv Ther 38(2021): 949-968.
- Giglio S, Montini G, Trepiccione F, et al. Distal renal tubular acidosis: a systematic approach from diagnosis to treatment. J Nephrol 34 (2021): 2073-2083.
- National Organization for Rare Diseases: Rare Diseases Database. Primary distal renal tubular acidosis (2020).
- Ohlsson A, Stark G, Sakati N. Marble brain disease: recessive osteopetrosis, renal tubular acidosis and cerebral calcification in three Saudi Arabian families. Dev Med Child Neurol 22 (1980): 72-84.
- Ballet JJ, Griscelli C, Coutris C, et al. Bone-marrow transplantation in osteopetrosis. Lancet 2 (1977): 1137.
- Guibaud P, Larbre F, Freycon MT, et al. Ostéopétrose et acidose rénale tubulaire. Deux cas de cette association dans une fratrie [Osteopetrosis and renal tubular 2 cases of this association in a sibship]. Arch Fr Pediatr 29 (1972): 269-286.
- Vainsel M, Fondu P, Cadranel S, et al. Osteopetrosis associated with proximal and distal tubular Acta Paediatr Scand 61 (1972): 429-434.
- Whyte MP, Murphy WA, Fallon MD, et Osteopetrosis, renal tubular acidosis and basal ganglia calcification in three sisters. Am J Med 69 (1980): 64-74.
- Giglio S, Montini G, Trepiccione F, et al. Distal renal tubular acidosis: a systematic approach from diagnosis to treatment. J Nephrol 34 (2021): 2073-2083.
- Chhabra A, Westerlund L, Kline A, et al. Management of proximal femoral shaft fractures in osteopetrosis: a case series using internal Orthopedics 28 (2005): 587-592.
