Bilateral DVTs in Hemophilia A, A Case Not Anticoagulated
Article Information
Clarke TR1*, Moas L2
1Assistant Professor of Clinical Medicine, Division of Hospital Medicine and UHealth International Department of Medicine, University of Miami, Miller School of Medicine, Florida, United States
2Medical Student, University of Miami, Miller School of Medicine, Florida, United States
*Corresponding author: Tanya Roxanne Clarke, Assistant Professor of Clinical Medicine, Division of Hospital Medicine and UHealth International Department of Medicine, University of Miami, Miller School of Medicine, Florida, United States
Received: 09 June 2022; Accepted: 17 June 2022; Published: 13 August 2022
Citation: Clarke TR, Moas L. Bilateral DVTs in Hemophilia A, A Case Not Anticoagulated. Archives of Internal Medicine Research 5 (2022): 428-430.
View / Download Pdf Share at FacebookAbstract
A male in his early twenties, who participates in mixed martial arts (MMA) fighting with a past medical history of Hemophilia A but otherwise healthy, presented to the emergency room with a chief complaint of a two-day history of right lower extremity swelling, limiting his ability to walk. Of note, the patient had been self-administering recombinant Factor VIII (FVIII) for 12 years. His most recent self-injection had been the night before the onset of swelling and pain. On examination, his right calf was 2 inches in diameter wider than the left. Bilateral lower extremity venous doppler ultrasounds revealed bilateral acute non-obstructing popliteal vein thromboses.
Keywords
DVT
Article Details
1. Background
Hemophilia A is a clotting disorder inherited in X-linked recessive fashion, characterized by lack of Factor VIII of the clotting cascade. Patients who are affected have prolonged partial thromboplastin time (PTT). Most cases present in childhood with easy bruising/bleeding, as seen in this patient, who was diagnosed due to bleeding complications from a perinatal circumcision. The diagnosis of deep vein thrombosis (DVT) in a patient with Hemophilia A is an unusual occurrence: upon reviewing the literature, we found twelve cases of DVTs reported in patients with this disorder. In patients with Hemophilia A who also take Factor VIII, the risk of DVT due to factor replacement has been found to be equal to the regular population’s baseline risk.
In this case, self-administration of FVIII was deemed unlikely to have contributed in any meaningful way to this patient’s presentation. In general, treatment guidelines maintain that hemophilia is a contraindication to anticoagulant therapy, but evidence-based guidelines do not exist regarding treatment of thrombosis [1]. Cited reasons for these DVTs include concomitant mutations in prothrombin. Other mechanisms put forward include inherited mutations in the methylenetetrahydrofolate reductase (MTHFR) gene, but no significant association has been found between the resultant hyperhomocystinemia and venous thrombosis [1].
1.1 Objective
The objective of this case report was to present a very unusual clinical paradox. Acute thrombosis in the setting of Hemophilia A. There are only few reported cases of this.
2. Case Report
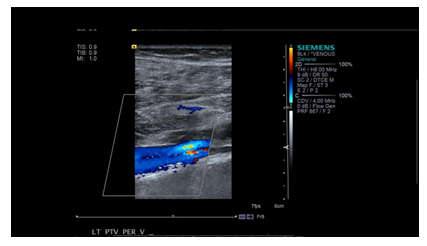
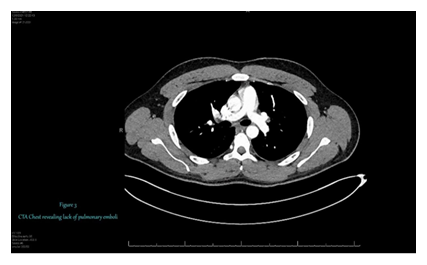
A male in his early twenties, who participates in mixed martial arts (MMA) fighting with a past medical history of Hemophilia A, otherwise healthy, presented to the Emergency room with a chief complaint of a two-day history of right lower extremity swelling, limiting his ability to walk. Of note, the patient had been self-administering recombinant Factor VIII (FVIII) every four days for 12 years. His most recent self-injection had been the night before the onset of swelling and pain. On examination, his right calf was 2 inches wider in diameter than the left calf. Bilateral lower extremity venous doppler ultrasounds revealed bilateral, acute, non- obstructing popliteal vein thromboses. Left popliteal vein DVT, [Figure 1], & Right popliteal vein DVT, [Figure 2]. CT angiogram of his chest was negative for any pulmonary emboli, [Figure 3]. Patient was managed initially with therapeutic Enoxaparin.
His history consisted of a job involving long hours seated in an office, at which he regularly had his legs elevated on another chair for comfort. He denied any long travel or periods of immobilization. This patient was found to have no traditional risk factors that might have contributed to his DVTs. His only evident risk was his MMA and wrestling practice. He has not had any known major trauma in the past, either due to his fighting hobby or otherwise. The patient did state that he primarily used his right leg for blocking and kicking, which, in the non-competitive environment he practiced in, were always guarded with padding. He had no surgery in the past. He stated he smokes marijuana 1-2 times per day, and his drinking habits consist of no more than 1 drink per week. Laboratory data collected included: Factor VIII Activity (Table1), Routine Coagulation Profile (Table 2), Anti-Cardiolipin Antibodies and Basic Metabolic Panel.
The patient was managed initially with therapeutic Enoxaparin. He continued his recombinant Factor VIII (FVIII) on his prescribed schedule of every four days. After 72 hours, a joint consensus with the hematologist was to discharge him home after 96 hours, without anticoagulation and with strict instructions to desist from his practice of MMA and wrestling and to follow up with his Hematologist. The mechanism behind the DVTs was theorized to be due to vascular injury resulting from his MMA and wrestling. The risk of anticoagulation with no clear mutation or laboratory premise was thought to present an elevated risk of bleeding.
|
Ref Range & Units .54 – 1.55 U/mL |
Day 1 |
Day 2 |
Day 3 |
Day 4 |
|
Factor VIII Activity |
3.00 ▲ |
1.27 |
.73 |
0.02 ▼ |
Table 1: Factor VIII Activity.
|
Routine Coagulation |
Day1 |
Day 2 |
Day 3 |
Day 4 |
|
PT |
13.4 |
13.7 |
13.6 |
|
|
POC INR |
1.0 |
1.1 |
1.1 |
|
|
APTT |
61.4 ▲ |
54.8 ▲ |
56.9 ▲ |
36.9 ▲ |
|
Fibrinogen Level |
601 ▲ |
|||
|
D-Dimer Quantitative |
.7 ▲ |
Table 2: Routine Coagulation Panel.
3. Discussion
Hemophilia A is a clotting disorder inherited in X-linked recessive fashion, characterized by lack of Factor VIII of the clotting cascade. Patients who are affected have prolonged partial thromboplastin time (PTT). Most cases present in childhood with easy bruising/bleeding, as seen in this patient, who was diagnosed due to bleeding complications from a perinatal circumcision. The diagnosis of deep vein thrombosis (DVT) in a patient with Hemophilia A is an unusual occurrence: upon reviewing the literature, we found twelve cases of DVTs reported in patients with this disorder. In patients with Hemophilia A who also take Factor VIII, the risk of DVT due to factor replacement has been found to be equal to the regular population’s baseline risk.
In this case, self-administration of FVIII was deemed unlikely to have contributed in any meaningful way to this patient’s presentation. In general, treatment guidelines maintain that hemophilia is a contraindication to anticoagulant therapy, but evidence-based guidelines do not exist regarding treatment of thrombosis [1]. Cited reasons for these DVTs include concomitant mutations in prothrombin. Other mechanisms put forward include inherited mutations in the methylenetetrahydrofolate reductase (MTHFR) gene, but no significant association has been found between the resultant hyperhomocystinemia and venous thrombosis [1].
In this patient, the underlying mechanism of injury remains unclear. His high Factor VII level on Hospital Day one seems to be the most likely cause. Chronic trauma due to his exercise habits was the best explanation on hand without extensive genetic testing results – which still may have left the pathophysiology unclear. His presentation was largely unusual due to his lack of risk factors seen in other patients of a similar group: those who traditionally have some sort of insult or disposition to thromboses [1]. His Factor VIII level was elevated on admission, this could paradoxically make him hypercoagulable.
A review of the literature yielded very little information on patients with Hemophilia A experiencing DVT. No more than 13 cases have been reported in the literature as of 12/2021, [1]. Several reports are characterized by recent injection of recombinant FVIII. Dargaud et al. reported a similar presentation in absence of anti-hemophilic treatment [1]. Of these cases, at least 3 were treated with anticoagulation, including enoxaparin, heparin, and warfarin, [1-4]. Given the paucity of cases to base clinical decision making on, the general contraindication of anticoagulation in hemophiliac patients was overridden for a short period, before anticoagulation was discontinued for discharge.
References
- Martin K, Key NS. How I treat patients with inherited bleeding disorders who need anticoagulant therapy. Blood 128 (2016): 178-184.
- Bezemer ID, Doggen CJM, Vos HL, et al. No association between the common MTHFR 677C→T polymorphism and venous thrombosis: Results from the MEGA study. Arch Intern Med 167 (2007): 497-501.
- Kreidy R, Salameh P, Waked M. Lower extremity venous thrombosis in patients younger than 50 years of age. Vasc Health Risk Manag 8 (2012): 161-167.
- Girolami A, Scandellari R, Zanon E, et al. Non-catheter associated venous thrombosis in hemophilia A and B. A critical review of all reported cases. J Thromb Thrombolysis 21 (2006): 279-284.