Bilateral Breast Cancer in a 65-Year-Old Man
Article Information
Arman Sharbatdaran1*, Mohammed Twam1, Novin Nikbakhsh2, Hosseine Ghorbane2
1St. George’s University School of Medicine, Grenada
2Babol University of Medical Sciences, Babol, Iran
*Corresponding Author: Arman Sharbatdaran, St. George’s University School of Medicine, Grenada
Received: 13 February 2022; Accepted: 24 February 2022; Published: 28 February 2022
Citation: Arman Sharbatdaran, Mohammed Twam, Novin Nikbakhsh, Hosseine Ghorbane. Bilateral Breast Cancer in a 65-Year-Old Man. Archives of Clinical and Medical Case Reports 6 (2022): 116-122.
View / Download Pdf Share at FacebookAbstract
Globally, breast cancer in men is exceedingly uncommon. The misinterpretation of signs and symptoms and lack of a proper medical history can lead to the progression of rare conditions to advanced stages. We report the case of a 65-year-old man who presented to the clinic complaining about progressive bilateral dull breast pain. He had been diagnosed with bilateral grade II invasive ductal carcinoma three months prior, and he underwent bilateral mastectomy followed by chemotherapy as a part of his treatment plan.
Keywords
Male breast cancer; Pathology, Radiology; Bilateral, physical exam; History of presenting illness
Male breast cancer articles; Pathology articles, Radiology articles; Bilateral articles, physical exam articles; History of presenting illness articles
Male breast cancer articles Male breast cancer Research articles Male breast cancer review articles Male breast cancer PubMed articles Male breast cancer PubMed Central articles Male breast cancer 2023 articles Male breast cancer 2024 articles Male breast cancer Scopus articles Male breast cancer impact factor journals Male breast cancer Scopus journals Male breast cancer PubMed journals Male breast cancer medical journals Male breast cancer free journals Male breast cancer best journals Male breast cancer top journals Male breast cancer free medical journals Male breast cancer famous journals Male breast cancer Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals cancer articles cancer Research articles cancer review articles cancer PubMed articles cancer PubMed Central articles cancer 2023 articles cancer 2024 articles cancer Scopus articles cancer impact factor journals cancer Scopus journals cancer PubMed journals cancer medical journals cancer free journals cancer best journals cancer top journals cancer free medical journals cancer famous journals cancer Google Scholar indexed journals Pathology articles Pathology Research articles Pathology review articles Pathology PubMed articles Pathology PubMed Central articles Pathology 2023 articles Pathology 2024 articles Pathology Scopus articles Pathology impact factor journals Pathology Scopus journals Pathology PubMed journals Pathology medical journals Pathology free journals Pathology best journals Pathology top journals Pathology free medical journals Pathology famous journals Pathology Google Scholar indexed journals Ultra Sound articles Ultra Sound Research articles Ultra Sound review articles Ultra Sound PubMed articles Ultra Sound PubMed Central articles Ultra Sound 2023 articles Ultra Sound 2024 articles Ultra Sound Scopus articles Ultra Sound impact factor journals Ultra Sound Scopus journals Ultra Sound PubMed journals Ultra Sound medical journals Ultra Sound free journals Ultra Sound best journals Ultra Sound top journals Ultra Sound free medical journals Ultra Sound famous journals Ultra Sound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Radiology articles Radiology Research articles Radiology review articles Radiology PubMed articles Radiology PubMed Central articles Radiology 2023 articles Radiology 2024 articles Radiology Scopus articles Radiology impact factor journals Radiology Scopus journals Radiology PubMed journals Radiology medical journals Radiology free journals Radiology best journals Radiology top journals Radiology free medical journals Radiology famous journals Radiology Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Bilateral, articles Bilateral, Research articles Bilateral, review articles Bilateral, PubMed articles Bilateral, PubMed Central articles Bilateral, 2023 articles Bilateral, 2024 articles Bilateral, Scopus articles Bilateral, impact factor journals Bilateral, Scopus journals Bilateral, PubMed journals Bilateral, medical journals Bilateral, free journals Bilateral, best journals Bilateral, top journals Bilateral, free medical journals Bilateral, famous journals Bilateral, Google Scholar indexed journals
Article Details
1. Background
Breast cancer in men tends to be diagnosed at advanced stages compared to women. Most diagnosed breast cancers in men take an invasive form, with invasive ductal carcinoma being the most prevalent. It is very rare to see ductal carcinoma in situ among men with breast cancer since it does not usually manifest as a palpable mass [1]. Male breast cancer patients generally have a lower survival rate because diagnosis is usually at advanced stages, leading to a shorter life expectancy [2]. In the absence of recommended screening in the general population for male breast cancer, taking an accurate medical history and conducting a thorough physical examination are crucial in distinguishing the etiologies of breast masses.
2. Case Presentation
A 65-year-old man presented to the general surgeon with a two-month history of bilateral dull breast pain that had been worsening between his first and second visits. During his second visit, the patient rated his pain as a 7/10 and claimed that he occasionally felt a mass on each breast. The patient’s past medical history was significant for type 2 diabetes mellitus, which was controlled by metformin, and hypertension, and the patient reported alcohol abuse and a 10-pack year smoking history. The patient denied a history of drug use. He currently works as a truck driver. His son was diagnosed with pancreatic cancer at 34, and his sister died of breast cancer at 59. The patient denied any significant weight loss, night sweats, or fever. On physical exam, there was bilateral breast tenderness along with 3 cm and 4 cm firm but mobile subareolar masses on the right and left breast, respectively. There was no skin dimpling or nipple discharge, and no enlarged lymph nodes, abnormally enlarged testicles, or hepatomegaly was observed.
On his first visit to the physician’s office, he was diagnosed with gynecomastia and was offered elective surgery, which he refused. After two months, he was referred for further evaluation due to increasing pain and the prominent bilateral palpable masses noted on his second visit.
2.1 Investigations
Laboratory investigations consisting of routine blood work and tumor markers were normal. Ultrasound revealed a hypervascular 3 cm x 2.5 cm hypoechoic mass with spiculated margins and posterior acoustic shadowing on the left and right breast, respectively. Ultrasound-guided core needle biopsy (CNB) yielded four creamy, yellow, needle-shaped soft tissues measuring 3 cm x 2.5 cmx 1.5 cm and 2.7 cm x 2 cm x 1.5 cm from the left and right breast, respectively. Microscopic sections (figure 1A-B) from the left breast indicated a malignant tumoral lesion composed of infiltrating nests and few tubules (T: 3/3) consisting of atypical cells with hyperchromatic and pleomorphic nuclei (P: 3/3) associated with mitotic figures (M: 2/3), desmoplastic stroma, and necrosis. A similar presentation was observed on the right side, except no necrosis was noted. Immunohistochemistry analysis revealed that the bilateral breast masses were positive for ER and PR but negative for HER2. The Ki67 index was less than 10% in the left breast and approximately 20% (tumor hotspot) in the right breast. Based on the CNB and FNA reports, bilateral grade II invasive ductal carcinoma was the final diagnosis. Post-mastectomy (figure 2), the diagnosis was confirmed by pathology and further indicated the presence of lymphovascular and perineural invasion of one lymph node out of 12 on the left side.
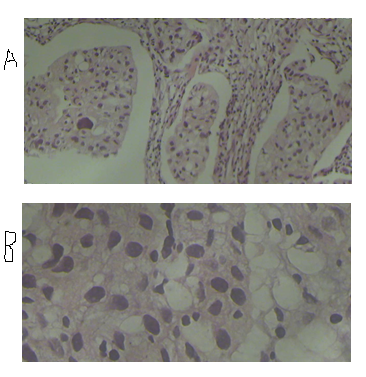
Figure 1A-B: Sheets and ductal view of malignant neoplastic cells.
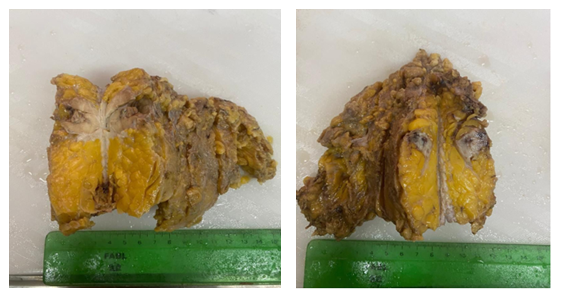
Figure 2: Macroscopic image.
2.2 Differential diagnosis
The misdiagnosis of breast cancer in men is very common, and they are often misdiagnosed as having gynecomastia (typically central in location). Some of the other less common differentials include sebaceous cysts, oil cysts, lipomas, hematomas, and lymphomas.
2.3 Outcome and follow-up
Surgical mastectomy was performed bilaterally, and the masses were removed with clear margins. The patient underwent chemotherapy one month after surgery and is now being managed with adjuvant tamoxifen therapy
3. Discussion
Breast cancer in men is known to be very rare, accounting for less than 1% of all breast cancers and less than 1% of all male malignancies in general [3]. Due to the low incidence and lack of awareness among the general population, most cases of male breast cancers are diagnosed at advanced stages. Breast cancer is also not routinely screened for in men. Breast cancer prognosis is directly associated with the stage in which the cancer is first diagnosed. Although available data regarding breast cancer in men are not as extensive as breast cancer in women, data suggest that an increase in the estrogen to testosterone ratio (Klinefelter syndrome, obesity, cryptorchidism, cirrhosis) can increase the risk of breast cancer in men. The mean age at which most men with breast cancer are diagnosed is 67 years old [4]. Family history also plays an important role in increasing the risk of breast cancer, especially in men with a family history of breast cancer in a first-degree female relative (sister), as is described in this case [5]. The risk of breast cancer in men increases with mutations in the BRCA1/2 gene. According to a population-based study performed in Italy, pathogenic BRCA1 and BRCA2 variants account for nearly 2% and 13% of all breast cancers in men, respectively [6]. Based on the National Comprehensive Cancer Network guidelines, breast cancer in men is a factor that requires further investigation into hereditary breast or ovarian cancer syndrome in diagnosed patients [4]. Thus, physicians need to take a thorough history, encompassing all pertinent information, to make an accurate diagnosis. Another risk factor present in this case is age; the incidence of breast cancer increases with age. Breast cancer cases are often confused for gynecomastia (especially the nodular type), which delays treatment. According to a study by the NYU School of Medicine, gynecomastia is prevalent and can be found in 40-55% of male autopsies [7]. Gynecomastia has a trimodal distribution: neonatal, pubertal, and geriatric. Gynecomastia is a clinical diagnosis. A physical exam is used further to differentiate gynecomastia from other differentials, notably breast cancer. Mammography is used when a physical exam is not definitive (Flowchart 1). Less than 1% of all male breast cancers are bilateral, as seen in this case. Breast cancer generally presents with a fixed subareolar mass, possible skin dimpling, and potential ulceration. Our patient did not exhibit any of the common breast cancer symptoms, aside from the subareolar mass. There are theories that breast carcinoma in men tends to form eccentrically, whereas the locus of gynecomastia (the nodular type) tends to form centrally. According to Oulmet-oliva et al. the eccentric location of lesions can be identified during physical exam to differentiate between breast cancer and gynecomastia [8]. A similar case was presented by Lambley et al., in which an 84-year-old man diagnosed with bilateral infiltrating ductal carcinoma underwent bilateral mastectomy along with axillary dissection. In their case, the patient had declined radiotherapy despite recommendations but was followed through adjuvant therapy with tamoxifen. In the Lambley case, it was noted that the patient continued to be disease-free one year postsurgery [9]. Another similar case was presented by Lehrberg et al, in which a 52-year-old man diagnosed with bilateral invasive ductal carcinoma underwent bilateral simple mastectomy with lymph node biopsy. In this case, adjuvant chemotherapy and pharmacotherapy with tamoxifen were recommended for five years in addition to surgical intervention [10]. In both cases, the importance of family history was emphasized through breast cancer history in a first- or second-degree family member. Breast cancer in men requires a multidisciplinary approach to enhance the effectiveness of treatment. Mastectomy has been the primary approach to breast cancer treatment due to the central location of most tumors’. According to Surveillance, Epidemiology, and End Results (SEER), adjuvant radiotherapy has benefitted patients with lymph node involvement and thus is recommended [4]. Chemotherapy and biological therapy (tamoxifen) are indicated for patients with locally advanced tumors, high-grade tumors, or lymph node involvement, as presented in this case.
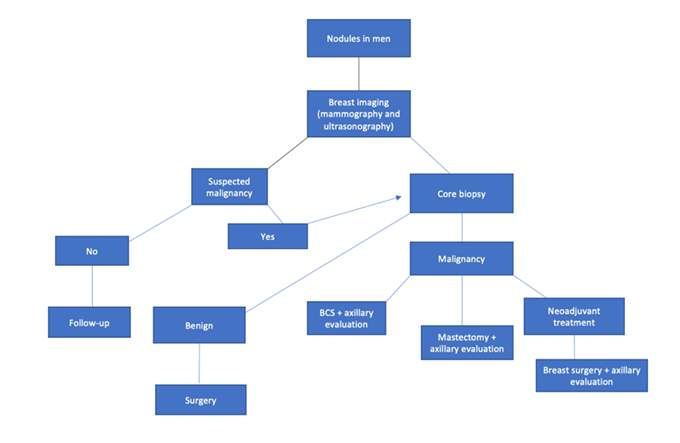
Flowchart 1: Nodule management in men.
3.1 Learning points
-The rarity of male breast cancer limits the available screening and management guidelines for patients at high risk.
-It is very important for physicians to take a thorough medical history and conduct a proper physical exam to differentiate between suspected breast cancer and gynecomastia.
-A multidisciplinary approach is required to enhance the effectiveness of treatment.
Declarations
Funding
Not applicable
Conflict of interest
Arman Sharbatdaran declares that he has no conflict of interest. Mohammed Twam declares that he has no conflict of interest. Dr. Hosseine Ghorbane declares that he has no conflict of interest. Dr. Novin Nikbakhsh declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Consent for publication was obtained from all individual participants included in the study.
Authors’ contributions
Dr. Hosseine Ghorbane and Dr. Novin Nikbakhsh were directly involved in the treatment and diagnosis of this case. Arman Sharbatdaran and Mohammed Twam contributed equally to assisting with diagnosis as well as the design and acquisition of data. Arman Sharbatdaran and Mohammed Twam contributed equally to drafting the report. Dr. Hosseine Ghorbane and Dr. Novin Nikbakhsh contributed equally to revising the report as well as analyzing and interpreting data. Arman Sharbatdaran and Mohammed Twam contributed equally to assistance with interpretation and analysis of data. The final version of the report was approved by all 4 authors. All authors agreed to be accountable for all aspects of the work.
References
- Giordano SH. Breast Cancer in Men. The New England journal of medicine 378 (2018): 2311-2320.
- Wang F, Shu X, Meszoely I, et al. Overall mortality after diagnosis of breast cancer in men vs women. JAMA oncology 5 (2019): 1589-1596.
- Breast cancer in men: a series of 45 cases and literature review. The Pan African medical journal 36 (2020): 181-183.
- Novita G, Frasson AL, Millen EC, et al. Breast Diseases: An evidence-based pocket guide. Cham: Springer International Publishing AG (2019).
- Calip GS, Kidd J, Bernhisel R, et al. Family history of breast cancer in men with non-BRCA male breast cancer: implications for cancer risk counseling. Breast cancer research and treatment 185 (2021): 195-204.
- Rizzolo P, Silvestri V, Tommasi S, et al. Male breast cancer: genetics, epigenetics, and ethical aspects. Annals of oncology 24 (2013) viii75-viii82.
- Gao Y, Heller SL, Moy L. Male Breast Cancer in the Age of Genetic Testing: An Opportunity for Early Detection, Tailored Therapy, and Surveillance. Radiographics 38 (2018): 289-311.
- Sencha AN. Imaging of Male Breast Cancer. (1st ed), Cham: Springer International Publishing (2015).
- Lambley J, Maguire E, Lam KY. Synchronous bilateral breast cancer in an elderly man. The breast journal 11 (2005): 153-153.
- Lehrberg A, Bensenhaver J. A rare presentation of bilateral, synchronous male breast cancer. The breast journal 26 (2020): 759-761.
