Benefits of IV Clonidine as Premedication on the Hemodynamic Response during Laryngoscopy and Tracheal Intubation
Article Information
Nga Nomo S1,5*, Iroume C2,6, Kuitchet Aristide3, Djomo Tamchom D4,6, Jemea B2,5, Nkoumou S, Binam F2, Ze Minkande J2
1Departement of surgery and specialties, Higher institute of medical technology, University of Douala
2Departement of surgery and specialties, Faculty of medicine and biomedical sciences, University of Yaounde 1
3Departement of surgery and specialties, Faculty of medicine and biomedical sciences, university of Garoua
4Departement of surgery and specialties, Faculty of health science, University of Buea
5Anesthesia and intensive care department, Yaounde-Essos hospital center, Cameroon
6Anesthesia and intensive care department, Yaounde Teaching Hospital, Cameroon
7Anesthesia and intensive care department, regional hospital of Maroua
8Anesthesia and intensive care department, Gyneco-obstetrics and pediatric hospital of Douala, Cameroon
*Corresponding Author: Nga Nomo Serge Vivier, Departement of Surgery and Specialities, Higher Institute of Medical Technology (ISTM) of Nkolondom, University of Douala, Cameroon.
Received: 12 June 2022; Accepted: 05 July 2022; Published: 30 December 2024
Citation:
Nga Nomo S, Iroume C, Kuitchet Aristide, Djomo Tamchom D, Jemea B, Nkoumou S, Binam F, Ze Minkande J. Benefits of IV Clonidine as Premedication on the Hemodynamic Response during Laryngoscopy and Tracheal Intubation. Anesthesia and Critical Care 6 (2024): 77-81.
View / Download Pdf Share at FacebookAbstract
Background: Clonidine is an alpha-2 adrenergic agonist which decreases the release of catecholamines at the level of the centers of regulation of blood pressure, and decreases sympathetic tone and the release of circulating catecholamines.
Patients and methods: This was a randomized single-blind clinical trial that took place over a period of 4 months. All adults classified as ASA I and II admitted for scheduled surgery and requiring general anesthesia were included. The patients were randomly divided into two groups: group A (clonidine) and group B (non-clonidine). Heart rate (HR), systolic blood pressure (SBP), and diastolic blood pressure (DBP) were observed at the following times: at the pre-anaesthetic consultation (t1), at installation on the operating table (t2), 5 minutes after clonidine infusion (t3), 1st, 3rd and 5th minute after tracheal intubation (t4, t5, t6), 1st, 3rd and 5th minute after surgical incision (t7, t8, t9).
Results: During the study period, 35 met the inclusion criteria: i.e. 20 patients for group A and 15 patients for group B. In group A, the systolic and diastolic arterial pressures decrease gradually from t3 to t6 and remain very close to the baseline values of the anesthesia consultation. In group B, there is a tendency to increase systolic and diastolic blood pressure compared to baseline values at the same times. Tachycardia is found in group B while a tendency to bradycardia is encountered in group A from t3 to t6.
Conclusion: Clonidine helps to control sympathetic hyperactivity, arterial hypertension and reflex tachycardia, induced by tracheal intubation.
Keywords
Benefits of clonidine, Premedication, Laryngoscopy, Tracheal intubation
Benefits of clonidine articles, Premedication articles, Laryngoscopy articles, Tracheal intubation articles
Article Details
Introduction
Laryngoscopy and tracheal intubation generate intense nociceptive stimulations which induce sympathetic stimulation responsible for tachycardia, arterial hypertension and arrhythmias [1-3]. The intensity of the hemodynamic response is directly related to the duration and force of the laryngoscopy [2]. In patients with no cardiovascular disorder, laryngoscopy and intubation lead to a highly variable increase in blood pressure, on average 40% to 50%, with a 20% increase in heart rate [2]. This rise in blood pressure figures is greater in unbalanced hypertensive patients [2]. In patients with coronary insufficiency, myocardial ischemia can be observed [2,4]. To limit this adrenergic stimulation during the tracheal intubation procedure, many agents have been tried without satisfactory results [1-7]. The combination of clonidine with morphinomimetics could to give better results in this indication. Compared to dexmedetomidine which is recently introduced in anesthetic pharmacology, clonidine is an alpha-2 adrenergic agonist accessible to poor populations in sub-Saharan Africa, it is easy to handle. This molecule has long been used in the African continent for the treatment of arterial hypertension before being replaced by new latest generation treatments. In recent years, new indications for general anesthesia have been discovered. The primary objective of our study was to evaluate the beneficial effects of intravenous (IV) clonidine on the hemodynamic response during the tracheal intubation procedure.
Patients and methods
This was a randomized single-blind clinical trial that took place over a period of 4 months from February to May 2016, in the anesthesia department of the Essos hospital center (Cameroon). All adult patients (age >18 years) classified as ASA I and ASA II, according to the American Society of Anesthesiologists, admitted for scheduled surgery and requiring general anesthesia with orotracheal intubation were included in the study. Pregnant women and surgical emergencies were excluded. Premedication was non-medication for all study participants. The patients were randomly divided into two groups by drawing lots: group A (clonidine) and group B (non-clonidine). All patients in group A received clonidine (3μg/kg) intravenously diluted in 250mL of isotonic saline 10 minutes before anesthetic induction. Intravenous (IV) induction of general anesthesia was classic, after 5 minutes of preoxygenation (FiO2 100%): fentanyl (3μg/kg), propofol (3mg/kg), vecuronium bromide (0.1mg/kg). Tracheal intubation was performed with an appropriately sized cuffed tracheal tube. Maintenance of anesthesia was provided with isoflurane, reinjections of fentanyl and vecuronium as needed for surgery. Heart rate (HR), systolic blood pressure (SBP), and diastolic blood pressure (DBP) were observed at the following times: during the pre-anaesthetic consultation (t1), at installation on the operating table (t2), 10 minutes after clonidine infusion (t3), at 1st, 3rd and 5th minute after tracheal intubation and cuff inflation (t4, t5, t6), at 1st, 3rd and 5th minute after incision surgery (t7, t8, t9). Rescue drugs were atropine 0.5 mg IV if heart rate was less than 50/min, or ephedrine 5 mg IV if systolic blood pressure fell more than 25% of baseline anesthesia consultation. The primary endpoints were the effectiveness of microinfusion administration of clonidine for 10 minutes in attenuating sympathetic overactivity (heart rate, diatolic blood pressure, and systolic blood pressure) induced by laryngoscopy and tracheal intubation. The secondary endpoint was to look for the adverse effects of this procedure. The patients involved in the data collection were not aware of the distribution of the groups; only the anesthetist in charge of the procedure was informed. Data entry and analysis were done using Microsoft Word 2007, Microsoft Excel 2007, EPI Info 7 and SPSS16.0 software. A p-value less than 0.05 were considered as statistical significance. Due to the small sample size, the results are expressed as the median.
Results
During the study period, 562 patients were operated on in the operating theaters of the Essos hospital centre, of which 35 met the inclusion criteria: i.e. 20 patients for group A and 15 patients for group B. average age was 34 years with extremes ranging from 19 to 75 years. The sex ratio was in favor of the male gender in both groups: 2.3 in group A and 2.7 in group B. Table 1 presents the socio-demographic and clinical characteristics of the study population.
|
Variables |
Group A |
Group B |
Total |
|
n=20 |
n=15 |
||
|
Age group (year) |
|||
|
[19-35] |
7 |
5 |
12 |
|
[35-50] |
8 |
6 |
14 |
|
[50-65] |
4 |
4 |
8 |
|
[65-80] |
- |
- |
- |
|
>80 |
1 |
- |
1 |
|
Total |
20 |
15 |
35 |
|
Weight |
|||
|
Nomal |
13 |
9 |
22 |
|
overweight |
5 |
3 |
8 |
|
Obese |
2 |
3 |
5 |
|
Total |
20 |
15 |
35 |
|
Gender |
|||
|
Male |
6 |
4 |
10 |
|
Female |
14 |
11 |
25 |
|
Total |
20 |
15 |
35 |
|
ASA |
|||
|
I |
16 |
10 |
26 |
|
II |
4 |
5 |
9 |
|
Total |
20 |
15 |
35 |
Table 1: Demographic profile of patients
The ASA1 class was the most represented in both groups (74.3%). Visceral surgery was the most performed surgical specialty (Table 2) in the 2 groups: 55% (n=11) for group A versus 53% (n=8) for group B.
|
Surgical specialty |
Group A |
Group B |
||
|
n |
% |
n |
% |
|
|
Visceral surgery |
11 |
55 |
8 |
53 |
|
Traumatology |
8 |
40 |
4 |
26.7 |
|
ENT surgery |
1 |
5 |
2 |
13.3 |
|
Gynecology |
- |
- |
1 |
6.7 |
Table 2: Distribution of participants according to surgical specialty
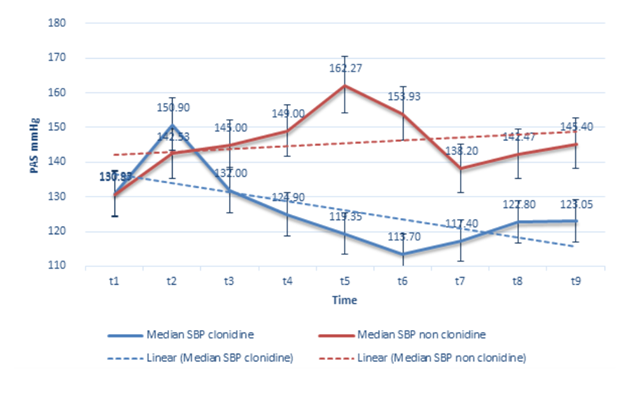
In group A (clonidine), there is a very slight variation in SBP from t4 to t6 compared to the baseline values obtained at the anesthesia consultation; the slope of the systolic blood pressure curve is negative in this sample of the study population, the systolic blood pressure trend curve shows a linear drop in blood pressure (Figure 1). In group B (non-clonidine), the SBP increases rapidly from t4 to t5, then there is a shift in the SBP curve from t5 to t6, but the SBP values remain well above the baseline values obtained at the consultation preanaesthetic. The SBP trend line shows a steady increase in blood pressure in this group of participants (Figure 1).
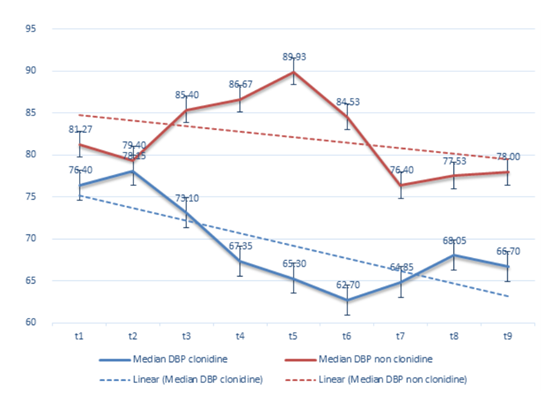
A gradual drop in diastolic blood pressure is observed in both groups (Figure 2), but this drop in diastolic blood pressure is more significant in group A (clonidine).
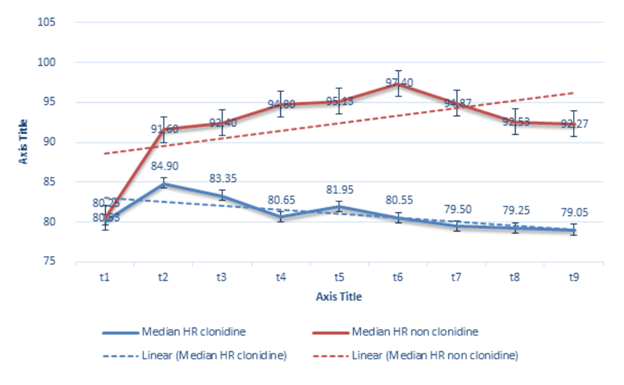
The slope of the heart rate trend curve is negative in group A (clonidine), while it remains positive in group B (non-clonidine). A regular and significant increase in heart rate is observed in the clonidine group, between t4 and t6 compared to the baseline values of the anesthesia consultation (figure 3), while in group A (clonidine) there is a tendency to bradycardia in the same time intervals.
Discussion
Tracheal intubation is a common procedure in general anesthesia, it is correlated with a significant release of catecholamines into the bloodstream. Clonidine hydrochloride is a powerful antihypertensive agent, used clinically since 1974 in the United States [8-10]. It is an alpha-adrenergic receptor agonist [9], which stimulates central alpha receptors in the depressant site of the vasomotor center of the medulla oblongata and hypothalamus, which decreases efferent sympathetic tone to the heart, the kidneys and peripheral vasculature with a concomitant increase in vagal activity [8-10]. Alpha-2 adrenergic agonists have seen renewed interest in anesthesia in recent years [11-13]. They are used as adjuvants, both for locoregional anesthesia and for general anesthesia [1,4,11,12]. In developed countries, dexmedetomidine is the molecule of choice in the family of alpha-2 adrenergic agonists [15,16], to limit the complications induced by the laryngoscopic nociceptive stimulus [15,16]. The low cost of clonidine, its availability and ease of handling make it an excellent alternative to dexmedetomidine in sub-Saharan Africa, in the prevention of sympathetic hyperactivity induced by tracheal intubation. Young adults constituted the majority of the workforce in both groups with an average age of 32 years, the most represented ASA1 class. Matot et al. in a work on the effect of clonidine premedication on hemodynamic responses to microlaryngoscopy and rigid bronchoscopy, found a mean age of 60 years with extremes ranging from 50 to 76 years [17]. ASA1 class was also the most represented in the two clonidine and control groups [17]. The strong representation of the age group of young adults in our series could be explained by the age pyramid in Cameroon [18]. According to the results of the last population census in Cameroon, half of the population is under 17.7 years old and the demographic weight of those under 15 is 43.6%. People over the age of 60 represent only 5.5% of the total population [18]. These young adults represent a population group that has very few defects, which could justify the strong dominance of ASA1 class. Referring to the last census of the Cameroonian population, we also realize that Cameroon still has a slightly more women (50.6%) than men (49.4%). This demographic trend would explain the strong predominance of the female gender in the two groups in our study. In our work, we found a small proportion of obese patients (14%). Overweight and obesity are defined as an abnormal or excessive accumulation of body fat that can impair health. For adults, the World Health Organization defines overweight when the body mass index (BMI) ≥25 and obesity when the BMI ≥30. Body mass index is the most useful measure of overweight and obesity in a population because, in adults, the scale is the same regardless of gender or age. However, it gives an approximate indication because it does not necessarily correspond to the same degree of adiposity from one individual to another. In anesthesia, the risk of difficult intubation is increased in the obese, the pharmacokinetics of anesthetics, in particular clonidine, is also modified [19]. In our series, we notice at installation on the operating table (t2), a considerable rise in systolic and diastolic arterial pressures, and heart rate in both groups in a similar way compared to the baseline values of the pre-anaesthetic consultation. This sudden increase in blood pressure figures could be linked to the stress generated by the environment of the operating room. After the clonidine infusion (t3), the systolic blood pressure decreases to approach the baseline values of the pre-anaesthetic consultation for patients in group A. Systolic blood pressure shows little variation after tracheal intubation in the clonidine group, it remains very close to the basic values. On the contrary, there is an explosive increase in systolic blood pressure from the installation on the operating table, until the 5th minute after tracheal intubation. The change in heart rate is superimposable on that of systolic blood pressure in the two groups. While a regular increase in heart rate is observed in group B (non-clonidine), there is a tendency to bradycardia in group A (clonidine) with a heart rate which remains stable at around 60/minute. In a work carried out by Hussain SY et all [20] in 2018, relating to the evaluation and comparison of the effects of clonidine and dexmedetominine versus placebo on the reduction of the hemodynamic effects induced by laryngoscopy, heart rate, systolic, diastolic and mean arterial pressures were lowered more in the clonidine and dexmedetomindine groups compared to the placebo group at all measured times. In this study, 90 patients of American Society of Anesthesiologists physical status I and II were randomized into three groups, namely group C (clonidine 2 μg/kg), group D (dexmedetomidine 1 μg/kg) and group S (normal saline) infused over 10 minutes. Blood pressures - systolic (SBP) and diastolic (DBP), mean arterial pressure (MAP) and heart rate (HR) were recorded after drug administration and intubation at regular intervals. Heart rate was significantly lower in the dexmedetomidine group compared to the clonidine group after drug infusion. At 1 min after intubation, SBP and MAP were lower in the dexmedetomidine group compared to the clonidine group. At 3, 5, and 10 minutes after intubation, SBP, DBP, and MAP were lower in the dexmedetomidine group compared to the clonidine group [20]. The authors concluded that the hemodynamic response was significantly reduced in the dexmedetomidine and clonidine groups compared to the control group [20]. They specify that this reduction in the hemodynamic response to laryngoscopic stimuli and tracheal intubation was better in the dexmedetomidine group [20]. Sarkar A et al compared the effects of IV clonidine as premedication on the hemodynamic response to tracheal intubation [21]. This was a prospective randomized and controlled study involving 75 adult patients, classified ASA 1 and 2 according to the American Society of Anesthesiologists. The patients were randomly divided into three groups of 25 patients each. Clonidine (3 μg/kg) or dexmedetomidine (0.5 μg/kg) or placebo (0.9% normal saline) diluted in 100 ml of 0.9% NaCl was infused over a period of 10 min in the operating room [21]. It has been found that an attenuation of the hemodynamic response to painful stimuli induced by laryngoscopy, with clonidine and dexmedetomidine without remarkable side effects [21]. In the systematic review conducted by Sanchez Munoz MC et al. [12], covering 57 meta-analyses that dealt with the place of clonidine in anesthesia, it was concluded that clonidine improves hemodynamic and sympathetic stability, without harmful consequences on renal function or wake-up time. The results obtained in our study are similar to those of many authors who have worked on the interest of clonidine on the hemodynamic response during the tracheal intubation procedure. The pharmacological activity of alpha-2 adrenergic receptor agonists explains the attenuation of the hemodynamic effects of clonidine on stimuli induced by laryngoscopy and tracheal intubation. Nociceptive stimuli from the A delta and C afferent fibers are transmitted to neurons in the posterior horn of the spinal cord, called convergent neurons. The activity of convergent neurons is regulated by descending noradrenergic pathways from the brainstem nuclei. Stimulation of these neural pathways inhibits pain transmission with release of norepinephrine. This action is blocked by alpha-2 adrenergic receptor antagonists. Clonidine blocks the activity of convergent neurons induced by stimulation of C and A delta fibres. This would explain the significant reduction in the catecholaminergic storm induced by tracheal intubation. The study’s sample size can be considered an initial limitation since the number of patients was relatively small. Another limitation of our study was a single-center study, and the results should not be generalized. Additional research is required to evaluate the practice of pediatric anesthesia in an adult operating theater.
Conclusion
Clonidine is an alpha-2 adrenergic receptor agonist of the imidazoline family. In addition to its ability to lower blood pressure, it has many other indications in anesthesia. Our results show that the use of IV clonidine a few minutes before anesthetic induction should be encouraged to prevent side effects related to laryngoscopy and tracheal intubation stimuli in precarious patients, particularly coronary insufficiency and hypertensive patients.
Conflicts of interest
The authors declare no conflicts of interest.
Author Contribution
All authors contributed to the development and conduction of this manuscript. All authors have read and approved the final version of the manuscript.
Acknowledgments
The authors wish to thank the anesthesiologists, surgeons and the nursing staff of the operating theatre of the Yaounde/Essos Hospital Center for their support of this study
References
- Yeganeh N, Roshani B, Latifi H et al. Comparison of target-controlled infusion of sufentanil and remifentanil in blunting hemodynamic response to tracheal intubation. J Inj Violence Res 5 (2013): 101-107.
- Bruder N, Ortega D, Granthil C. Conséquences et moyens de prévention des modifications hémodynamiques lors de la laryngoscopie et de l'intubation endotrachéale. Annales Françaises d'Anesthésie et de Réanimation 11 (1992): 57-71.
- Anthony LK. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. Journal of Clinical Anesthesia 8 (1996): 63-79.
- Aditya PM, Prakash KD, Alok R. Comparison between dexmedetomidine and fentanyl bolus in attenuating the stress response to laryngoscopy and tracheal intubation: a randomized double-blind trial. Brazilian Journal of Anesthesiology 72 (2022): 103-109.
- Sulaiman S, Karthekeyan RB, Vakamudi M, et al. The effects of dexmedetomidine on attenuation of stress response to endotracheal intubation in patients undergoing elective off-pump coronary artery bypass grafting. Ann Card Anaesth 15 (2012): 39-43.
- Laha A, Ghosh S, Sarkar S. Attenuation of sympathoadrenal responses and anesthetic requirement by dexmedetomidine. Anesth Essays Res 7 (2013): 65-70.
- Gunalan S, Venkatraman R, Sivarajan G, et al. Comparative evaluation of bolus administration of dexmedetomidine and fentanyl for stress attenuation during laryngoscopy and endotracheal intubation. J Clin Diagn Res 9 (2015): UC06-09.
- Houston MC. Clonidine hydrochloride. South Med J 75 (1982): 7193-7199.
- Houston MC. Clonidine hydrochloride: review of pharmacologic and clinical aspects. Prog Cardiovasc Dis. 23 (1981): 337-350.
- Kosman ME. Evaluation of clonidine hydrochloride (Catapres). A new antihypertensive agent. JAMA 233 (1975): 174-176.
- Nguyen V, Tiemann D, Park E, et al. Alpha-2 Agonists. Anesthesiol Clin 35 (2017): 233-245.
- Sanchez Munoz MC, De Kock M, Forget P. What is the place of clonidine in anesthesia? Systematic review and meta-analyses of randomized controlled trials. J Clin Anesth 38 (2017): 140-153.
- Afshari A. Clonidine in pediatric anesthesia: the new panacea or a drug still looking for an indication? Curr Opin Anaesthesiol 32 (2019): 327-333.
- Misra S, Behera BK, Mitra JK et al. Effect of preoperative dexmedetomidine nebulization on the hemodynamic response to laryngoscopy and intubation: a randomized control trial. Korean J Anesthesiol. 74 (2021): 150-157.
- Koh V, Ali S, Hassan MH et al. Comparison of Esmolol and Dexmedetomidine Infusion in Attenuating Haemodynamic and Blood Glucose Response to Laryngoscopy and Intubation: A Single Blinded Study. Malays J Med Sci 28 (2021): 46-55.
- Mahjoubifard M, Heidari M, Dahmardeh M et al. Comparison of Dexmedetomidine, Lidocaine, and Fentanyl in Attenuation Hemodynamic Response of Laryngoscopy and Intubation in Patients Undergoing Cardiac Surgery. Anesthesiol Res Pract. 1 (2020): 4814037.
- Matot I, Sichel JY, Yofe V et al. The effect of clonidine premedication on hemodynamic responses to microlaryngoscopy and rigid bronchoscopy. Anesth Analg. 91 (2000): 828-33.
- Ngwe, Emmanuel. La Collecte des Données Démographiques au Cameroun: Evolution et Problèmes. African Population Studies 22 (2013): 222-337.
- Anne Mongredien-Menigaux. Anesthésie du patient obèse. Le Praticien en Anesthésie Réanimation 12 (2008): 85-91.
- Hussain SY, Karmarkar A, Jain D. Evaluation and Comparison of Clonidine and Dexmedetomidine for Attenuation of Hemodynamic Response to Laryngoscopy and Intubation: A Randomized Controlled Study. Anesth Essays Res 12 (2018): 792-796.
- Sarkar A, Tripathi RK, Choubey S et al. Comparison of effects of intravenous clonidine and dexmedetomidine for blunting pressor response during laryngoscopy and tracheal intubation: A randomized control study. Anesth Essays Res 8 (2014): 361-366.