Atopy and Food Allergies among Children Attending Outpatient Department of a Selected Tertiary Care Hospital in Dhaka City
Article Information
Biplob Biswas1, Wahida Khanam2, Delwar Hossain3, Mohammad Ahad Adnan4, Uttam Kumar Datta5, A.K. Naseruzzaman6, Zamil Ahmed Manik7, Tauhidul Islam8
1Assistant Surgeon, Department of Paediatrics, Institute of Child and Mother Health, Dhaka, Bangladesh
2Head, Department of Paediatrics, Institute of Child and Mother Health, Dhaka, Bangladesh
3Professor, Department of Paediatrics Pulmonology, Institute of Child and Mother Health, Dhaka, Bangladesh
4Registrar, Department ofGeneral Paediatric, Institute of Child and Mother Health, Dhaka, Bangladesh
5Assistant Registrar, Department of Paediatrics, Institute of Child and Mother Health, Dhaka, Bangladesh
6Assistant Professor, Department of Paediatrics, Institute of Child and Mother Health, Dhaka, Bangladesh
7Associate Professor, Department of Paediatrics (Haemato-Oncology), Institute of Child and Mother Health, Dhaka, Bangladesh
8Assistant Professor, Department of Paediatrics, Institute of Child and Mother Health, Dhaka, Bangladesh
*Corresponding author: Dr. Biplob Biswas, Assitant Surgeon, Department of Paediatrics, Institute of Child and Mother Health, Dhaka, Bangladesh.
Received: 25 May 2023; Accepted: 05 June 2023; Published: 14 June 2023
Citation: Biplob Biswas, Wahida Khanam, Delwar Hossain, Mohammad Ahad Adnan, Uttam Kumar Datta, A.K. Naseruzzaman, Zamil Ahmed Manik, Tauhidul Islam. Atopy and Food Allergies among Children Attending Outpatient Department of a Selected Tertiary Care Hospital in Dhaka City. Journal of Biotechnology and Biomedicine. 6 (2023): 259-264.
View / Download Pdf Share at FacebookAbstract
Background: Atopic dermatitis (AD), also called atopic eczema, is a common chronic or recurrent inflammatory skin disease and affects 15-20% of children.
Objective: The aim of the study was to determine the proportion of atopy and food allergies among children attending outpatient department of a selected tertiary care hospital in Dhaka city.
Methodology: This was a cross-sectional study. It was carried out on 384 children from June 2022 to December 2022 at pediatric outpatient department in Institute of child and mother health (ICMH), Dhaka, Bangladesh. The statistical evaluation of the results by using a window-based computer software program devised with Statistical Packages for Social Sciences (SPSS-24).
Result: Total 384 children were enrolled among them Mean age was (1.15±0.43) years, 52% were female and 92.18% had a family history of atopy. Regarding symptoms 4.3% had lip or tongue swelling, 8.5% had difficulty in swallowing, 39.30% had urticaria, 13.7% had dyspnea and 5.1% had anaphylaxis. 82.8% of the respondents had mild illness, 11.98% had moderate illness and 5.21% had severe illness. 48.6% had Cow's Milk allergy, 19.5% to beef, 3.3% to egg ,2.6%to hilsa fish and prawn respectively and 22.3% to others. Mean Eosinophil count was (11.62±2.14), IgE was (747.40±314.2) IU and the skin prick test was positive 90.0%.
Conclusion: The predominant sign of food allergy in young children was atopic dermatitis. Allergic conjunctivitis, oral allergy syndrome and respiratory distress appeared later in the progression of symptoms. Additionally, anaphylaxis is usually used to affect older children.
Keywords
IgE; Atopic dermatitis; Food Allergies
IgE articles IgE Research articles IgE review articles IgE PubMed articles IgE PubMed Central articles IgE 2023 articles IgE 2024 articles IgE Scopus articles IgE impact factor journals IgE Scopus journals IgE PubMed journals IgE medical journals IgE free journals IgE best journals IgE top journals IgE free medical journals IgE famous journals IgE Google Scholar indexed journals Atopic dermatitis articles Atopic dermatitis Research articles Atopic dermatitis review articles Atopic dermatitis PubMed articles Atopic dermatitis PubMed Central articles Atopic dermatitis 2023 articles Atopic dermatitis 2024 articles Atopic dermatitis Scopus articles Atopic dermatitis impact factor journals Atopic dermatitis Scopus journals Atopic dermatitis PubMed journals Atopic dermatitis medical journals Atopic dermatitis free journals Atopic dermatitis best journals Atopic dermatitis top journals Atopic dermatitis free medical journals Atopic dermatitis famous journals Atopic dermatitis Google Scholar indexed journals Food Allergies articles Food Allergies Research articles Food Allergies review articles Food Allergies PubMed articles Food Allergies PubMed Central articles Food Allergies 2023 articles Food Allergies 2024 articles Food Allergies Scopus articles Food Allergies impact factor journals Food Allergies Scopus journals Food Allergies PubMed journals Food Allergies medical journals Food Allergies free journals Food Allergies best journals Food Allergies top journals Food Allergies free medical journals Food Allergies famous journals Food Allergies Google Scholar indexed journals allergy articles allergy Research articles allergy review articles allergy PubMed articles allergy PubMed Central articles allergy 2023 articles allergy 2024 articles allergy Scopus articles allergy impact factor journals allergy Scopus journals allergy PubMed journals allergy medical journals allergy free journals allergy best journals allergy top journals allergy free medical journals allergy famous journals allergy Google Scholar indexed journals environmental articles environmental Research articles environmental review articles environmental PubMed articles environmental PubMed Central articles environmental 2023 articles environmental 2024 articles environmental Scopus articles environmental impact factor journals environmental Scopus journals environmental PubMed journals environmental medical journals environmental free journals environmental best journals environmental top journals environmental free medical journals environmental famous journals environmental Google Scholar indexed journals rhinitis articles rhinitis Research articles rhinitis review articles rhinitis PubMed articles rhinitis PubMed Central articles rhinitis 2023 articles rhinitis 2024 articles rhinitis Scopus articles rhinitis impact factor journals rhinitis Scopus journals rhinitis PubMed journals rhinitis medical journals rhinitis free journals rhinitis best journals rhinitis top journals rhinitis free medical journals rhinitis famous journals rhinitis Google Scholar indexed journals asthma articles asthma Research articles asthma review articles asthma PubMed articles asthma PubMed Central articles asthma 2023 articles asthma 2024 articles asthma Scopus articles asthma impact factor journals asthma Scopus journals asthma PubMed journals asthma medical journals asthma free journals asthma best journals asthma top journals asthma free medical journals asthma famous journals asthma Google Scholar indexed journals immune system articles immune system Research articles immune system review articles immune system PubMed articles immune system PubMed Central articles immune system 2023 articles immune system 2024 articles immune system Scopus articles immune system impact factor journals immune system Scopus journals immune system PubMed journals immune system medical journals immune system free journals immune system best journals immune system top journals immune system free medical journals immune system famous journals immune system Google Scholar indexed journals biological articles biological Research articles biological review articles biological PubMed articles biological PubMed Central articles biological 2023 articles biological 2024 articles biological Scopus articles biological impact factor journals biological Scopus journals biological PubMed journals biological medical journals biological free journals biological best journals biological top journals biological free medical journals biological famous journals biological Google Scholar indexed journals skin disease articles skin disease Research articles skin disease review articles skin disease PubMed articles skin disease PubMed Central articles skin disease 2023 articles skin disease 2024 articles skin disease Scopus articles skin disease impact factor journals skin disease Scopus journals skin disease PubMed journals skin disease medical journals skin disease free journals skin disease best journals skin disease top journals skin disease free medical journals skin disease famous journals skin disease Google Scholar indexed journals
Article Details
Introduction
Atopy is a specific type of allergy which is a predisposition to an immune response against divers’ antigens and allergen leading to CD 4 + Th 2 differentiation and over-production of immunoglobulin E(IgE). [1] The manifestation of allergic illnesses are caused by genetic and environmental factors, but inheritance is still thought to be more significant than any environmental impacts. [2-4] The hereditary susceptibility to develop allergic conditions like allergic rhinitis, asthma, and atopic dermatitis is known as atopy. [5] If anyone have an atopic condition, his/her immune system usually overreacts to certain triggers and produces too much IgE, causing inflammation. [6] For the ability to recognize antigenic specificities, immunoglobulin E (IgE) generated by plasma cells is the key player in allergic reactions. Following first sensitization, exposure to the same allergen again causes the production of a number of cytokines that result in the symptoms of atopic conditions. [7,8] A positive genetic history of atopy had already been defined as either single or double depending on whether the disease affected one parent, a biological sibling, or both parents. [9] Depending on condition, the symptoms of inflammation can be anything from a rash to watery eyes, a runny nose, or a restricted airway. [10] Atopic dermatitis (AD), also called atopic eczema, is a common chronic or recurrent inflammatory skin disease that affects 15-20% of children [5] and 1-3% of adults worldwide. [11] Bangladesh reported the prevalence of atopic dermatitis to be 6.0% and 7.1% in children 6–7 years and 13–14 years, respectively. [12] The prevalence of atopy has been rising, and atopic illness is a frequent health issue. [13] According to the First National Asthma Prevalence Study (FNAP) conducted in Bangladesh in 1999, 7.4% of the paediatric population (1-15 years of age group) currently have asthma and have at least two or three episodes of asthma attacks per year. [14]
Food is an integral part of life, even though some foods are responsible for allergies and some may even lead to fatality. [15] Over 2000 years ago, Hippocrates first recognized the adverse reactions to food who often addressed as the “Father of Medicine”. [16] Different genetic factors are also responsible for allergic reactions to food as having two or more family members with a history of allergy was more strongly predictive of food allergy in the child. [17] The body's immune system reacts abnormally to a particular food, it is known as a food allergy. Food allergies happen among children when a food is perceived as a "threat" by the child's immune system. This immunologic adverse reaction are not due to toxic contaminants or pharmacologic characteristics of the food; it may be due to metabolic disorders of the host or idiosyncratic responses, such as lactase deficiency. [18-20] Due to the immature immune system in childhood and/or the inappropriate food introductory practices, children are more likely to develop food allergies than adults. [21] A current study revealed that about 20% of the adult population of developed countries and 40-50% of school-going children suffered from different allergic problems. [22] Food allergy symptoms usually develop within a few minutes to 2 hours after eating the offending food. Rarely, symptoms may be delayed for several hours. The most common sign and symptoms of food allergy include tingling and itching in the skin and mouth, rashes, angioedema, dermatitis, as well as in the gastrointestinal tract including vomiting, abdominal cramping, nausea, diarrhea and in the respiratory tract disorder including rhinitis, asthma and laryngeal edema. [23-25] Anaphylactic shock is the most frightening symptom which is induced by a particular food that is acute in onset, occurring within minutes or hours, and without proper treatment, it may lead to death badly. [26, 27] Much other allergic disorder has been found in different organ systems that increase the risk of other allergic condition due to consuming allergic food items. [28-29] These conditions could be minimized if proper strategies are taken followed by its early identification. [19] About 49% perceived diet plays an important part in the control of their asthma was investigated by Melbourne Hospital [29]. The most common allergenic foods are beef, cow's milk and dairy products, brinjal, hen’s egg, prawn, peanuts, gluten-containing cereals (e.g., wheat, rye, barley), mustard sesame, soybeans, fish, nuts crustaceans, and shellfish. [30,31] Cow's milk and eggs are recognized as the most common food allergens in the United States, while fruits and eggs in Europe and Middle East countries respectively. [32,33] By changing the environmental lifestyle and adopting a westernized lifestyle increased the frequency of food allergy, as the western populations documenting the highest prevalence. [34,35] Children with severe Aopic Dermatitis (AD) comprise about 35% of those who also have a food allergy. [36] The clinical control of AD becomes defaults when children are exposed to seasonal and chronic respiratory allergens. [7,37] This current study was designed to document the proportion of atopy and food allergies among children as well as to identify the risk factors associated with food allergies and atopy.
Objective
The aim of the study was to determine the proportion of atopy and food allergies among children attending Outpatient Department of a selected tertiary care hospital in Dhaka city.
Methods
This was a cross-sectional study. It was carried out on 384 population and duration was June 2022 to December 2022 in Institute of child and mother health (ICMH), Dhaka, Bangladesh at pediatric outpatient department. The Pediatrician was primarily involved in the decision-making process. The choice of treatment was made by the physician after a full discussion with the multidisciplinary team consisting of Pediatrician. Inclusion criteria were age one year to ten years, both Genders attended OPD with H/O runny nose, red eyes, skin itching and urticaria, parents interested to participant. And attend OPD with H/O exposure to pollen dust, cold, pet, carpet and ingest of allergic food. Exclusion criteria were sign and symptoms of atopy and allergy after intake of any kind of drugs. All respondents were clarified about the study and an informed consent in written form was obtained from each respondent or authorized person after proper counseling. Data was collected by using a structured questionnaire. We ensured participants that any personal information will not be disclosed anywhere. To diagnose food allergies and atopy, we first talked to parents about reactions to certain foods, atopic disease (atopic dermatitis, allergic rhinitis and asthma) and, then detailed medical history & physical examination were done. Skin prick tests or blood tests checked for reactions to specific food allergens. For this test, a blood sample was sent by maintain all aseptic precaution to a medical laboratory (ICMH laboratory, ICDDRB laboratory and BSMMU laboratory), where different parameter (laboratory test reports including CBC, Eosinophil count, IgE, skin prick test) were tested. The CBC is usually performed by an automated hematology analyzer, which counts cells and collects information on their size and structure. An allergen-specific immunoglobulin E (IgE) test is a blood test that measures the levels of different IgE antibodies in a person's blood. Allergen-specific IgE tests are sometimes used to diagnose and better management of food allergies. They can also be helpful for environmental allergy diagnosis in some cases. Skin prick tests is the most accurate and least expensive way to confirm allergens. Skin prick tests is a simple, safe and quick test, that gives results within 15-20 minutes. The test involves placing a small amount of the suspected allergy-causing substance (allergen) on the skin (usually the forearm, upper arm, or the back), and then scratching or pricking the skin so that the allergen is introduced under the skin surface. About 15 minutes after the skin pricks, the physician observes respondent skin for signs of allergic reactions. If respondents are allergic to one of the substances tested, they developed a raised, red, itchy bump (wheal) that may look like a mosquito bite. The physicians were measured the bump's size and record the results. Demographic and personal details of the respondents, relevant history and associated co-morbidities were recorded. After completion of data collection, to maintain consistency, the data were checked and verified for any omission, error or irrelevance before tabulation. The statistical evaluation of the results by using a window-based computer software program devised with Statistical Packages for Social Sciences (SPSS-24). Ethical approval was obtained from the Institutional Review Board (IRB) of Institute of child and mother health (ICMH), Dhaka, Bangladesh.
Figure-1 shows that about 75.2% of the respondents were aged between 1-5 year and 24.8% of the respondents were aged between 6-10 year. Mean(±SD) age was 1.15(±0.43).
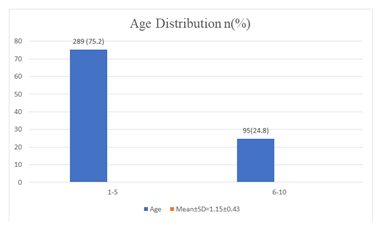
Figure 1: Distribution of the respondents by age.
Figure shows about 52% of the respondents were female and 48% were male.
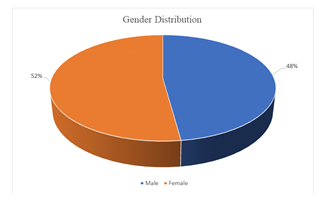
Figure 2: Distribution of the respondents by gender.
About 57.30% of the respondent had kacha house and 42.70 had building.
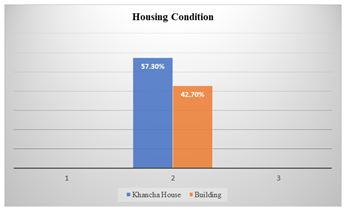
Figure 3: Distribution of the respondents by housing condition
|
Family history of atopy |
n=384 |
% |
|
Yes |
354 |
92.18 |
|
No |
30 |
7.8 |
|
Total |
384 |
100 |
Table-1 shows that 92.18% of the respondent had family history of atopy.
Table 1: Distribution of the respondents by Family history of atopy
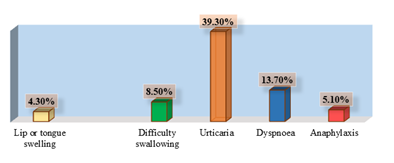
Figure 4: Distribution of the respondents by clinical symptoms.
Figure-IV shows 4.30% of the respondents had lip or tongue swelling, 8.50% had difficulty swallowing, 39.30% had urticarial, 13.70% had dyspnea and 5.10% had anaphylaxis.
|
Severity of illness |
n=384 |
% |
|
Mild |
318 |
82.8 |
|
Moderate |
46 |
12 |
|
Severe |
20 |
5.21 |
|
Total |
384 |
100 |
Table-2 shows that 82.8% of the respondents had mild illness, 11.98% had moderate illness and 5.21% had severe illness.
Table-2: Distribution of the respondents by Severity of illness
|
Food allergy |
n=384 |
% |
|
Egg |
13 |
3.3 |
|
Cow's Milk |
187 |
48.6 |
|
Beef |
75 |
19.5 |
|
Hilsa Fish |
10 |
2.6 |
|
Prawn |
10 |
2.6 |
|
Brinjal |
3 |
0.8 |
|
Others |
86 |
22.3 |
Table-3 shows 48.6% of the respondents had allergy to Cow's Milk,19.5% to beef, 3.3% to egg, 2.6%to hilsa fish and prawn respectively and 22.3% to others.
Table 6: Distribution of the respondents by food allergy.
|
Investigation |
Mean(±SD) |
|
Eosinophil |
11.62(±2.14) |
|
IgE |
747.40(±314.2) |
Table-7 shows the mean Eosinophil was11.62(±2.14), IgE was 747.40(±314.2).
Table 4: Distribution of the respondents by findings of investigation
Figure V shows the skin prick test was positive 90.0% children.
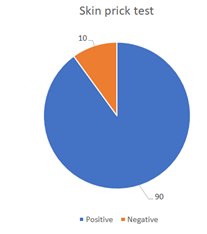
Figure 5: Percentage of skin prick test.
Discussion
This is a cross-sectional study. This study was carried out on 384 respondents to find out the population including male and female, age one year to ten years at pediatric outpatient department in Institute of Child and mother health (ICMH).
In our study about 75.2% of the respondents were aged between 1-5 year and 24.8% of the respondents were aged between 6-10 year. Mean(±SD) age was 1.15(±0.43). A study showed that respondents were aged 5 months-16 years [38]. Our study showed that about 52% of the respondents were female and 48% were male. Another study showed majority (75%) were male and 25% were female [38]. Our study showed that, about 57.30% of the respondent had kacha house and 42.70 had building. Regarding education 55.6% father of the respondent had completed primary level education,17.9% secondary level, and 14.5% were graduate. About 1.7% had no formal schooling. that 56.4% Mother of the respondent had completed primary level education, 22.2% secondary level, and 11.1% were graduate. About 3.1% had no formal schooling. Parents level of education is very much important for their children’s healthy food habit. Here, 92.18% of the respondent had a family history of atopy. A study shows that 316 (60%) of the 529 children had a history of atopic dermatitis. Girls and boys were both equally affected. In respondents whose spouses did not have a history of both respiratory atopy and atopic dermatitis, the incidence of affected children was 56% (180/321) [39]. There was a family history of atopic disease in 70.5% of respondents [40]. In our study about 4.30% of the respondents had lip or tongue swelling, 8.50% had difficulty swallowing, 39.30% had urticarial, 13.70% had dyspnea and 5.10% had anaphylaxis. Another study by Rance et al revealed that, 30% had urticaria and angio-edema, anaphylaxis in 4.5%, oral allergy syndrome (n=8; 1.4%), and gastrointestinal signs (n=11; 2%) [40]. Food allergies affect 4% to 6% of children, have become more common over the past ten years, and are therefore a significant burden on our children. According to research on the natural history of food allergies, reactions to cow's milk, eggs, and soy commonly go away while reactions to fish, almonds, and peanuts typically last into adulthood, though there are some exceptions [41]. Our study showed 48.6% of the respondents had allergy to Cow's Milk,19.5% to beef, 3.3% to egg ,2.6%to hilsa fish and prawn respectively, and 22.3% to others. In this study the mean Eosinophil was 11.62(±2.14), IgE was 747.40(±314.2). The skin prick test was positive 90.0% children
Conclusion
The predominant sign of food allergy in young children was atopic dermatitis. Allergic conjunctivitis, oral allergy syndrome and respiratory distress appeared later in the progression of symptoms. Additionally, anaphylaxis is usually used to affect older children.
Declaration
Funding
None.
Conflict of Interest
None declared.
Ethical approval
Ethical approval was obtained from the Institutional Review Board (IRB) of Institute of child and mother health (ICMH), Dhaka, Bangladesh.
References
- Vaillant AA, Modi P, Jan A. Atopy. InStatPearls (2021).
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Annals of nutrition and metabolism 66 (2015): 8-16.
- Ownby DR. Environmental factors versus genetic determinants of childhood inhalant allergies. J Allergy Clin Immunol 86 (1990): 279-287.
- Croner S, Kjellman N-IM. Development of atopic disease in relation to family history and cord blood IgE levels. Eleven-year follow-up in 1654 children. Pediatr Allergy Immunol 1 (1990): 14-20.
- Thomsen SF. Epidemiology and natural history of atopic diseases. European clinical respiratory journal 2 (2015): 24642.
- Badloe FM, De Vriese S, Coolens K, et al. IgE autoantibodies and autoreactive T cells and their role in children and adults with atopic dermatitis. Clinical and translational allergy 10 (2020): 1-5.
- Lazova S, Hristova D, Priftis S, et al. Food Sensitization Impact on Asthma Attacks in Children According to Age Group. Allergies 2 (2022): 44-56.
- Wong CY, Yeh KW, Huang JL, et al. Longitudinal Analysis of Total Serum IgE Levels with Allergen Sensitization and Atopic Diseases in Early Childhood. Sci. Rep 10 (2020): 21278.
- Brockow I, Zutavern A, Hoffmann U, et al. 3 Early Allergic Sensitizations and Their Relevance to Atopic Diseases in Children Aged 6 Years: Results of the GINI Study. Journal of investigational allergology & clinical immunology 19 (2009): 180.
- Workshops, Bousquet J, Van Cauwenberge P, et al. ARIA in the pharmacy: management of allergic rhinitis symptoms in the pharmacy: Allergic Rhinitis and its Impact on Asthma.
- Saarinen UM, Kajosaari M. Breastfeeding as prophylaxis against atopic disease: prospective follow-up study until 17 years old. The Lancet 346 (1995): 1065-1069.
- Kabir ML, Rahman F, Hassan MQ, et al. Asthma, atopic eczema and allergic rhino-conjunctivitis in school children. Mymensingh medical journal: MMJ 14 (2005): 41-45.
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Annals of nutrition and metabolism 66 (2015): 8-16.
- Chowdhury MA, Kabir AL, Alam MM. Allergic rhinitis, asthma and atopic diseases: Bangladesh perspective. Bangladesh Journal of Otorhinolaryngology 14 (2008): 66-70.
- Irani C, Maalouly G. Prevalence of self-reported food allergy in Lebanon: a middle-eastern taste. Int Scholar Res Notices. 2015 (2015).
- Sampson HA. Food allergy. Part 1: immunopathogenesis and clinical disorders. J Allerg Clin Immunol 103 (1999): 717-728.
- Koplin JJ, Allen KJ, Gurrin LC, et al. The impact of family history of allergy on risk of food allergy: a population-based study of infants. Int J Environ Res Public Health 10 (2013): 5364-5377.
- Le TT, Nguyen DH, Vu AT, et al. A cross-sectional, population-based study on the prevalence of food allergies among children in two different socio-economic regions of Vietnam. PediatrAllerg Immunol 30 (2019): 348-355.
- Han Y, Kim J, Ahn K. Food allergy. Korean J Pediatr 55 (2012): 153.
- Gupta RS, Kim JS, Barnathan JA, et al. Food allergy knowledge, attitudes and beliefs: focus groups of parents, physicians and the general public. BMC Pediatr 8 (2008): 36.
- Neeland MR, Koplin JJ, Dang TD, et al. Early life innate immune signatures of persistent food allergy. J Allerg Clin Immunol 142 (2018): 857-864.
- Voloshin S, Smoldovskaya O, Feyzkhanova G, et al. Patterns of sensitization to inhalant and food allergens among pediatric patients from the Moscow region (Russian Federation). PloS One 13 (2018): e0194775.
- Morita Y, Iwakura H, Ohtsuka H, et al. Milk allergy in the neonatal intensive care unit: comparison between premature and full-term neonates. Asia Pac Allerg 3 (2013): 35-41.
- Choi Y, Ju S, Chang H. Food allergy knowledge, perception of food allergy labelling, and level of dietary practice: a comparison between children with and without food allergy experience. Nutr Res Pract 9 (2015): 92-98.
- Skypala IJ, Venter C, Meyer R, et al. The development of a standardised diet history tool to support the diagnosis of food allergy. Clin TranslatAllerg 5 (2015): 1-0.
- Nowak-Wegrzyn A. New perspectives for use of native and engineered recombinant food proteins in treatment of food allergy. Immunol Allerg Clin North Am 27 (2007): 105-127.
- Gupta R, Siracusa M, Yarbrough M, et al. Parental therapy preferences for children with food allergy. In: Annals of allergy asthma and immunology. 360 Park Ave South, New York, NY 10010-1710 USA: Elsevier Science Inc 117 (2016): S104.
- Fiocchi A, Brozek J, Schünemann H, et al. World Allergy Organization (WAO) diagnosis and rationale for action against cow's milk allergy (DRACMA) guidelines. World Allerg Organ J 3(2010): 57-161.
- Hodge L, Yan KY, Loblay RL. Assessment of food chemical intolerance in adult asthmatic subjects. Thorax 51 (1996): 805-809.
- Boye JI. Food allergies in developing and emerging economies: need for comprehensive data on prevalence rates. Clin TranslatAllerg 2 (2012): 25.
- Peters RL, Gurrin LC, Dharmage SC, et al. The natural history of IgE-mediated food allergy: can skin prick tests and serum-specific IgE predict the resolution of food allergy? Int J Environ Res Public Health 10 (2013): 5039-5061.
- Ahanchian H, Jafari S, Behmanesh F, et al. Epidemiological survey of pediatric food allergy in Mashhad in Northeast Iran. Electron Phys 8 (2016): 1727.
- Prescott SL, Pawankar R, Allen KJ, et al. A global survey of changing patterns of food allergy burden in children. World Allerg Organ J 6 (2013): 1-2.
- Lee BW, Shek LP, Gerez IF, et al. Food allergy- lessons from Asia. World Allerg Organ J 1 (2008): 129.
- Lee AJ, Thalayasingam M, Lee BW. Food allergy in Asia: how does it compare? Asia Pac Allerg 3 (2013): 3-14.
- Branum AM, Lukacs SL. Food allergy among US children: trends in prevalence and hospitalizations.
- Upton E, Martin B, Wehmeyer A. Allergic Rhinitis: To Sneeze or to Wheeze. Pollen Is the Question, What Is the Answer? South African Pharm. J 85 (2018): 37-42.
- Cudowska B, Kaczmarski M. Atopy patch test in the diagnosis of food allergy in children with atopic eczema dermatitis syndrome. Roczniki Akademii Medycznej w Bialymstoku (1995). 50 (2005): 261-267.
- Uehara M, Kimura C. Descendant family history of atopic dermatitis. Acta dermato-venereologica 73 (1993): 62-63.
- Rance F, Kanny G, Dutau G, et al. Food hypersensitivity in children: clinical aspects and distribution of allergens. Pediatric Allergy and Immunology 10 (1999): 33-38.
- Zeiger RS. Dietary aspects of food allergy prevention in infants and children. Journal of pediatric gastroenterology and nutrition 30 (2000): S77-86.
