Astigmatoma
Article Information
Maryam Naser1, Parizad Hooshi2, Martin Mortazavi3, Danielle Westfal4, Wayne Schultheis4, Nafiseh Hashemi1*
1Hashemi Eye Care, Neuro-ophthalmology Clinic, Encino, CA, USA
2Northridge Specialty Imaging Center, CA, USA
3California Institute of Neuroscience, CA, USA
4Los Robles Hospital, Pathology Department, CA, USA
*Corresponding Author: Nafiseh Hashemi, MD, Hashemi Eye Care, Neuro-Ophthalmology Clinic, Encino, CA, USA
Received: 22 January 2021; Accepted: 02 February 2021; Published: 09 February 2021
Citation: Maryam Naser, Parizad Hooshi, Martin Mortazavi, Danielle Westfal, Wayne Schultheis, Nafiseh Hashemi. Astigmatoma. Journal of Ophthalmology and Research 4 (2021): 101-103.
View / Download Pdf Share at FacebookAbstract
Difficulty with reading may come from refractive errors including astigmatism, but also can arise from neurological disease causing difficulty focusing. We present a patient referred to neuro-ophthalmology clinic after initial treatment of astigmatism by Lasik was failed to address the patient’s main complaint.
Keywords
Astigmatoma; Lasik; Germinoma; Parinaud’s syndrome; Vertical gaze palsy; Nystagmus
Astigmatoma articles; Lasik articles; Germinoma articles; Parinaud?s syndrome articles; Vertical gaze palsy articles; Nystagmus articles
Article Details
Case Presentation
The patient is a 24-year-old Hispanic male. He noticed blurry vision and inability in focusing on words while reading in January 2019. The astigmatism corrective glasses was prescribed. Since he remained symptomatic, the patient underwent bilateral Lasik surgery in March 2019. A month after the procedure, his symptoms worsened with development of nystagmus and double vision.
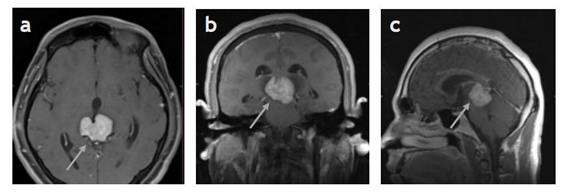
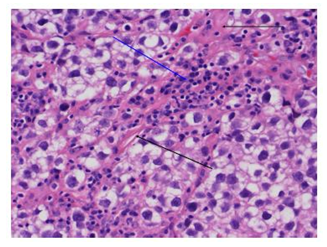
The patient presented to neuro-ophthalmology clinic with triad of Parinaud’s syndrome including collier lid retraction, limitation in elevation, and convergence retraction syndrome. He was complaining of mild headaches and could not look up. His past medical and surgical history were insignificant. He was not taking any medication. In eye exam, he had light-near dissociation and upward gaze palsy. The rest of eye exam including visual acuity, color vision, fundus exam, visual field and OCT optic nerve were within normal limits. MRI brain was performed which showed large posterior mid brain tumor (Figure 1). There was edema around the tumor. The pathology result confirmed the diagnosis of pure germinoma (Figure 2).
The patient had bleeding during the surgery and developed hemiparesis. Neurosurgery/Oncology team planned cranioplasty followed by decannulation and later radiation.
Discussion
Parinaud’s syndrome usually presents with abnormal motility in eye muscles and pupil dysfunction. The classic triad of upgaze paralysis, pupillary light-near dissociation and convergence retraction nystagmus are seen in most of patients [1]. The patient may express difficulty focusing on words while reading or jumping letters as in our case. Patients may complain of diplopia, difficulty looking up and blurred near vision. A thorough neurological examination, visual acuity, visual fields, color vision, pupillary examination and fundoscopy should be done in all patients. Neuroimaging, infection screening, serum protein electrophoresis, thyroid function tests and cerebrospinal fluid studies may also help with diagnosis. Pineal gland tumor is the most common and other midbrain pathologies such as vascular abnormalities, hemorrhage or infarction are less common causes. A team work between neurosurgery, pathology, ophthalmology and oncology are necessary for treatment of Parinaud’s syndrome. Up gaze palsy usually can be corrected surgically. The outcomes for patients depend on the cause.The most common etiology of Parinaud’s syndrome in children and young adults are neoplastic while in adults vascular disease are more common [2]. Germinoma should be considered in the differential diagnosis of midbrain lesions in young adults. MRI-guided stereotactic biopsy provides a helpful diagnostic information in patients with midbrain lesion. Koizumi., et al. presented a 29-year-old man with germinoma in midbrain who had diplopia and involvement of 3rd, 6th and 7th nerve treated by chemotherapy and radiotherapy [3]. long-term survival in patients with intracranial germinoma treated with low-dose radiotherapy alone has been promising [4,5]. Long-term follow-up in patients who receive radiation therapy is necessary for developing secondary tumors such as meningiomas, gliomas and cavernomas [6].
Conclusion:
Our purpose of reporting this case is making the readers familiar with different presentation of midbrain tumor. Any complaint of difficulty focusing on letters at near would require thorough motility and pupillary exam. Early diagnosis and prompt treatment with radiation and chemotherapy may improve the survival rate in patient with mid-brain tumor.
References
- Shields M, Sinkar S, Chan W, et al. Parinaud syndrome: a 25-year (1991–2016) review of 40 consecutive adult cases. Acta Ophthalmologica 95 (2017): e792-e793.
- Bradley WG. Bradley's neurology in clinical practice. Elsevier (2016).
- Koizumi H, Oka H, Utsuki S, et al. Primary germinoma arising from the midbrain. Acta Neurochirurgica 148 (2006): 1197-1200.
- Yen SH, Chen YW, Huang PI, et al. Optimal treatment for intracranial germinoma: can we lower radiation dose without chemotherapy?. International Journal of Radiation Oncology* Biology* Physics 77 (2010): 980-987.
- Cho J, Choi JU, Kim DS, et al. Low-dose craniospinal irradiation as a definitive treatment for intracranial germinoma. Radiotherapy and Oncology 91 (2009): 75-79.
- Osorio DS, Allen JC. Management of CNS germinoma. CNS oncology 4 (2015): 273-279.