Association of Serum Uric Acid with the Severity of Knee Osteoarthritis in a Tertiary Care Hospital
Article Information
Sarker S1*, Kamal T2, Dina NA3, Sharmin S4
1Department of Physical Medicine and Rehabilitation, MH Samorita Hospital and Medical College, Dhaka, Bangladesh
2Department of Physical Medicine and Rehabilitation, Dhanmondi Diagnostic and Consultation Centre, Dhaka, Bangladesh
3Department of Physical Medicine and Rehabilitation, National Healthcare Network, Dhaka, Bangladesh
4Department of Physical Medicine and Rehabilitation, Shaheed Monsur Ali Medical College, Dhaka, Bangladesh
*Corresponding Author: Supriya Sarker, Department of Physical Medicine and Rehabilitation, MH Samorita Hospital and Medical College, Dhaka, Bangladesh.
Received: 05 January 2023; Accepted: 22 January 2023; Published: 06 February 2023
Citation:
Sarker S, Kamal T, Dina NA, Sharmin S. Association of Serum Uric Acid with the Severity of Knee Osteoarthritis in a Tertiary Care Hospital. Journal of Orthopedics and Sports Medicine 5 (2023): 40-49.
View / Download Pdf Share at FacebookAbstract
Background: Osteoarthritis (OA) is the most common musculoskeletal condition and the most common cause of activity limitation among the middle aged and elderly population. Uric acid (UA) is constitutively present in normal cells, increased in concentration when cells are injured, and released from dying cells. Reaction of UA with oxidizing species generates UA radicals which is capable of causing biological damage. Several studies have previously showed an association between raised uric acid level and OA.
Objectives: The objectives of this study were to determine the correlation between serum uric acid level and radiological severity of knee osteoarthritis according to Kellgren-Lawrence grading. Methods: This was a cross sectional study done among 80 cases of knee osteoarthritis for the period from August 2017 to May 2018 in Department of Physical Medicine and Rehabilitation, Bangabandhu Sheikh Mujib Medical University, (Shahbagh, Dhaka). Correlation between serum uric acid level and severity of knee osteoarthritis was made by Spearman’s rho correlation. Continuous variables were tested with paired t-tests. Ordinal variables were tested with Wilcoxon signed rank test.
Results: Mean serum Uric Acid was 6.08 ± 1.11 mg/dl in male and 5.99 ± 0.97 mg/dl in female patients. Majority of the patients (42.5%) suffered from Grade 3 knee osteoarthritis radiologically. Maximum uric acid level was found (6.53 ± 1.54) in Grade 4 osteoarthritis. Mean Serum Uric acid Level was 5.85 ± 0.28 in Grade 3 and 5.52 ± 0.47 in Grade 2 knee osteoarthritis. Serum Uric acid level with severity of knee osteoarthritis Spearman’s rho correlation was done. There was significant correlation between severity of knee osteoarthritis and serum uric acid (rs= +0.288; p=0.013).
Keywords
Osteoarthritis; Serum uric acid; Kellgren-Lawrence grading
Physical medicine articles Physical medicine Research articles Physical medicine review articles Physical medicine PubMed articles Physical medicine PubMed Central articles Physical medicine 2023 articles Physical medicine 2024 articles Physical medicine Scopus articles Physical medicine impact factor journals Physical medicine Scopus journals Physical medicine PubMed journals Physical medicine medical journals Physical medicine free journals Physical medicine best journals Physical medicine top journals Physical medicine free medical journals Physical medicine famous journals Physical medicine Google Scholar indexed journals Rehabilitation articles Rehabilitation Research articles Rehabilitation review articles Rehabilitation PubMed articles Rehabilitation PubMed Central articles Rehabilitation 2023 articles Rehabilitation 2024 articles Rehabilitation Scopus articles Rehabilitation impact factor journals Rehabilitation Scopus journals Rehabilitation PubMed journals Rehabilitation medical journals Rehabilitation free journals Rehabilitation best journals Rehabilitation top journals Rehabilitation free medical journals Rehabilitation famous journals Rehabilitation Google Scholar indexed journals Osteoarthritis articles Osteoarthritis Research articles Osteoarthritis review articles Osteoarthritis PubMed articles Osteoarthritis PubMed Central articles Osteoarthritis 2023 articles Osteoarthritis 2024 articles Osteoarthritis Scopus articles Osteoarthritis impact factor journals Osteoarthritis Scopus journals Osteoarthritis PubMed journals Osteoarthritis medical journals Osteoarthritis free journals Osteoarthritis best journals Osteoarthritis top journals Osteoarthritis free medical journals Osteoarthritis famous journals Osteoarthritis Google Scholar indexed journals Synovial membrane articles Synovial membrane Research articles Synovial membrane review articles Synovial membrane PubMed articles Synovial membrane PubMed Central articles Synovial membrane 2023 articles Synovial membrane 2024 articles Synovial membrane Scopus articles Synovial membrane impact factor journals Synovial membrane Scopus journals Synovial membrane PubMed journals Synovial membrane medical journals Synovial membrane free journals Synovial membrane best journals Synovial membrane top journals Synovial membrane free medical journals Synovial membrane famous journals Synovial membrane Google Scholar indexed journals Subchondral bone articles Subchondral bone Research articles Subchondral bone review articles Subchondral bone PubMed articles Subchondral bone PubMed Central articles Subchondral bone 2023 articles Subchondral bone 2024 articles Subchondral bone Scopus articles Subchondral bone impact factor journals Subchondral bone Scopus journals Subchondral bone PubMed journals Subchondral bone medical journals Subchondral bone free journals Subchondral bone best journals Subchondral bone top journals Subchondral bone free medical journals Subchondral bone famous journals Subchondral bone Google Scholar indexed journals Articular cartilage articles Articular cartilage Research articles Articular cartilage review articles Articular cartilage PubMed articles Articular cartilage PubMed Central articles Articular cartilage 2023 articles Articular cartilage 2024 articles Articular cartilage Scopus articles Articular cartilage impact factor journals Articular cartilage Scopus journals Articular cartilage PubMed journals Articular cartilage medical journals Articular cartilage free journals Articular cartilage best journals Articular cartilage top journals Articular cartilage free medical journals Articular cartilage famous journals Articular cartilage Google Scholar indexed journals Subchondral osteonecrosis articles Subchondral osteonecrosis Research articles Subchondral osteonecrosis review articles Subchondral osteonecrosis PubMed articles Subchondral osteonecrosis PubMed Central articles Subchondral osteonecrosis 2023 articles Subchondral osteonecrosis 2024 articles Subchondral osteonecrosis Scopus articles Subchondral osteonecrosis impact factor journals Subchondral osteonecrosis Scopus journals Subchondral osteonecrosis PubMed journals Subchondral osteonecrosis medical journals Subchondral osteonecrosis free journals Subchondral osteonecrosis best journals Subchondral osteonecrosis top journals Subchondral osteonecrosis free medical journals Subchondral osteonecrosis famous journals Subchondral osteonecrosis Google Scholar indexed journals Osteophyte articles Osteophyte Research articles Osteophyte review articles Osteophyte PubMed articles Osteophyte PubMed Central articles Osteophyte 2023 articles Osteophyte 2024 articles Osteophyte Scopus articles Osteophyte impact factor journals Osteophyte Scopus journals Osteophyte PubMed journals Osteophyte medical journals Osteophyte free journals Osteophyte best journals Osteophyte top journals Osteophyte free medical journals Osteophyte famous journals Osteophyte Google Scholar indexed journals Joint margin articles Joint margin Research articles Joint margin review articles Joint margin PubMed articles Joint margin PubMed Central articles Joint margin 2023 articles Joint margin 2024 articles Joint margin Scopus articles Joint margin impact factor journals Joint margin Scopus journals Joint margin PubMed journals Joint margin medical journals Joint margin free journals Joint margin best journals Joint margin top journals Joint margin free medical journals Joint margin famous journals Joint margin Google Scholar indexed journals Knee articles Knee Research articles Knee review articles Knee PubMed articles Knee PubMed Central articles Knee 2023 articles Knee 2024 articles Knee Scopus articles Knee impact factor journals Knee Scopus journals Knee PubMed journals Knee medical journals Knee free journals Knee best journals Knee top journals Knee free medical journals Knee famous journals Knee Google Scholar indexed journals Hip articles Hip Research articles Hip review articles Hip PubMed articles Hip PubMed Central articles Hip 2023 articles Hip 2024 articles Hip Scopus articles Hip impact factor journals Hip Scopus journals Hip PubMed journals Hip medical journals Hip free journals Hip best journals Hip top journals Hip free medical journals Hip famous journals Hip Google Scholar indexed journals Lumbosacral articles Lumbosacral Research articles Lumbosacral review articles Lumbosacral PubMed articles Lumbosacral PubMed Central articles Lumbosacral 2023 articles Lumbosacral 2024 articles Lumbosacral Scopus articles Lumbosacral impact factor journals Lumbosacral Scopus journals Lumbosacral PubMed journals Lumbosacral medical journals Lumbosacral free journals Lumbosacral best journals Lumbosacral top journals Lumbosacral free medical journals Lumbosacral famous journals Lumbosacral Google Scholar indexed journals Spine articles Spine Research articles Spine review articles Spine PubMed articles Spine PubMed Central articles Spine 2023 articles Spine 2024 articles Spine Scopus articles Spine impact factor journals Spine Scopus journals Spine PubMed journals Spine medical journals Spine free journals Spine best journals Spine top journals Spine free medical journals Spine famous journals Spine Google Scholar indexed journals Tissue inflammation articles Tissue inflammation Research articles Tissue inflammation review articles Tissue inflammation PubMed articles Tissue inflammation PubMed Central articles Tissue inflammation 2023 articles Tissue inflammation 2024 articles Tissue inflammation Scopus articles Tissue inflammation impact factor journals Tissue inflammation Scopus journals Tissue inflammation PubMed journals Tissue inflammation medical journals Tissue inflammation free journals Tissue inflammation best journals Tissue inflammation top journals Tissue inflammation free medical journals Tissue inflammation famous journals Tissue inflammation Google Scholar indexed journals Distal finger joints articles Distal finger joints Research articles Distal finger joints review articles Distal finger joints PubMed articles Distal finger joints PubMed Central articles Distal finger joints 2023 articles Distal finger joints 2024 articles Distal finger joints Scopus articles Distal finger joints impact factor journals Distal finger joints Scopus journals Distal finger joints PubMed journals Distal finger joints medical journals Distal finger joints free journals Distal finger joints best journals Distal finger joints top journals Distal finger joints free medical journals Distal finger joints famous journals Distal finger joints Google Scholar indexed journals
Article Details
1. Introduction
Osteoarthritis is a progressive, immune mediated inflammatory disorder involving the entire joint structure including the synovial membrane, cartilage and subchondral bone. Osteoarthritis is characterized by focal loss of articular cartilage, subchondral osteonecrosis, osteophyte formation at the joint margin, and remodeling of joint contour with enlargement of affected joints. Osteoarthritis affects certain joints such as knee, hip, lumbosacral, spine. The proximal and distal inter phalangeal joints and base of the thumb are mostly affected and spare the wrist, elbow and ankle. It is the most common among the middle aged and elderly people. Arthralgia caused by osteoarthritis can seriously impact the quality of life. Osteophyte and joint space narrowing are the two typical radiographic features of osteoarthritis. Although still of uncertain etiology, there are many clinical factors that contribute to the risk and progression of OA, including obesity, joint mal-alignment, trauma, age, and female sex [1]. When cells are injured, the concentration of Uric Acid (UA) rises, and releases from dying cells [2]. On the basis of a theory proposed by Matzinger [3] the products of cell stress and tissue damage may represent “danger signals” that function as endogenous adjuvants recognized by the immune system. Matzinger [4] proposed that immunity is controlled by an internal factor between tissues and the cells of the immune system. This proposal introduced a new immunological model of an immune system capable of sensing cellular stress and tissue damage [5]. Shi subsequently identified uric acid as one of these principal endogenous danger signals released from injured cells and mediating the immune response to antigens associated with injured cells [2]. The molecular mechanism of this innate immune response to uric acid was further shown to be the result of the activation of the NALP3 inflammasome, a cytosolic, multiprotein complex that mediates caspase activation by uric acid crystals, leading to the production of the active forms of IL-1β and IL 18 [6]. Recently, Kono et al. [7] demonstrated in an in vivo hepatoxicity mouse model that uric acid is a physiological regulator of the inflammation induced by tissue injury values. These data form the basis for our hypothesis that uric acid is a factor regulating tissue inflammation, disease severity, and progression in Osteoarthritis (OA). Uric acid is best known for its role in gout. When uric acid concentrations exceed the limit of solubility (∼6.8 mg/dl or even lower under conditions of low pH or temperature), crystal formation can ensue, which is capable of activating the NALP3 inflammasome [6] and triggering the acute severe attacks of joint inflammation characteristic of gout [8]. Several studies have previously posited an association of uric acid and OA. These include a study of hip replacement patients where in elevated serum uric acid concentrations were associated with the presence of OA [9]. A second study noted the apparent co-localization of gout attacks and radiographic OA at a multitude of joint sites (big toe, midfoot, knee, and distal finger joints) and suggested that OA may facilitate the localized deposition of gout (monosodium urate or MSU) crystals [10]. The association with age, obesity, sex and metabolic factors has been studied [11-16]. All of these studies showed an association of osteoarthritis with obesity. Some of these studies accounted for serum uric acid and found no association between it and osteoarthritis [12-14,16]. Davis et al. [11] found a positive association between knee osteoarthritis and uric acid albeit a small one not reaching significant level. Sun et al. [17] specifically investigated serum uric acid relationship with osteoarthritis and concluded that although uric acid was associated with generalized osteoarthritis in patients undergoing hip replacement, there were no association with knee OA or bilateral hip or knee OA. Others reported an association with OA of multiple joints [18].
Reaction of UA with oxidizing species generates UA radicals which is capable of causing biological damage. To the best of my knowledge, no previous study has done to assess serum uric acid concentration with regard to radiographic OA features and severity in Bangladesh. So, in this study, we want to evaluate the potential association between levels of uric acid with severity of knee OA.
2. Materials and Methods
Serum uric acid level of patients presented with knee osteoarthritis was measured in biochemistry department and X-ray of affected joint Anterior posterior view standing position 100% SC view was done in radiology department of Bangabandhu Sheikh Mujib Medical University .At the same time synovial fluid was collected with all aseptic precaution and sent to Clinical Pathology Department for polarized light microscopy to exclude gout. All data was recorded systematically in a semi-structured questionnaire.
Patient with knee joint pain attending the outpatient department of Physical Medicine and Rehabilitation BSMMU, was registered as population for the study. A thorough history was taken from the registered patients and clinical examination of the patients was done which includes general examination and musculoskeletal examination to find out the cause of knee joint pain. Past history of illness and any systemic diseases was inquired cautiously. Patient who met the exclusion criteria were excluded. All symptoms and signs of each patient were recorded accordingly and clinical diagnosis was made. X-ray of affected joint and serum uric acid was done and at the same time synovial fluid from involved joint was taken out with all aseptic precaution and sent to clinical pathology lab for polarized light microscopy to exclude gout. Thus diagnosis of knee osteoarthritis was confirmed. A brief idea about the nature of study and intervention was delivered to each patient. Written informed consent was taken before entering into research.
All the data was compiled and sorted properly and the numerical data was analyzed statistically by using Statistical Package for Social Scientists (SPSS-18). The results were expressed as percentage and mean ± SD and P <0.05 will be considered as the level of significant. Correlation between hyperuracaemia and severity of knee osteoarthritis was made by Spearman’s rho correlation. Continuous variables were tested with paired t-tests. Ordinal variables were tested with Wilcoxon signed rank test.
3. Results
Table 1 shows baseline characteristics of the participants. Mean age of the male patients was 63.83 ± 10.72 and in female it was 62.86 ± 11.67 years. Mean BMI of male and female patients were 24.31 ± 1.50 and 24.47 ± 1.71 kg/m2successively. Mean ESR were 24.20 ± 5.80 in male and 28.80 ± 28.22 in female patients as well as Serum Uric Acid was 6.08 ± 1.11 mg/dl in male and 5.99 ± 0.97 mg/dl in female patients.
|
Male |
Female |
||
|
n (%) |
31 (38.8) |
49 (61.3) |
|
|
Age |
63.83 ± 10.72 |
62.86 ± 11.67 |
b0.694 |
|
BMI (kg/m2) |
24.31 ± 1.50 |
24.47 ± 1.71 |
a0.677 |
|
Systolic BP (mm of Hg) |
121.72 ± 3.84 |
123.49 ± 5.73 |
b0.145 |
|
Diastolic BP (mm of Hg) |
81.66 ± 4.41 |
82.33 ± 4.67 |
b0.303 |
|
Hb (g/dl) |
11.29 ± 1.14 |
11.11 ± 0.90 |
b0.538 |
|
ESR |
24.20 ± 5.80 |
28.80 ± 28.22 |
b0.842 |
|
Serum Uric Acid (mg/dl) |
6.08 ± 1.11 |
5.99 ± 0.97 |
b0.473 |
|
RBS (mmol/L) |
5.53 ± 0.20 |
5.46 ± 0.13 |
b0.498 |
|
Serum cratinine (mg/dl) |
1.06 ± 0.14 |
1.03 ± 0.22 |
b0.262 |
|
aUnpaired t test was done to measure the level of significance bMann Whitney U test was done to measure the level of significance |
|||
Table 1: Baseline characteristics of the Osteoarthritis patients (n=80).
|
Knee |
Frequency (n) |
Percentage (%) |
|
Left knee |
39 |
53.4 |
|
Right knee |
34 |
46.6 |
|
Total |
80 |
100 |
Table 2: Distribution of patients according to affected knee (n=80).
Table 2 shows 53.4% patients had left knee joint involvement and 46.6% patients had right knee joint involvement.
|
Frequency (n) |
Percentage (%) |
|
|
Grade 2 |
21 |
26.2 |
|
Grade 3 |
34 |
42.5 |
|
Grade 4 |
25 |
31.3 |
|
Total |
80 |
100 |
Table 3: Distribution of patients according to severity of knee Osteoarthritis (n=80).
Table 3 shows Majority of the patients (42.5%) suffered from Grade 3 knee osteoarthritis radiologically. 31.3% patients suffered from grade 4 and 26.2% patients showed Grade 2 severity of knee osteoarthritis.
|
Grade |
n (%) |
Serum Uric Acid (mg/dl) |
Min – max |
|
Mean ± SD |
|||
|
Grade 2 |
21 (26.2) |
5.52 ± 0.47 |
4.30 – 6.00 |
|
Grade 3 |
34 (46.6) |
5.85 ± 0.28 |
5.00 – 6.60 |
|
Grade 4 |
25 (34.2) |
6.53 ± 1.54 |
4.00 – 9.60 |
|
p value |
0.003 |
||
|
Kruskal Wallis test was done to measure the level of significance |
|||
Table 4: Serum Uric Acid at different grading of Osteoarthritis (n=80).
Table 4 shows Serum Uric Acid level in different grading of osteoarthritis of knee joint. Here, maximum uric acid level was found (6.53 ± 1.54) in Grade 4 osteoarthritis. Mean Serum Uric acid level was 5.85 ± 0.28 in Grade 3 and 5.52 ± 0.47 in Grade 4 knee osteoarthritis.
|
Grade |
Serum uric acid (mg/dl) |
p value |
|
|
≤ 7 |
>7 |
||
|
Grade 2 |
21 (28.8) |
0 (0.0) |
0.001 |
|
Grade 3 |
34 (46.6) |
0 (0.0) |
|
|
Grade 4 |
18 (24.7) |
7 (100.0) |
|
|
Chi-square test was done to measure the level of significance |
|||
Table 5: Serum Uric Acid at different grading of Osteoarthritis (n=80).
Table 5 shows that out of 25 patients of Grade 4 osteoarthritis 7 had uric acid >7 mg/dl. Rest of the patients of Grade 4 and all patients of Grade 2 and 3 had uric acid <7 mg/dl (Figure 1).
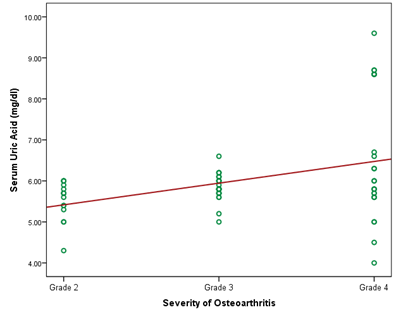
Figure 1: Correlation of severity of osteoarthritis with serum uric acid.
Spearman’s rho correlation was done. There is significant correlation between severity of osteoarthritis and serum uric acid (rs= + 0.288; p=0.013).
4. Discussion
OA is a progressive, inflammatory disorder in which one or more joints are affected. However, the knee joint is affected most, hence, the patients of Knee OA were included in our study. Out of 80 patients 31 were in the age group of >70 years and second highest prevalent group was 61-70 years that included 19 patients, a finding which is in concurrence with the global data, maximum numbers of reported patients are around 55 years of age [19]. In this study it was observed that the number of females was almost 2/3rd (61.3%) of the total number of patients. Although, there are few isolated reports that Knee OA is found more in males as compared to females [20], however, majority of studies have reported that the prevalence of Knee OA is more in females [21]. This study showed mean BMI of male and female patients were 24.31 ± 1.50 and 24.47 ± 1.71 kg/m2 successively, which is regarded as overweight for Asian population. Mean ESR were 24.20 ± 5.80 in male and 28.80 ± 28.22 in female patients as well as mean serum Uric Acid was 6.08 ± 1.11 mg/dl in male and 5.99 ± 0.97 mg/dl in female patients. In our study epidemiologic results particularly about greater prevalence of raised serum uric acid level among male are very much comparable with other previous studies. In our study, 53.4% patients had left knee joint involvement and 46.6% patients had right knee joint involvement. Among them, Majority of the patients (42.5%) suffered from Grade 3 knee osteoarthritis radiologically.31.3% patients suffered from grade 4 and 26.2% patients showed Grade 2 severity of knee osteoarthritis. Maximum uric acid level was found (6.53 ± 1.54) in Grade 4 osteoarthritis. Mean Serum Uric acid level was 5.85 ± 0.28 in Grade 3 and 5.52 ± 0.47 in Grade 2 knee osteoarthritis. Our study also found that, out of 25 patients of Grade 4 osteoarthritis 7 had uric acid >7 mg/dl, rest of the patients of Grade 4 and all patients of Grade 2 and 3 had uric acid < 7 mg/dl. To determine the correlation of Serum Uric acid level with severity of knee osteoarthritis Spearman’s rho correlation was done.
There was significant correlation between severity of knee osteoarthritis and serum uric acid (rs= +0.288; p=0.013).The levels of serum UA were also found to be increased in KL grade-III and grade IV patients as compared to KL grade-II patients and this increase was statistically significant. This showed that the rise in both the parameters was in parallel with the progression of the disease. A co-relation between rise in uric acid level and progression of knee osteoarthritis that was found in present study which is comparable to result of various previous studies [16,20,22]. Our study also showed the correlation of serum uric acid level with radiographic severity in knee osteoarthritis as measured by Kellgren-Lawrence osteoarthritis scale has been previously reported by Denoblea et al. [23]. That showed the strong association of uric acid level with severity of osteoarthritis of knee joint was advocated. In his study he quantified severity of osteoarthritis radiographically and scintigraphically and concluded that uric acid is a marker of disease severity. He also described strong possibility that uric acid may act as a promoting factor in the pathological process of osteoarthritis by activating the cascade of inflammation. Other possible explanatory mechanisms for the association between high serum uric acid levels and knee OA include genetic predisposition, and endogenous hormonal environment. Another reason for the observed association of uric acid level with osteoarthritis of knee joint in present study may be that we did not excluded patients already having diabetes and medications including diuretics which have been shown to be associated with osteoarthritis. The level of serum UA was found to be in increasing order, parallel to the grades of the disease. A probable mechanism of such UA related OA may be that the higher level of UA might lead to the formation of microcrystals in the joint space which is responsible for the commencement of inflammatory chain reaction leading to OA. Thus, it may be concluded that higher plasma UA levels have strong association with KOA. We observed that the severity of pain was parallel to the KL grade of the disease. As expected, the severity of pain was much more in patients with higher grades of disease. Among many inflammatory biochemical substances, possible association of UA with OA has been studied by many workers [24,25]. In the studies of late 20th century an association between raised UA levels and OA could not be established [26]. However, recent studies have shown correlation between higher UA levels and generalized OA/KOA [27,28]. Etiology of osteoarthritis is still doubtful but there are many physiological and clinical factors that may contribute to the risk and progression of osteoarthritis. These factors include obesity, joint deformity, trauma, age, and female sex [1]. The increase in both hyperuricemia and osteoarthritis in women after menopause indicate towards any possible hormonal mechanisms. Another Indian study by Mishra et al. [29] described correlation of elevated serum uric acid levels with laboratory and anthropometric parameters of various metabolic syndromes. They suggested that this may be due to high caloric diet, sedentary habits and greater prevalence of obesity unfortunately in our study we were unable to find any co-relation in dietary pattern and life style with the elevated serum uric acid level. Possible explanatory mechanism for association between hyperuricemia and osteoarthritis includes genetic predisposition, insulin resistance, and endogenous hormonal environment. The increase in both hyperuricemia and osteoarthritis in women after menopause may point to hormonal mechanisms. In conclusion, our data points to association between hyperuricemia and knee osteoarthritis.
5. Conclusion
In our study we found that there is a significant correlation between serum uric acid level and radiological severity of knee osteoarthritis. The level of serum UA was found to be in increasing order, parallel to the grades of the disease. We conclude that the presence of hyperuricaemia is associated with increased knee OA prevalence and severity in older men. While direction of the association between serum uric acid and OA is still unknown, and may be bi-directional. If Serum uric acid can be shown as a biomarker to predict future OA progression, it will help to identify high-risk subjects suitable for interventional trials like uratelowering therapy which may deserve future consideration.
6. Limitation and Recommendations
As it was a single center study. So, this study will not focus the entire population and further study recommended to focus entire population with facilities available in nearest possible area. Age groups of my study were 35-55. Usually osteoarthritis becomes more marked at the late age group. So this was one of limitation of this study. Further studies with more number of patients are needed for verification of various information collected from the present study
References
- Kraus VB, Vail TP, Worrell T, et al. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum 52 (2005): 1730-1735.
- Shi Y, Evans JE, Rock KL. Molecular identification of a danger signal that alerts the immune system to dying cells. Nature 425 (2003): 516-521.
- Matzinger P. Tolerance, danger, and the extended family. Annu Rev Immunol 12 (1994): 991-1045.
- Matzinger P. The danger model: A renewed sense of self. Science 296 (2002): 301-305.
- Pulendran B. Immune activation: Death, danger and dendritic cells. CurrBiol 14 (2004;): R30-R32.
- Martinon F, Pétrilli V, Mayor A, et al. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature 440 (2006): 237-241.
- Kono H, Chen C-J, Ontiveros F, et al. Uric acid promotes an acute inflammatory response to sterile cell death in mice. J Clin Invest 120 (2010): 1939-1949.
- Schumacher HR, Jr. The pathogenesis of gout. Cleve Clin J Med 75 (2008): S2-S4.
- Sun Y, Brenner H, Sauerland S, et al. Serum uric acid and patterns of radiographic osteoarthritis—the Ulm Osteoarthritis Study. Scand J Rheumatol 29 (2000): 380-386.
- Roddy E, Zhang W, Doherty M. Are joints affected by gout also affected by osteoarthritis? Ann Rheum Dis 66 (2007): 1374-1377.
- Davis MA, Ettinger WH, Neuhaus JM. The role of metabolic factors and blood pressure in the association of obesity with osteoarthritis of the knee. J Rheumatol 15 (1988): 1827-1832.
- Felson DT, Anderson JJ, Naimark A, et al. Obesity and knee osteoarthritis: The Framingham Study. Ann Int Med 109 (1988): 18-24.
- Bagge E, Bjelle A, Eden S, et al. Factors associated with radio-graphic osteoarthritis: Results from the population study: 70-year old people in Götenborg. J Rheumatol 18 (1991): 1218-1222.
- Schouten JSA, VandenOuweland FA, Valkenburg HA. A 12-year follow-up study in the general population on prognostic factors of cartilage loss in osteoarthritis of the knee. Ann Rheum Dis 51 (1992): 932-937.
- Hart DJ, Spector TD. The relationship of obesity, fat distribution and osteoarthritis in women in the general population: the Chingford Study. JRheumatol 20 (1993): 331-335.
- Hart DJ, Doyle DV, Spector TD. Association between metabolic factors and knee osteoarthritis in Women: the Chingford Study. J Rheumatol 22 (1995): 1118-1123.
- Sun Y, Brenner H, Sauerland S, et al. Serum uric acid and pattern of radiographic osteoarthritis: the U/M osteoarthritis study. Scand J Rheumatol 29 (2000): 380-386.
- Acheson R, Collart AB. New Haven survey of joint diseases XVII: Relationship between some systemic characteristics and osteoarthritis in a general population. Ann Rheum Dis 34 (1975): 379-387.
- Bannuru RR, Schmid CH, Kent DM, et al. Comparative Effectiveness of Pharmacologic Interventions for Knee Osteoarthritis: A Systematic Review and Network Metaanalysis. Ann Intern Med 162 (2015): 46-54.
- Al-Afraj AS. Serum uric acid and radiographic osteoarthritis. J Pak Med Assoc 53 (2003): 187-189.
- Al-Arfaj AS. Radiographic Osteoarthritis and Serum Triglycerides. Bahrain Medical Bulletin 25 (2003).
- Schouten JS, van den Ouweland FA, Valkenburg HA. A 12 year follow up study in the general population on prognostic factors of cartilage loss in osteoarthritis of the knee. Ann Rheum Dis 51 (1992): 932-937.
- Denoble AE, Huffman KM, Stabler TV, et al. Uric acid is a danger signal of increasing risk for osteoarthritis through inflammasome activation. Proceedings of the National Academy of Sciences of the United States of America 108 (2011): 2088-2093.
- Erden M, Ediz L, H?z O, et al. Effect of Colchicine on Total Antioxidant Capacity, Antioxidant Enzymes and Oxidative Stress Markers in Patients with Knee Osteoarthritis. International Journal of Clinical Medicine; 3 (2012): 377-382.
- Murakiy S, Dennisonz AE, Jamesonz K, et al. Association of vitamin D status with knee pain and radiographic knee Osteoarthritis. Osteoarthritis and Cartilage 19 (2011): 1301-1306.
- Krasnokutsky S, Oshinsky C, Attur M, et al. Serum urate levels predict joint space narrowing in non-Gout patients with medial knee osteoarthritis. Arthritis Rheumatol 69 (2017): 1213-1220.
- Ding X, Zeng C, Wei J, et al. 2016. The associations of serum uric acid level and hyperuricemia with knee osteoarthritis. Rheumatology International 1-7.
- Sun Y, Brenner H, Sauerland S, et al. Serum uric acid,and pattern of radiographic osteoarthritis: the U/M osteoarthritis study. Scand J Rheumatol 29 (2000): 380-386.
- Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J ClinEndocrinolMetab 93 (2008): S9-30.
