Association of CHA₂DS₂-VASc-HSF Score with Coronary Artery Disease Severity in Patients with Non-ST Segment Elevation Myocardial Infarction
Article Information
Md. Mostafa-Al-Rasel1*, Syed Nasir Uddin2,AbulKhair3, A K M Monwarul Islam3, Tariq Ahmed Chowdhury3, Md. Wareshuzzaman3, Md. Faisal Bin Selim Khan4, Syed Mahmud Ali5, Md. Rashidul Hassan6, Farida Parvin7
1Assistant Registrar (Cardiology), National Institute of Cardiovascular Diseases (NICVD), Dhaka, Bangladesh
2Professor (Cardiology), National Institute of Cardiovascular Diseases (NICVD), Dhaka, Bangladesh
3Associate Professor of Cardiology, National Institute of Cardiovascular Diseases (NICVD), Dhaka, Bangladesh
4Resident (Cardiology), National Institute of Cardiovascular Diseases (NICVD), Dhaka, Bangladesh
5Specialist & Registrar, Dept of Cardiology, Ibrahim Cardiac Hospital and Research Institute, Dhaka, Bangladesh
6Assistant Registrar (Cardiology), NITOR, Dhaka, Bangladesh
7Medical Officer (Pediatric Cardiology), National Institute of Cardiovascular Diseases & Hospital, Dhaka, Bangladesh
*Corresponding author: Md. Mostafa-Al-Rasel, Assistant Registrar(Cardiology), National Institute of Cardiovascular Diseases (NICVD), Dhaka, Bangladesh.
Received: 21 January 2025; Accepted: 29 January 2025; Published: 10 February 2025
Citation: Md. Mostafa-Al-Rasel, Syed Nasir Uddin, Mohammad Abul Khair, AKM Monwarul Islam, Tariq Ahmed Chowdhury, Md. Wareshuzzaman, Md. Faisal Bin Selim Khan, Syed Mahmud Ali, Md. Rashidul Hassan, Farida Parvin. Association of CHA₂DS₂-VASc-HSF Score with Coronary Artery Disease Severity in Patients with Non-ST Segment Elevation Myocardial Infarction. Cardiology and Cardiovascular Medicine. 9 (2025): 27-34.
View / Download Pdf Share at FacebookAbstract
Background and Objectives: Due to the wide spectrum of risk for death and recurrent events among patients with Non-ST Elevation Myocardial Infarction (NSTEMI), management guidelines emphasize the importance of early risk stratification. In addition to prognostic assessment, predicting the anatomical extension of coronary artery disease (CAD) is potentially useful for clinical decisions. The aim of the study was to determine whether the CHA2DS2-VASc-HSF score correlates with the angiographic extent and severity of CAD in patients with NSTEMI.
Methods: It was a cross-sectional observational study. A total of 80 patients with NSTEMI were enrolled. Based on the CHA2DS2-VASc- HSF score, the patients were divided into low (≤4) and high (>4) risk groups. All patients underwent coronary angiography during the index hospitalization and the severity of CAD was assessed by the SYNTAX score. The association between the CHA2DS2-VASc-HSF score and the SYNTAX score was evaluated.
Results: The mean age of patients was 50.58±9.53 and 54.48±10.66 years for group I and group II respectively with the majority (81.2%) being male. The mean CHA2DS2-VASc-HSF score of the patients was 2.68±0.92 in group I and 5.48±0.60 in group II (P value=<0.001). The median SYNTAX score was 7.50 (range 0.0 to 24.0) in Group I and 23.3 (range 0.0 to 39.0) in Group II (P value=<0.001). The CHA2DS2-VASc- HSF score was positively and significantly correlated with the SYNTAX score (Spearman’s ρ =0.703, p<0.001). A CHA2DS2-VASc-HSF score of 4.5 has 86.7% sensitivity and 72.0% specificity to detect severe coronary artery involvement (SYNTAX score >22).
Conclusion: The study demonstrated that the CHA2DS2-VASc-HSF score was associated with the severity of coronary artery disease in patients with NSTEMI. Notably, those with elevated CHA2DS2-VASc-HSF scores tended to have higher SYNTAX scores.
Keywords
CHA2DS2-VASc-HSF score; Coronary Artery Disease severity; Angiographic severity; SYNTAX score; NSTEMI; Bangladesh
CHA2DS2-VASc-HSF score articles; Coronary Artery Disease severity articles; Angiographic severity articles; SYNTAX score articles; NSTEMI articles; Bangladesh articles
Article Details
1. Introduction
Coronary artery disease (CAD), a form of atherosclerotic cardiovascular disease (CVD), is responsible for a significant global health burden, causing approximately 9.14 million deaths, which accounts for 16.2% of all global fatalities [1]. South Asians are particularly susceptible to CAD, exhibiting distinct characteristics, including early onset, increased severity, 2-4 times higher prevalence, incidence, hospitalization rates, and mortality, as well as a 5-10 year earlier occurrence of the first myocardial infarction (MI), along with a 5-10 times higher rate of MI and mortality before the age of 40 [2]. Bangladeshis are also at a heightened risk of CAD, experiencing early onset, rapid progression, and more severe angiographic presentations [3]. Ischemic heart disease (IHD) is the leading cause of death in Bangladesh, with acute myocardial infarction (AMI) being the leading cause (3.7% of deaths) across 504 public hospitals in the country in 2012 [4]. NSTEMI and UA are often grouped together under the term non-ST segment elevation acute coronary syndrome (NSTE-ACS) [5]. Globally, the prevalence of NSTEMI is rising compared to ST-elevation MI [6]. Patients with NSTEMI typically have more cardiac and non-cardiac comorbidities than those with STEMI [7]. Patients presenting with NSTE-ACS are at risk for adverse events such as death or recurrent infarction. While in STEMI management is clear and well defined, in patients with suspected NSTE-ACS early risk stratification is crucial to define the type of early management [8,9]. Therefore, identifying patients at high risk of developing major adverse cardiovascular events (MACEs) that may contribute to optimal management is crucial. Risk evaluation is important for the management of patients with ACS. Clinicians need simple, reliable, reproducible, and quantitative tools to identify patients’ risks and recommend prevention strategies. The Thrombolysis in Myocardial Infarction (TIMI) and Global Registry of Acute Coronary Events (GRACE) scoring systems used for the risk stratification of ACS patients are primarily based on multivariable models that include components of the medical history, admission electrocardiogram, and cardiac biomarker variables [10]. In our country, the association of risk score systems like GRACE and TIMI was evaluated with regard to angiographic scores [11]. Recently, the CHA2DS2-VASc-HS score has emerged as a novel predictor of CAD severity in stable CAD patients who have undergone diagnostic coronary angiography. In another study, the diagnostic accuracy of the CHA2DS2-VASc-HS score was compared with the TIMI and GRACE risk scores, revealing no significant differences [12]. In one study in our country, the CHA2DS2-VASc-HS score was found to be useful in predicting the risk of clinical adverse events in patients with NSTEMI [13]. In yet another study, the CHA2DS2-VASc-HSF score demonstrated a correlation with CAD severity and showed potential for predicting short-term prognosis [14]. In a study in our country, the CHA2DS2-VASc-HSF score positively correlated with the severity of CAD in patients presenting with ST-segment elevation myocardial infarction [15]. To the best of our knowledge, no study has been done to use this scoring model in predicting the severity of CAD in patients with NSTEMI in our country. The purpose of this study is to find out the utility of the CHA2DS2-VASC-HSF scoring system in predicting the angiographic extent and severity of CAD in patients with NSTEMI in our population. This score is practical, simple, and an easily remembered formula that includes multiple risk factors.
2. Methods and Materials
2.1 Study design: Cross-sectional observational study.
2.2 Place of study: This study was carried out in the Department of Cardiology, National Institute of Cardiovascular Diseases (NICVD), Dhaka, Bangladesh.
2.3 Study period: Study period was from September, 2022 to August, 2023.
2.4 Study population: On the basis of inclusion and exclusion criteria, NSTEMI patients admitted into NICVD who underwent coronary angiography during index hospitalization within the specified period of time were the study population.
2.5 The sample size was 40 in each group:
The study subjects were divided into two groups.
Group I: 40 patients, with lower CHA2DS2-VASc-HSF score (≤4)
Group II: 40 patients, with higher CHA2DS2-VASc-HSF score (>4)
Inclusion criteria:
- • Patients ≥ 18 years of either sex with NSTEMI undergoing coronary angiography at NICVD during index hospitalization.
Exclusion criteria:
Patients with the following conditions were excluded:
- • New left bundle branch block
- • History of prior CABG
- • Valvular heart diseases
- • Congenital heart diseases
- • Chronic Kidney disease with estimated glomerular filtration rate (eGFR) < 30 mL/m²/min
- • Severe liver disease
- • Advanced malignancy
- • Active infection
2.6 Study procedure:
- • All patients who were admitted in the Department of Cardiology, NICVD presenting with NSTEMI and fulfilling the inclusion criteria were the study subjects.
- • Informed written consent was taken from each patient before enrollment.
- • Meticulous history was taken and detailed clinical examinations were performed and recorded in a predesigned structured questionnaire.
- • Demographic data such as, age and sex were recorded.
- • Risk factors profile including smoking, hypertension, diabetes, hyperlipidemia, history of stroke or TIA, PVD, and family history of CAD were noted.
- • Laboratory investigations were done on index hospitalization: hs-Troponin I, serum creatinine, random blood sugar and serum electrolytes, CBC, Blood grouping, and screening blood tests. Automated Hormone Analyzer, Model- ACCESS 2 (Beckman Coulter, USA) assay was used for high sensitivity cTnI measurement (99th percentile cut-off value for males ≤ 0.020 ng/ml and females ≤ 0.012 ng/ml).
- • ECG: 12 lead resting ECG was done at a paper speed of 25 mm/s and 10 mm standardization at admission (model- iMAC 300, Wuhan Zoncare Bio-medical Electronics Co., Ltd, China).
- • Transthoracic echocardiography was done by an expert cardiologist before coronary angiography using the echocardiography machine (model- PHILIPS affiniti 30, country of origin-USA).
- • CHA2DS2-VASc-HSF scores were calculated where the presence of congestive heart failure 1 point, hypertension 1 point, age >75 years 2 points, diabetes mellitus 1 point, previous stroke or TIA 2 points, vascular disease 1 point, age 65–74 years 1 point, male gender 1 point, hyperlipidemia 1 point and smoker 1 point, Family history of CAD 1 point. The total score was 12 points.
- • Cut-off value of the CHA2DS2-VASc-HSF score were > The patients were categorized according to CHA2DS2-VASc-HSF score:
- • CHA2DS2-VASc-HSF score > 4 (High risk)
- • CHA2DS2-VASc-HSF score £ 4 (Low risk) [14]
- • Following standard protocol coronary angiography was carried out through a trans-femoral or trans-radial approach within the index hospitalization using the C-arm machine and Trinias system for Interventional Angiography, SHIMADZU (Origin-Japan).
- • All standard views were taken. In selected cases, additional views were taken.
- • Angiographic severity assessment was done by visual estimation. Two expert cardiologists who were blind to the ECG changes evaluated the CAG images.
- • Angiographic data were analyzed for the presence, extent, and severity of CAD. CAD severity was assessed by the SYNTAX score. All coronary lesions with diameter stenosis > 50% in vessels > 1.5 mm were scored, using the SYNTAX algorithm. The SYNTAX score calculator software version 2.11 (SYNTAX Score Working Group, www.syntaxscore.com) was used to calculate the SYNTAX score.
- • The SYNTAX score was defined as low if < 23, intermediate if 23 and 32, and high if >32. By this definition, patients with SYNTAX score ≥ 23 were considered to have moderate to severe CAD. Thus, the patients were divided into 2 groups:
- • low SYNTAX score (0–22)
- • Intermediate to high SYNTAX score (> 22) [16]
- • The comparison of the SYNTAX Score with the CHA2DS2-VASc-HSF Score was performed.
- • Data were presented in appropriate tables, graphs, charts, diagrams, etc., and were shown in the results section of the study.
2.7 Statistical Methods
- • The nature of the data was explored by exploratory data analysis.
- • Quantitative (continuous) data such as age were expressed as mean/ median and standard deviation and comparison was done by the “Student’s t” test and ‘Mann-Whitney-U’ test.
- • Qualitative (categorical) data such as DM, HTN, and smoking were expressed as frequency and percentage, and comparison was carried out by chi-square (χ2) Test.
- • The comparison of the CHA2DS2-VASc-HSF Score with the SYNTAX Score was performed.
- • Logistic regression analysis was done to adjust for the potential confounders in predicting angiographic severity among NSTEMI patients.
- • The Spearman correlation test was performed to determine the correlation between two continuous variables.
- • A P value <0.05 was considered as statistically significant.
- • Analysis was conducted by SPSS 26.0 for Windows software.
3. Results
Total 80 patients with NSTEMI were enrolled in this study after considering inclusion and exclusion criteria. A coronary angiogram was done within index hospitalization. Coronary angiograms were analyzed for the extent and severity of CAD using the SYNTAX score. Depending on the CHA2DS2-VASc-HSF score patients were divided into two groups.
- • Group I = CHA2DS2-VASc-HSF Score ≤4
- • Group II = CHA2DS2-VASc-HSF Score >4
- • SYNTAX score was calculated. The cut-off value of SYNTAX score was 22.
- • low SYNTAX score (0–22)
- • Intermediate to high SYNTAX score (> 22)
|
Age group (years) |
Group I (n=40) |
Group II (n=40) |
p-value |
|
21-30 |
0(0.0%) |
1(2.5%) |
|
|
31-40 |
8(20.0%) |
3(7.5%) |
|
|
41-50 |
14(35.0%) |
13(32.5%) |
|
|
51-60 |
14(35.0%) |
9(22.5%) |
|
|
61-70 |
3(7.5%) |
12(30.0%) |
|
|
>70 |
1(2.5%) |
2(5.0%) |
|
|
Total |
40(100.0%) |
40(100.0%) |
|
|
Mean±SD Range |
50.58±9.53 (35.00 - 72.00) |
54.48±10.66 (28.00 - 75.00) |
0.088 |
the P value obtained by Unpaired t-test, p<0.05 considered as a level of significance, SD-Standard Deviation
Group I = CHA2DS2-VASc-HSF Score ≤4, Group II = CHA2DS2-VASc-HSF Score >4
Table 1: Comparison of the study group according to age (N=80).
Table 1 shows the age distribution between the two groups. The most common age group among participants in both Group I and Group II was 41-50 years, with 35.0% in Group I and 32.5% in Group II. The mean age in Group I was 50.58 years (±9.53), and in Group II, it was 54.48 years (±10.66). There was no statistically significant difference between the two groups (p=0.088). In both groups, the majority of participants were male, constituting 80.0% of Group I and 82.5% of Group II. The remaining participants in 20% female in Group I and 17.5% in Group II. There was no statistically significant difference in sex distribution between two groups.
|
Cardiac risk factor |
Group I (n=40) |
Group II (n=40) |
P value |
|
Smoking |
12(30.0%) |
27(67.5%) |
<0.001 |
|
Hypertension |
22(55.0%) |
29(72.5%) |
0.104 |
|
Diabetes mellitus |
16(40.0%) |
28(70.0%) |
0.007 |
|
Hyperlipidemia |
5(12.5%) |
26(65.0%) |
<0.001 |
|
Family history of CAD |
6(15.0%) |
18(45.0%) |
0.003 |
|
Congestive Heart Failure |
4(10.0%) |
15(37.5%) |
0.004 |
|
History of stroke or TIA |
0(0.0%) |
4(10.0%) |
0.040 |
|
History of vascular disease |
2(5.0%) |
17(42.5%) |
<0.001 |
P value obtained by chi-square test, p<0.05 considered as a level of significance, CAD-coronary artery disease, TIA-Transient Ischaemic attack Group I = CHA2DS2-VASc-HSF Score ≤4, Group II = CHA2DS2-VASc-HSF Score >4
Table 2: Comparison of the study group according to the cardiovascular risk factors (N=80).
The above Table 2 describes risk factors among the studied patients, the highest percentage had a history of hypertension (72.5%), followed by diabetes mellitus (70.0%), smoking (67.5%), hyperlipidemia (65.0%), family history of CAD (45.0%), history of vascular disease (42.5%), congestive heart failure (37.5%), history of stroke or TIA (10.0%) in group II. The Table 2 also describes that there was a significant difference between the two groups in terms of diabetes mellitus (p=0.007), smoking (p=<0.001), hyperlipidemia (p=<0.001), family history of CAD (p=0.003), congestive heart failure (p=0.004), history of stroke (p=0.040s) and history of vascular disease (<0.001). It shows hypertension was higher in group II than in group I but statistically no significant difference (p>0.05).
|
Parameters |
Group I (n=40) |
Group II (n=40) |
P value |
|
Serum creatinine |
0.97±0.20 (0.40 - 1.30) |
1.04±0.17 (0.80 – 1.40) |
0.096 |
|
RBS |
7.71±2.19 (5.10 - 13.80) |
9.93±3.07 (4.90 - 14.80) |
<0.001 |
|
Serum Cholesterol |
174.43±7.76 (150.00 - 190.00) |
180.2±20.75 (105.00 - 220.00) |
0.104 |
|
Serum LDL |
89.85±18.00 (40.00 - 108.00) |
107.13±14.79 (36.00 - 128.00) |
<0.001 |
|
Serum HDL |
39.40±2.11 (35.00 - 43.00) |
38.91±3.50 (35.00 - 40.00) |
0.451 |
|
Serum TG |
150.23±9.05 (138.00 - 170.00) |
154.25±15.47 (135.00 - 190.00) |
0.160 |
P value obtained by chi-square test, p<0.05 considered as a level of significance, RBS-Random blood sugar, LDL-low density lipoprotein, HDL-High density lipoprotein, TG-triglycerides. Group I = CHA2DS2-VASc-HSF Score ≤4, Group II = CHA2DS2-VASc-HSF Score >4
Table 3: Distribution of study subjects by biochemical parameters (N=80).
Table 3 shows a comparative overview of biochemical parameters in two study groups. Group II exhibited significantly higher levels of RBS (9.93±3.07 vs. 7.71±2.19, p<0.001), serum LDL (107.13±14.79 vs. 89.85±18.00, p<0.001) compared to Group I. However, there were no statistically significant differences between the two groups in terms of serum creatinine (p=0.096), serum cholesterol (p=0.104), serum HDL (p=0.451), and serum triglycerides (p=0.160).
|
Coronary |
Group I (n=40) |
Group II (n=40) |
P value |
|
Right |
39(97.5%) |
38(95.0%) |
0.556 |
|
Left |
1(2.5%) |
2(5.0%) |
|
|
Co-dominant |
0(0.0%) |
0(0.0%) |
|
|
Total |
40(100.0%) |
40(100.0%) |
P value obtained by chi-square test, p<0.05 considered as a level of significance. Group I = CHA2DS2-VASc-HSF Score ≤4, Group II = CHA2DS2-VASc-HSF Score >4
Table 4: Demonstration of coronary dominance between study groups (N=80).
Table 4 shows a comparison of coronary dominance between the two study groups. In Group I, 97.5% of participants showed Right coronary dominance, while only 2.5% exhibited Left dominance. Group II had a similar distribution, with 95.0% displaying Right coronary dominance and 5.0% showing Left dominance. Notably, no participants in either group had Co-dominant coronary dominance. There was no statistically significant difference in coronary dominance between the two groups (p=0.556).
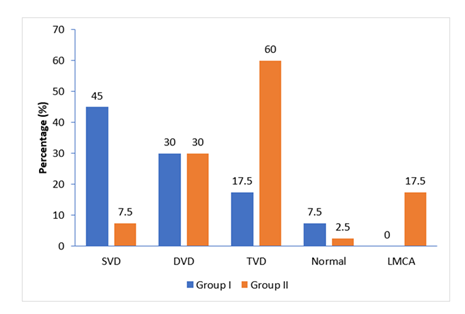
(SVD-single vessel disease, DVD-double vessel disease, TVD-triple vessel disease, LMCA-left main coronary artery)
Figure 1 presents a comparison of lesion severity between the two study groups. In Group I, 45.0% of the participants had SVD, while only 7.5% of Group II participants had SVD (p<0.001). Regarding DVDs, both groups had a similar prevalence of 30.0%. For TVD, Group I had a prevalence of 17.5%, while Group II had a prevalence of 60.0% which was statistically significant (p=0.001). The prevalence of normal lesions was 7.5% in Group I and 2.5% in Group II, with no significant difference between the two groups (p=0.305). In terms of LMCA disease, none of the participants in Group I had LMCA disease, while 17.5% of Group II participants had LMCA disease which was statistically significant (p=0.006).
|
Severity of lesion |
n |
CHA2DS2-VASc-HSF Score |
P value |
|
|
Mean±SD (N=80) |
Range (Min-Max) |
|||
|
SVD |
21 |
2.90±1.45 |
1.0 - 6.0 |
<0.001 |
|
DVD |
24 |
4.21±1.38 |
2.0 - 6.0 |
|
|
TVD |
31 |
4.97±1.20 |
2.0 - 7.0 |
|
|
Normal |
4 |
3.0±1.41 |
2.0 - 5.0 |
|
P value obtained by ANOVA test, p<0.05 considered as a level of significance. (SVD-single vessel disease, DVD-double vessel disease, TVD-triple vessel disease, SD-standard deviation, Min-minimum, Max-maximum)
Table 5: Relationship of the number of affected vessels and CHA2DS2-VASc-HSF Score (N=80).
The Table 5 shows that there is a significant difference in the mean CHA2DS2-VASc-HSF score between the different severity of lesions (p<0.001). Patients with TVD had the highest mean CHA2DS2-VASc-HSF score of 4.97±1.20, followed by patients with DVD with a mean score of 4.21±1.38 and SVD with a mean score of 2.90±1.45. Only 4 patients had normal results with a mean CHA2DS2-VASc-HSF score of 3.0±1.41.
|
Group I (n=40) |
Group II (n=40) |
P value |
|
|
CHA2DS2-VASc-HSF score |
|||
|
Mean±SD |
2.68±0.92 |
5.48±0.60 |
<0.001a |
|
Range |
1-4 |
5-7 |
|
|
SYNTAX score |
|||
|
Low Score (≤22) |
36(90.0%) |
14(35.0%) |
<0.001b |
|
Intermediate to high Score (>22) |
4(10.0%) |
26(65.0%) |
|
|
Mean±SD |
8.96±6.47 |
25.24±9.22 |
|
|
Median |
7.50 |
23.3 |
<0.001c |
|
Range |
0.0-24.0 |
0.0-39.0 |
P value obtained by aUnpaired t-test, bchi-square test, cMann-Whitney-U test and, SD-standard deviation, p<0.05 considered as a level of significance.
Group I = CHA2DS2-VASc-HSF Score ≤4, Group II = CHA2DS2-VASc-HSF Score >4
Table 6: Comparison of CHA2DS2-VASc-HSF score and SYNTAX score between the study groups (N=80).
Table 6 presents a comparison of the CHA2DS2-VASc-HSF score and SYNTAX score between two study groups (Group I and Group II). Regarding the CHA2DS2-VASc-HSF score, Group I had a mean score of 2.68±0.92, while Group II had a mean score of 5.48±0.60 (p<0.001). In Group I, 90.0% of the participants had a low SYNTAX score (≤22), while only 35.0% of Group II participants had a low SYNTAX score and the group difference was statistically significant (p<0.001). The median SYNTAX score was 7.50 (Range 0.0 to 24.0) in Group I and 23.3 (range 0.0 to 39.0) in Group II (P value=<0.001) (Figure 3).
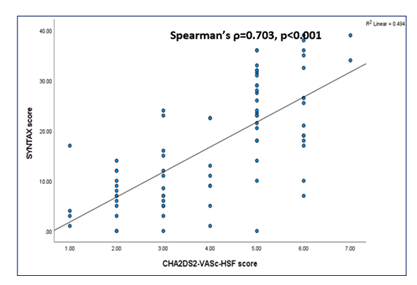
Figure 2 shows a strong positive correlation (ρ = 0.703) between the CHA2DS2-VASc-HSF score and the SYNTAX Score, which was statistically significant (p < 0.001). The higher the CHA2DS2-VASc-HSF score, the higher the SYNTAX score.
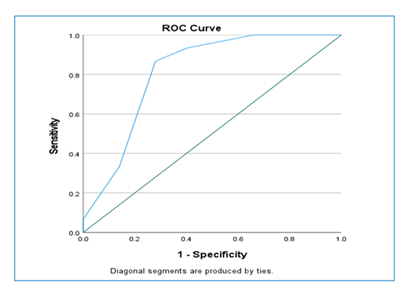
AUC-area under curve, SE-standard error, p<0.05 considered as a level of significance. ROC curve showed that a cut-off value of CHA2DS2-VASc-HSF score 4.5 had a sensitivity of 86.7%, and specificity of 72.0% to predict severity CAD. AUC was statistically significant (81.1%).
4. Discussion
The objective of the study was to investigate the association of CHA2DS2-VASc-HSF score with CAD severity. Following specific inclusion and exclusion criteria, this study involved 80 patients diagnosed with Non-ST-Segment Elevation Myocardial Infarction (NSTEMI), who were then categorized into two groups based on their CHA2DS2-VASc-HSF scores. Patients with a CHA2DS2-VASc-HSF score of ≤4 were designated as Group I, while those with a CHA2DS2-VASc-HSF score exceeding 4 were assigned to Group II. The defined cut-off point for the SYNTAX score was set at >22. In Group I, patients had an average age of 51 years, and in Group II, it was 55 years. No significant age difference was found between the two groups (P value = 0.088). Compared patients were younger, indicating a probable earlier onset of CAD in Bangladeshi individuals [13]. This study exhibited a significant male predominance, with a male-to-female ratio of 4:1. This finding aligns with similar studies, such as Cetin et al. [17] in which reported a 71% male frequency among study subjects. Male predominance in CAD has been consistently observed in various studies [12,16,18]. The higher prevalence of males in CAD studies may be influenced by factors such as limited healthcare access for females, particularly in low socioeconomic populations like our country [19]. Among the studied patients, hypertension was the most prevalent, followed by diabetes mellitus, smoking, hyperlipidemia, family history of CAD, history of vascular disease, and history of stroke in group II patients. Significantly higher rates of smoking, diabetes mellitus, hyperlipidemia, family history of CAD, history of stroke, and history of vascular disease were observed in group II compared to group I. A significant difference in smoking habits was observed between the two groups. This finding is in line with several studies that have reported similar disparities between smoker groups [14,17,20]. Sanlialp et al. [14] demonstrated that a family history of CAD was significantly higher in the high CHA2DS2-VASc-HSF score group than low CHA2DS2-VASc-HSF score group (30% vs. 13%, P value 0.006) which was consistent with this study. Sunman et al. [21] indicated that a family history of CAD is linked to the severity and extent of coronary atherosclerosis . In the present study, the history of stroke or TIA was higher in group II than in group I with a statistically significant difference (p=0.048) and was compatible with other studies [12,14,15,20]. Additionally, in a separate study, investigators pointed out that the risk of CAD was particularly elevated in stroke patients [22]. In this study, hyperlipidemia and vascular disease were higher in group II than in group I with a significant difference (P value <0.001 for both) which was compatible with another study Sanlialp et al. [14], although some other studies showed no significant difference Rahim et al. Uysal et al. [15,18]. Korkmaz et al. [23] found, there was a strong correlation between the degree of peripheral artery disease and the severity of coronary atherosclerosis. The mean LDL cholesterol and RBS levels were high in group II. These findings are consistent with other similar studies [12,14]. This significant difference in RBS and LDL is likely due to more diabetic and hyperlipidemic patients in the high-score group. However, serum creatinine levels showed no significant difference between the two groups, consistent with other studies [12,14,15,17]. In this study, the burden of atherosclerosis was evaluated by SYNTAX score. SYNTAX score was significantly higher in group II (Median 23.3) than in group I (Median 7.50) with a P value of <0.001. An almost similar result was demonstrated by another study where the SYNTAX score was 24±3 in the high SYNTAX score group and 12±2 in the low SYNTAX score group [18]. In another study, the SYNTAX score was 20.24±12.38 in the low-score group and 28.46±9.67 in the high-score group [14]. Rahim et al. [15] found a SYNTAX score of 28.6±4.5 in the high CHA2DS2-VASc-HSF score group and 11.4±5.8 in the low CHA2DS2-VASc-HSF group. It was found that the mean CHA2DS2-VASc-HSF score in group II was significantly higher than in group I (2.68±0.92 vs. 5.48±0.60, p=<0.001). The study also observed an increasing trend in the CHA2DS2-VASc-HSF score with higher SYNTAX scores. These findings align with previous research, including studies by Sanlialp et al. [14] and Tasolar et al. [12], which both reported a significant association between high SYNTAX scores and high CHA2DS2-VASc-HSF scores (6.00 vs. 3.50, P value <0.001 and 4.87±1.94 vs. 2.89±1.31, respectively). Similar trends were also noted in other studies [15,18]. Receiver operating characteristic (ROC) curve analysis determined that a CHA2DS2-VASC-HSF score of 4.5 is the optimal cut-off value for predicting CAD severity, with an area under the curve (AUC) of 0.811 and a 95% confidence interval (CI) ranging from 0.718 to 0.905 (P value 0.000). This cut-off value aligns with findings from other studies, including Cetin et al. [17], Taşolar et al. [12], and Sanlialp et al. [14]. In predicting the severity of CAD, CHA2DS2-VASc-HSF score with a cut-off value of 4.5 demonstrated a sensitivity of 86.7%, a specificity of 72.0%. These findings are consistent with studies by Cetin et al. [17] and Sanlialp et al. [14], which reported similar performance metrics. Bala et al. [13] and Taşolar et al. [12] found comparable results but focused on predicting major adverse cardiac events (MACE). This study established a significant positive correlation (Spearman's ρ = +0.703, p < 0.001) between the CHA2DS2-VASc-HSF score and the SYNTAX score, indicating that higher CHA2DS2-VASc-HSF scores were associated with increased CAD severity, as measured by the SYNTAX score. These findings align with similar strong correlations reported in other studies, including Sanlialp et al. [14] (r = 0.825, p < 0.001), Al-shorbagy et al. (r = 0.4811, p < 0.01), Rahim et al. [15] (r = 0.74, p < 0.001), and Taşolar et al. [12] (r = 0.474, p < 0.001). However, Uysal et al. [18] reported a weaker positive correlation (r = 0.271, p < 0.001) in their study. The main findings of this study were CHA2DS2-VASC-HSF score was independently associated with the severity of CAD in patients with NSTEMI. A high CHA2DS2-VASC-HSF score was significantly associated with an increased number of vessel involvement and a high SYNTAX score (P value <0.001). CHA2DS2-VASC-HSF score >4 predicts severe CAD assessed by SYNTAX score with 86.7% sensitivity and 72.0% specificity (AUC: 0.811, 95% CI: 0.718-0.905, P value 0.000). In clinical practice, straightforward risk scores are more appreciated during risk assessment. The ideal risk score should be easy to calculate and effective for rapid screening of high-risk patients to prevent adverse outcomes. This is why the CHA2DS2-VASC-HSF risk scoring systems may play an important role as predictive models. They are user-friendly for healthcare professionals and do not add extra costs to routine practice, making them practical risk assessment tools.
5. Conclusion
This study demonstrated a significant association between the CHA2DS2-VASC-HSF score and the severity of CAD in NSTEMI patients. Patients with higher CHA2DS2-VASC-HSF scores tended to have higher SYNTAX scores, indicating a more severe coronary artery disease.
6. Limitations
- • The sampling method used was not random but purposive, which introduces the potential for selection bias.
- • It's important to note that this study was limited to a single center and may not accurately reflect the broader population's characteristics and experiences.
- • Assessment of coronary angiography relied on visual observation, increasing the possibility of interobserver variation in the results.
- • The sample size was quite small, making it challenging to draw general conclusions from the findings.
7. Recommendations
- • The CHA2DS2-VASC-HSF score can be used as a valuable risk assessment tool for evaluating the prognosis and severity of CAD in NSTEMI patients.
- • To further investigate the relationship between the CHA2DS2-VASC-HSF score and CAD severity, large-scale, randomized, and multi-center studies are warranted.
References
- Brodmann M, Cahill TJ, Hil DP, et al. Global Burden of Cardiovascular Diseases. Journal of the American College of Cardiology 76 (2020): 2982-3021.
- Enas EA, Senthilkumar A. Coronary Artery Disease in Asian Indians: An Update and Review. J Cardiol 1 (2001).
- Islam AKMM, Majumder AAS. Coronary artery disease in Bangladesh: A review. Indian Heart Journal 65 (2013): 424-435.
- Al Mamun M, Rumana N, Pervin K, et al. Emerging Burden of Cardiovascular Diseases in Bangladesh. Journal of Atherosclerosis and Thrombosis 23 (2016): 365-375.
- Kumar A, Cannon CP. Acute Coronary Syndromes: Diagnosis and Management. Part I’. Mayo Clinic Proceedings 84 (2009): 917-938.
- Rosamond W, Flegal K, Friday G, et al. Heart Disease and Stroke Statistics—2007 Update. Circulation 115 (2007).
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology 64 (2014): 139-228.
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal 37 (2015): 267-315.
- Vrints CJM. The 12 lead ECG rules the waves in acute cardiovascular care. European Heart Journal: Acute Cardiovascular Care 7 (2018): 197-199.
- Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA 284 (2000): 835-842.
- Roy SS, Abu Azam STM, Khalequzzaman Md, et al. GRACE and TIMI risk scores in predicting the angiographic severity of non-ST elevation acute coronary syndrome. Indian Heart Journal 70 (2018): 250-253.
- Taşolar H, Çetin M, Ball M, et al. CHA2DS2-VASc-HS score in non-ST elevation acute coronary syndrome patients. Assessment of coronary artery disease severity and complexity and comparison to other scoring systems in the prediction of in-hospital major adverse cardiovascular events. Anatolian Journal of Cardiology 16 (2016): 742-748.
- Bala P, Rahman A, Ullah M, et al. Association CHA2DS2-VASc-HS Score with Adverse In-hospital Outcomes in Patients with Non-ST Segment Elevation Myocardial Infarction. Cardiovascular Journal 11 (2019): 159-166.
- Sanlialp SC, Nar G. The evaluation of the newly defined CHA2DS2-VASc-HSF score in the severity of coronary artery disease and short-term prognosis CHA2DS2-VASc-HSF score and coronary artery disease. Annals of Clinical and Analytical Medicine (2021): 1-6.
- Rahim MA, Uddin MJ, Jahan J, et al. Prediction of Coronary Artery Disease Severity by Using CHA2DS2-VASc-HSF Score in Patients with ST-Elevation Myocardial Infarction. Mymensingh Med J 32 (2023): 393-402.
- Seyis S, Gunay S, Rencuzoglu I. Relationship between platelet to lymphocyte ratio and coronary angiography timing in patients with NSTEMI. Biomedical Research 28 (2017): 8945-8950.
- Cetin M, Cakici M, Zencir C, et al. Prediction of coronary artery disease severity using CHADS2 and CHA2DS2VASc scores and a newly defined CHA2DS2-VASc-HS score. The American Journal of Cardiology 113 (2014): 950-956.
- Uysal OK, Turkoglu C, Duran M, et al. Predictive value of newly defined CHA2DS2-VASc-HSF score for severity of coronary artery disease in ST-segment elevation myocardial infarction. Kardiologia Polska 74 (2016): 954-960.
- Ahmed SM, Adams AM, Chowdhury M, et al. Gender, socioeconomic development and health-seeking behaviour in Bangladesh. Social Science & Medicine 51 (2000): 361-371.
- Modi R, Patted SV, Halkati PC, et al. CHA2DS2-VASc-HSF score - New predictor of severity of coronary artery disease in 2976 patients. International Journal of Cardiology 228 (2017): 1002-1006.
- Sunman H, Yorgun H, Canpolat U, et al. Association between family history of premature coronary artery disease and coronary atherosclerotic plaques shown by multidetector computed tomography coronary angiography’, International Journal of Cardiology 164 (2013): 355-358.
- Yoo J, Yang JH, Choi BW, et al. The frequency and risk of preclinical coronary artery disease detected using multichannel cardiac computed tomography in patients with ischemic stroke. Cerebrovascular Diseases (Basel, Switzerland) 33 (2012): 286-294.
- Korkmaz L, Adar A, Erkan H. Ankle-brachial index and coronary artery lesion complexity in patients with acute coronary syndromes. Angiology 63 (2012): 495-499.