Association between Primary School Children’s Unhealthful Behaviors and Overweight/Obesity: A Cross-Sectional Analysis in Urban Kenya
Article Information
Constance Awuor Gewa1*, Agatha Christine Onyango2, Rose Okoyo Opiyo3, Joel Gittelsohn4, Lawrence J Cheskin1
1Department of Nutrition and Food Studies, College of Health & Human Services, George Mason University, Fairfax, USA
2Department of Nutrition and Health, Maseno University, Maseno, Kenya
3School of Public Health, University of Nairobi, Nairobi, Kenya
4Department of International Health, Bloomberg School of Public Health, John Hopkins University, Baltimore, USA
*Corresponding Author: Constance Awuor Gewa, Associate Professor, George Mason University, College of Health & Human Services - Department of Nutrition & Food Studies, 4408 Patriot Circle, Suite 4100, MSN 1F7, Fairfax, VA 22030, USA
Received: 02 December 2021; Accepted: 10 December 2021; Published: 03 January 2022
Citation:
Constance Awuor Gewa, Agatha Christine Onyango, Rose Okoyo Opiyo, Joel Gittelsohn, Lawrence J Cheskin. Association between Primary School Children’s Unhealthful Behaviors and Overweight/Obesity: A Cross-Sectional Analysis in Urban Kenya. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 009-028.
View / Download Pdf Share at FacebookAbstract
We examined patterns of unhealthful dietary, PA and sleep behaviors among primary school children of different socio-economic status (SES) in two urban settings in Kenya and explored the association between these behaviors and overweight/obesity among the children. Data was collected on 390 children, aged 10-12 years, who attended public primary schools in two cities. Children’s anthropometric measurements were taken and parents, with the help of their children, completed questionnaires on children’s dietary, physical activity, and sleep behaviors. Body-mass-index-for-age z-scores, waist-circumference-to-height ratio, and the sum of skinfold measures were calculated. We utilized prevalence ratio analysis to examine the association between socio-economic/demographic characteristics, unhealthful behaviors and overweight/obesity. Overall, 21% of the children were overweight or obese and 9% had abdominal obesity. Prevalence of unhealthful behaviors varied significantly by child’s age, gender, school income levels, city, and frequency of consumption of restaurant foods. Children who consumed less than recommended amount of fruit servings had 1.68 times the risk of being overweight/obese, 2.49 times the risk of having abdominal obesity and 1.47 times the risk of having high total skinfold values compared to children with adequate fruit intake. Children with high frequency of consumption of red/processed meats had 1.50 times the risk of being overweight/obesity compared to children with less-frequent consumption. We found rather high prevalence of unhealthful behaviors among primary school children in Kenya, identified their determinants, and the association between specific behaviors and overweight/obesity. These results can guide childhood obesity prevention measures in Kenya and neighboring countries.
Keywords
School children, Overweight and obesity, Body-mass index, Waist circumference, Skinfold thickness, Dietary practices, Physical activity, Sleep, Kenya
Article Details
Abbreviations:
ANOVA: Analysis of variance; BAZ: Body mass index-for-age z-scores; BMI: Body Mass Index; NACOSTI: National Commission for Science, Technology and Innovation; PA: Physical activity; SES: Socio-economic status; SPANS: School Physical Activity and Nutrition Survey; SSB: sugar-sweetened beverages; TSKF: Total skinfold; USDA: United States Department of Agriculture; WC: Waist circumference; WHtR: Waist-circum- ference-to-height ratio
1. Introduction
Populations in East Africa are experiencing stage 1 of the obesity transition, characterized by an obesity prevalence of 5-14% among women, higher preva- lence of obesity among women compared to men and children, and among those with higher socio- economic status [1-4]. Although childhood obesity research in Kenya is still minimal, recent studies have reported an overweight/obesity prevalence of 19-20% among school children in Kenya, and the rise in childhood overweight/obesity seems to follow a socio-economic trend that is similar to that reported among reproductive age women [5, 6].
Unhealthful dietary habits, sedentary behaviors, inadequate physical activity (PA), and inadequate sleep have been shown to influence obesity rates among populations around the world [7-10]. How- ever, research on the association of these behaviors with childhood obesity in Kenya and in the region is still limited. A systematic review of dietary intake patterns among school children in developing nations reported an increasing trend towards consumption of calorie-dense foods in urban settings [11].
Studies on PA patterns have reported a shift in PA levels and modes of transportation, with differences shown between rural and urban populations and across socio-economic status and generations in Kenya [6, 12]. Research on the link between sleep and obesity has increased in high-income nations but not in lower-income nations [13]. We examined patterns of unhealthful dietary, PA and sleep behaviors among primary school children of different socio-economic status (SES) in two urban settings in Kenya and explored the association between these behaviors and overweight/obesity among the children.
2. Materials and Methods
Ethical approval and consent to participate This study was conducted according to the guidelines in the Declaration of All procedures involving human subjects were approved by the Office of Research Subject Protections at George Mason University (#1385824-3), Maseno University Ethics Review Committee (#MSU/DRP/MUERC/ 00679/19), and the National Commission for Science, Technology and Innovation (NACOSTI). Parental consent and child assent was obtained prior to commencing research study activities.
2.2 Participants
The study utilized a cross-sectional study design and was conducted in Kisumu and Nairobi cities, Kenya, in May-July 2019, giving us the opportunity to compare childhood obesity patterns and determinants across cities of different mean income and develop- ment levels. Nairobi is the capital of Kenya and has a total population of 4.4 million people [14]. Kisumu, the third-largest city in Kenya, has a population of 440,906 [14]. We identified public primary schools located within one Sub-County in each city. Each Sub-County was selected for their ease of access from the city center and presence of public primary schools that cater to children across different income levels. Public primary schools with higher costs of attendance predominantly cater to children from high-income households and vice-versa [15]. The highest enrolment public primary schools catering to children from low-, middle- and high-income house- holds in each Sub-County were identified, giving a total of three participating schools per Sub-County, referred to as low- middle- and high-income schools in the manuscript.
Details of children’s study sample size estimation are available in a previous publication [16]. Sixty-five to seventy children aged 10-12 years (grades 4-6) in each school were randomly selected to participate in the obesity research study.
2.3 Assessing children’s behaviors
Information on children’s dietary practices, sleep duration, engagement in PA and modes of transportation to and from school was collected via a questionnaire completed by parents with help from their children. The questionnaire was adapted from the NSW School Physical Activity and Nutrition Survey (SPANS) [17]. Lists of foods, drinks and food sources were updated to reflect foods/drinks and food sources in Kenya, and pretested prior to use. Questio- nnaires and written instructions were available in English and Kiswahili, and were sent to children’s parents in sealed envelopes. Four university gradua- tes (two per city) were trained to collect data. Resear- ch assistants telephoned parents to remind them to complete the questionnaire and to answer questions that arose.
Schoolchildren’s vegetable consumption was assess- ed using the question “How many servings of vegetables does your child usually eat at each meal (breakfast, lunch, dinner and snack) on each day?” Response options included “does not eat vegetabl- es”(coded 0), less than half serving (coded 0.25),one-half serving, one serving, two, three, four, five, and six servings or more (coded 6). A similar question and coding format was used to assess daily fruit consumption. Two-dimensional food models illustrating a one-half serving and one serving of vegetables and fruits were included with the questionnaire. Daily servings were calculated as the sum of servings consumed at each meal. Children who met the daily recommended vegetable and fruit servings were noted based on the United States Department of Agriculture (USDA) My Plate recommendations for individuals of their age and gender [18].
Frequency of consumption of red meats was assessed by asking parents to indicate how often their children consumed red meats and red meat products. Resp- onse options included “never or rarely” (recoded 0), “1-2 times per week” (recoded 1), “3-4 times per
week” (recoded 3), “5-6 times per week” (recoded 5) and “every day” (recoded 7). Consumption levels in the highest tercile were categorized as high- frequency consumption. Similar question and coding formats were used to assess frequency of consum- ption of fries/crisps, fried/baked wheat products, confectioneries, and restaurant foods.
Parents were asked to indicate the number of days in a week their child consumed plain water and sugar- sweetened beverages (processed juice, soda, flavored water and energy drinks), and the average amount of each drink consumed per day. Response options for amounts of drinks were based on a 250 ml cup. Two- dimensional food models illustrating a half cup and one cup were included with the questionnaire. Total weekly sugar-sweetened beverage (SSB) consum- ption levels within the highest tercile were categorized as high consumption levels.
Parents were asked to indicate the number of days their child used different transportation modes (walk/run, bicycle, motorcycle, car, and bus) to and from school. Parents also indicated the amount of time (hours or minutes) their child engaged in PA (cycling, running, jumping, playing football, swim- ming, skating, dancing, etc.) before and after school, and during the weekend. The amount of time spent on daily PA was calculated as the mean of the weekday and weekend averages. Children who did not walk/run to or from school on any school day nor meet the recommended sixty minutes of daily PA were noted [19]. Parents indicated their child’s “go- to-bed” and “wake-up” times on school and non- school days/nights. Hours of sleep were calculated. Children with a daily mean sleep duration below 9 hours were noted [20].
2.4 Anthropometric measurements
Children’s height, weight, skin-folds, and waist and hip circumferences were measured by trained research assistants at an assigned private location in each school. All measurements were taken in accordance with recommended procedures [21]. Body weights were measured barefoot, in light clothing and to the nearest 0.1 kg using a SECA 874 digital scale (SECA GmbH, Hamburg, Germany). Height measurements were taken without any foot or head wear and to the nearest 0.1 cm using a portable SECA 213 stadiometer (SECA GmbH, Hamburg, Germany). Body-mass index-for-age z-scores (BAZ) were calculated and classified as underweight (BAZ< -2), healthy weight (-2 ≤ BAZ ≤ 1), overweight (1< BAZ ≤ 2) and obese categories (BAZ > 2) [22]. Bicep, tricep, subscapular and suprailiac skinfold measurements were taken to the nearest 0.1 mm using Lange skinfold calipers (Beta Technology, Santa Cruz, CA, USA).
The sum of the four skinfold measures was used to estimate body fatness [23]. Sum of skinfold values within the highest tercile were categorized as high total skinfold (TSKF). Waist circumference (WC) was measured to the nearest 0.1 cm at the level of the umbilicus after normal expiration with an anthro- pometric, non-elastic measuring tape. The waist- circumference-to-height ratio (WHtR) was calculated and a WHtR above 0.5 was used to define abdominal obesity, and has proven a useful tool in evaluating cardiovascular health risks [24, 25].
2.5 Data analysis
Data analysis was performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). Anthropometric measurements and parent questionnaires were available for 390 children. Wilcoxon-Mann Whitney, one sample t-test and chi-squared statistics were used to compare unhealthful behaviors and overweight/ obesity status across cities. Kruskal Wallis, one-way ANOVA and chi-squared statistics were used to compare unhealthful behaviors and overweight/ obesity status across school income levels.
We utilized prevalence ratio (PR) multiple regression analysis to examine the association (i) between socio- economic and demographic characteristics (child- ren’s age, gender, and frequency of consumption of restaurant foods; city; school income level) and each behavior; (ii) between socio-economic/demographic characteristics and each overweight/obesity indicator (BAZ > 1, WHtR > 0.5, high TSKF) and (iii) between unhealthful behaviors and each overweight/ obesity indicator (BAZ > 1, WHtR > 0.5, high
TSKF). Results from regression analysis are reported as PR and corresponding 95% confidence intervals (CI). Each PR represents the risk of outcome (unhealthful behavior or overweight/obesity) that is associated with each independent variable, while controlling for other variables in the regression model.
3. Results
3.1 Socio-economic and demographic character- ristics
Children’s ages ranged from 8.45 to 14 years, with a mean of 11.28 ± 0.96 and a median of 11.28 years. Overall, 47% of the children resided in Nairobi, 42% were boys, and 35% were enrolled in low-income schools, 31% in middle-income schools and 34% in high-income schools.
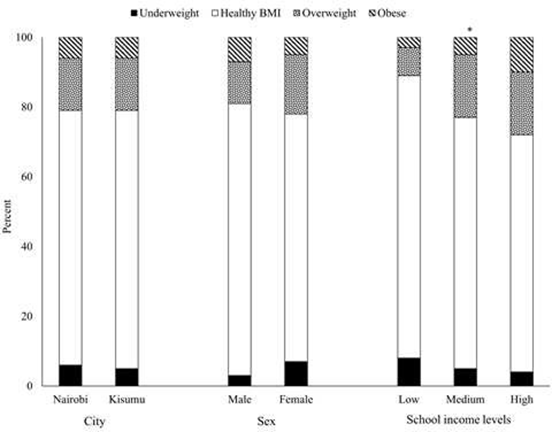
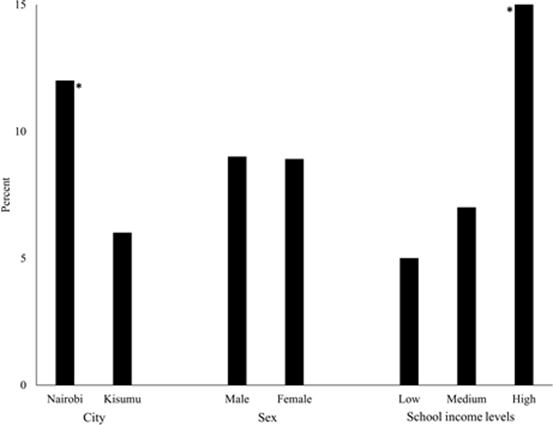
3.2 Overweight and obesity
There was a high correlation between children’s BAZ, WHtR and total SKF (rho ≥0.80). Overall, 5% of the children were stunted, and 21% were overweight or obese. Children’s mean WHtR was 0.44 ± 0.05 with a median of 0.43. Overall, 9% of the children had WHtR > 0.5. Prevalence of overweight/ obesity significantly varied across cities and school income levels (Figures 1 & 2). School children’s mean total skinfolds was 39.5 ± 21 mm, with a median of 32.5 mm.
3.3 Children’s behaviors
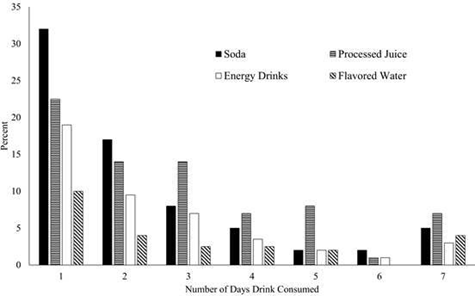
School children consumed a median of 2.3 servings of vegetable and 2.5 servings of fruits per day (Table 1). Overall, 28% and 42% of children did not meet the daily recommended vegetable and fruit servings, respectively. Frequency of consumption of confec- tioneries was significantly higher among children enrolled in schools in Kisumu compared to their counterparts in Nairobi. Frequency of consumption of red/processed meats was significantly higher among children enrolled in schools in Nairobi compared to Kisumu, as well as among children enrolled in high- income schools compared to low- and middle-income schools. Amounts of SSBs consumed per week was significantly higher among children enrolled in high- income schools. Thirty-five percent of children consumed soda one day per week while 5% consumed soda daily (Figure 3).
The percentage of children who did not walk to or from school varied across school income levels (5%, 80% and 80% in low-, middle and high-income schools respectively, p= <0.0001); 52% of the children did not meet recommended daily minutes of PA. The percentage of children who neither walked to/from school nor met recommended PA minutes varied across school income levels (1%, 44% and 40% in low-, middle- and high-income schools respectively, p= <0.0001). Overall, 41% of the children slept <9 hours per night with significant differences across school income levels (33%, 53% and 39% in low-, middle- and high-income schools, respectively (p= 0.0074).
3.4 Association between socio-economic and demographic characteristics and unhealthful behaviors
Each one-year increase in children’s age was associated with 1.17 times risk of children consuming high amounts of confectioneries/candies (Table 2). Male students were associated with 0.64 times risk of not walking to school nor meeting PA recommend- dations compared to females. Children in Nairobi had 0.73 times risk of consuming high amounts of confectioneries/candies but 1.73 times the risk of consuming high amounts of red/processed meats,compared to children in Kisumu.
Children in middle-income schools had 0.61 times the risk of consuming high amounts of fried/baked wheat products but 40 times the risk of not walking to school nor meeting PA recommendations and 1.57 times the risk of not getting recommended sleep hours compared to students in low-income schools. Children in high-income schools had 0.61 times the risk of consuming high amounts of fried/baked wheat products but 1.78 times the risk of consuming high amounts of SSBs, 1.97 times the risk of consuming high amounts of red/processed meats and 44 times the risk of not walking to school nor meeting PA recommendations compared to children in low- income schools.
Children with high frequency of consumption of restaurant foods had 1.87 times risk of consuming high amounts of SSBs, 1.94 times the risk of consuming high amounts of fries/crisps, 1.79 times the risk of consuming high amounts of confectioneries/candies and 2.02 times the risk of consuming high amounts of red/processed meats compared to children who consumed restaurant foods less-frequently.
3.5 Association between socio-economic and demographic characteristics and overweight/ obesity
Each one-year increase in students’ age was associated with 0.77 times the risk of having BAZ > 1 (Table 3). Male children had 0.55 times the risk of high total SKF compared to female children. Children in middle-income schools had 1.87 times the risk of having BAZ > 1 and 1.94 times the risk of having high total SKF compared to children in low- income schools. Children in high-income schools had 2.30 times the risk of having BAZ > 1, 2.69 times the risk of having WHtR > 0.5 and 1.97 times the risk of having high total SKF compared to children in low- income schools.
3.6 Association between unhealthful behaviors and overweight/obesity
Children who consumed less than recommended fruit servings had 1.68 times the risk of having BAZ > 1,2.49 times the risk of having WHtR > 0.5 and 1.47 times the risk of having high total SKF compared to children who consumed daily recommended fruit servings (Table 4). Children with high frequency of consumption of red/processed meats had 1.50 times the risk of having BAZ > 1 compared to students with less-frequent consumption of red/processed meats. 1Based on BMI-for-age z-score categories *P<0.05
1Based on WHtR values above 0.5
*P<0.05
Q2: median; SD: standard deviation; X? : mean
aChi-square test utilized to compare between-city and between-school income level percentages unless indicated otherwise: *P<0.05, **P<0.01, ***P<0.001,
****P<0.0001
bWilcoxon-Mann-Whitney test and t-test used to compare between-city values: *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001
cKruskal Wallis and one-way ANOVA tests used to compare between-school income level values: *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001
Table 1: Diet-related behaviors among primary school children in two cities in Kenyaa,b,c.
|
Unhealthful behavior and socio-economic and demographic characteristics |
PR |
CI |
|
Did not meet recommended daily vegetable intakea,c |
||
|
Child's age (years) |
1.05 |
(0.93, 1.20) |
|
Male student (ref=female student) |
1.21 |
(0.95, 1.54) |
|
Nairobi (ref=Kisumu) |
1.15 |
(0.90, 1.47) |
|
Middle-income school (ref=low-income school) |
0.98 |
(0.72, 1.34) |
|
High-income school (ref=low-income school) |
1.12 |
(0.84, 1.50) |
|
High frequency of eating restaurant foods (ref=low intake) |
0.81 |
(0.61, 1.08) |
|
Did not meet recommended daily fruit intakea,c |
||
|
Child's age (years) |
1.00 |
(0.84, 1.19) |
|
Male student (ref=female student) |
1.15 |
(0.83, 1.61) |
|
Nairobi (ref=Kisumu) |
1.03 |
(0.74, 1.44) |
|
Middle-income school (ref=low-income school) |
1.26 |
(0.84, 1.88) |
|
High-income school (ref=low-income school) |
1.00 |
(0.65, 1.51) |
|
High frequency of eating restaurant foods (ref=low intake) |
0.69 |
(0.46, 1.03) |
|
High intake of sugar-sweetened beveragesa,c |
||
|
Child's age (years) |
1.07 |
(0.92, 1.26) |
|
Male student (ref=female student) |
1.25 |
(0.93, 1.68) |
|
Nairobi (ref=Kisumu) |
0.81 |
(0.60, 1.10) |
|
Middle-income school (ref=low-income school) |
1.07 |
(0.69, 1.67) |
|
High-income school (ref=low-income school) |
1.78** |
(1.21, 2.62) |
|
High frequency of eating restaurant foods (ref=low intake) |
1.87**** |
(1.40, 2.50) |
|
High frequency of consuming of fries/crispsa,c |
||
|
Child's age (years) |
1.12 |
(0.93, 1.36) |
|
Male student (ref=female student) |
0.96 |
(0.68, 1.37) |
|
Nairobi (ref=Kisumu) |
0.87 |
(0.61, 1.25) |
|
Middle-income school (ref=low-income school) |
0.79 |
(0.52, 1.20) |
|
High-income school (ref=low-income school) |
0.85 |
(0.56, 1.28) |
|
High frequency of eating restaurant foods (ref=low intake) |
1.94*** |
(1.37, 2.73) |
|
High frequency of consuming of baked/fried wheat productsa,c |
||
|
Child's age (years) |
1.16 |
(0.98, 1.37) |
|
Male student (ref=female student) |
0.89 |
(0.65, 1.22) |
|
Nairobi (ref=Kisumu) |
0.87 |
(0.63, 1.19) |
|
Middle-income school (ref=low-income school) |
0.61* |
(0.41, 0.89) |
|
High-income school (ref=low-income school) |
0.61** |
(0.43, 0.88) |
|
High frequency of eating restaurant foods (ref=low intake) |
1.25 |
(0.92, 1.71) |
|
High frequency of consuming of confectioneries/candiesa,c |
||
|
Child's age (years) |
1.17* |
(1.01, 1.35) |
|
Male student (ref=female student) |
0.79 |
(0.60, 1.03) |
|
Nairobi (ref=Kisumu) |
0.73* |
(0.55, 0.96) |
|
Middle-income school (ref=low-income school) |
1.12 |
(0.80, 1.57) |
|
High-income school (ref=low-income school) |
1.17 |
(0.85, 1.61) |
|
High frequency of eating restaurant foods (ref=low intake) |
1.79**** |
(1.40, 2.30) |
|
High frequency of consuming of red or processed meatsa,c |
||
|
Child's age (years) |
1.04 |
(0.90, 1.22) |
|
Male student (ref=female student) |
0.91 |
(0.68, 1.20) |
|
Nairobi (ref=Kisumu) |
1.73*** |
(1.30, 2.29) |
|
Middle-income school (ref=low-income school) |
1.23 |
(0.80, 1.88) |
|
High-income school (ref=low-income school) |
1.97*** |
(1.39, 2.81) |
|
High frequency of eating restaurant foods (ref=low intake) |
2.02**** |
(1.54, 2.64) |
|
Neither walked to school nor met PA recommendationsb,c |
||
|
Child's age (years) |
1.15 |
(0.98, 1.35) |
|
Male student (ref=female student) |
0.64* |
(0.46, 0.89) |
|
Nairobi (ref=Kisumu) |
1.29 |
(0.96, 1.74) |
|
Middle-income school (ref=low-income school) |
48.0*** |
(7.00, 343) |
|
High-income school (ref=low-income school) |
44.0*** |
(6.00, 316) |
|
Slept less than 9 hours per dayb,c |
||
|
Child's age (years) |
1.08 |
(0.95, 1.24) |
|
Male student (ref=female student) |
0.99 |
(0.78, 1.27) |
|
Nairobi (ref=Kisumu) |
0.90 |
(0.70, 1.16) |
|
Middle-income school (ref=low-income school) |
1.57** |
(1.16, 2.13) |
|
High-income school (ref=low-income school) |
1.99 |
(0.86, 1.65) |
CI: confidence interval; PA: physical activity; PR: prevalence ratio
aMultiple regression model includes child’ age and sex, city, school income level and high frequency of consuming restaurant
food as independent variables and unhealthful behavior as dependent variable.
bMultiple regression model includes child’ age and sex, city and school income level as independent variables and unhealthful behavior as dependent variable.
cPR and associated CI from each row represent association between each independent variable and unhealthful behavior while controlling for other variables within the model: *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001
Table 2: Association between socio-economic, demographic characteristics and unhealthful behaviors among primary school children in urban Kenya (n=390)a,b,c.
|
Socio-economic demographic characteristics |
BAZ > 1 |
WHtR > 0.5 |
High Total SKF |
|||
|
PR |
CI |
PR |
CI |
PR |
CI |
|
|
Child's age (years) |
0.77* |
(0.62, 0.96) |
0.73 |
(0.52, 1.03) |
0.95 |
(0.83, 1.10) |
|
Male student (ref=female student) |
0.89 |
(0.59, 1.31) |
0.97 |
(0.52, 1.81) |
0.55*** |
(0.40, 0.76) |
|
Nairobi (ref=Kisumu) |
0.98 |
(0.66, 1.46) |
1.71 |
(0.88, 3.32) |
0.98 |
(0.74, 1.29) |
|
Middle-income school (ref=low-income school) |
1.87* |
(1.05, 3.31) |
1.20 |
(0.45, 3.19) |
1.94** |
(1.29, 2.90) |
|
High-income school (ref=low-income school) |
2.30** |
(1.33, 3.97) |
2.69 * |
(1.18, 6.13) |
1.97** |
(1.31, 2.94) |
|
High frequency of eating restaurant foods (ref=low intake) |
1.07 |
(0.71, 1.62) |
0.68 |
(0.32, 1.45) |
1.2 |
(0.91, 1.58) |
BAZ: body mass index-for age z-score, CI: confidence interval; PR: prevalence ratio; SKF: skinfold; WHtR: waist circumference: height ratio
aMultiple regression model includes child's age and sex, city, school income level and high frequency of consuming restaurant food as independent variables and obesity indicator as dependent variable
bFor each obesity indicator: PR and associated CI from each row represent association between independent variable and obesity indicator while controlling for other variables within the model; *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001
Table 3: Association between socio-economic and demographic characteristics and overweight/obesity among primary school children in urban Kenya (n=390)a,b.
|
Unhealthful behavior |
BAZ > 1 |
WHtR > 0.5 |
High Total SKF |
|||
|
PR |
CI |
PR |
CI |
PR |
CI |
|
|
Did not meet recommended daily vegetable intake (ref=met intake recommendation)a |
1.32 |
(0.89, 1.95) |
1.24 |
(0.66, 2.32) |
1.02 |
(0.77, 1.36) |
|
Did not meet recommended daily fruit intake (ref=met intake recommendation) 2 |
1.68 ** |
(1.14, 2.47) |
2.49 ** |
(1.36, 4.58) |
1.47* * |
(1.12, 1.92) |
|
High intake of SSBs (ref=medium or low level of SSBs intake)a |
1.01 |
(0.64, 1.58) |
1.15 |
(0.56, 2.39) |
0.94 |
(0.67, 1.30) |
|
High frequency of consuming of chips/crisps (ref=medium or low frequency)a |
1.08 |
(0.69, 1.69) |
1.01 |
(0.48, 2.15) |
1.11 |
(0.82, 1.51) |
|
High frequency of consuming of fried/baked wheat products (ref=medium or low frequency)a |
0.73 |
(0.45, 1.20) |
0.75 |
(0.34, 1.64) |
0.86 |
(0.63, 1.19) |
|
High frequency of consuming of confectioneries (ref=medium or low frequency)a |
0.68 |
(0.43, 1.07) |
0.47 |
(0.49, 1.92) |
0.87 |
(0.65, 1.18) |
|
High frequency of intake of red or processed meats (ref=medium or low frequency)a |
1.50 * |
(1.01, 2.25) |
1.88 |
(0.96, 3.69) |
1.15 |
(0.85, 1.55) |
|
Neither walked to school nor met PA recommendations (ref=walked to school and/ or met PA recommendation)b |
1.03 |
(0.66, 1.61) |
1.05 |
(0.52, 2.11) |
1.02 |
(0.75, 1.38) |
|
Slept less than 9 hours of sleep per day (ref=slept at least 9 hours per day)b |
1.09 |
(0.74, 1.63) |
1.18 |
(0.62, 2.29) |
1.19 |
(0.90, 1.57) |
BAZ: body mass index-for age z-score, CI: confidence interval; PA: physical activity; PR: prevalence rate ratio; SSBs: sugar- sweetened beverages; SKF: skinfold; WHtR: waist circumference: height ratio
aFor each obesity indicator: PR and associated CI from each row represent association between unhealthful behavior and obesity indicator while controlling for child's age and sex, city, school income level, and frequency of consumption of restaurant foods;
*P<0.05, **P<0.01, ***P<0.001, ****P<0.0001
bFor each obesity indicator: PR and associated CI from each row represent association between unhealthful behavior and obesity indicator while controlling for child's age and sex, city and school income level; *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001
Table 4: Association between unhealthful behaviors and overweight/obesity among primary school children in urban in Kenya (n=390)a,b.
4. Discussion
Research has shown that overweight and obese children are more likely to become obese adults and suffer higher risks for obesity-related comorbidities [26]. Although the overall prevalence of overweight/ obesity found in this study is similar to that reported in previous studies conducted among primary school children in Kenya, our study showed that overweight/ obesity increased with income levels [5, 6]. The findings of the current study were strengthened by the use of multiple indicators of obesity. The percentage of children with BAZ > 1 was higher than reported in Ethiopia and Tanzania, but lower than that reported in a higher-income nation like South Africa [27-30]. Overall, the median WHtR and TSK in the current study was similar to those of school children in Norway and South Africa [23, 31, 32].
The percentage of children who consumed recommended amounts of fruits was similar to that reported among adolescents in Tanzania, Malawi and the Seychelles, but higher than adolescents in Ethiopia, Benin, Botswana, Ghana, Mauritania, Senegal, Sudan, Swaziland and Zambia [27, 28, 33]. Vegetable intake levels were higher than that among adolescents in more than ten African nations [33]. The average fruit and vegetable servings reported in this study were higher than previously reported among older children and adults in Kenya, and much higher than that reported among 9-13 year old children in the US [34, 35]. We found that children who did not consume recommended levels of fruit were significantly more likely to be overweight/ obese, have central obesity, and high levels of adipose tissue. Murage et al. reported a negative association between fruit and vegetable consumption and overweight or obesity among adult men in poorer urban settings in Kenya [36]. Experimental and prospective studies, for the most part, have shown an inverse relationship between fruit consumption and weight gain, overweight and obesity among adults [37-42]. This relationship may be attributed to multiple factors, including decreased dietary energy density, increased satiety and satiation, and increased intake of polyphenols, all of which have anti-obesity properties [43, 44].
Our study showed that high consumption of red/processed meats was associated with a significantly higher proportion of overweight/obesity. This is consistent with previous studies. Studies among adults in the US have shown that meat consumption is positively associated with obesity and central obesity [45]. Other studies have shown that processed meats, but not unprocessed meats, are associated with obesity and poor health outcomes [46-49]. Consuming higher amounts of meat and an animal-driven nutrient pattern was positively associated with higher risks of overweight/obesity among children in Ethiopia and South Africa [28, 50]. The list of red meats examined in our study consisted mostly of processed red meats. In Kenya, beef and goat meat were the most consumed meats in high- and middle-income households, fish was most- consumed in low-income households, while sausages were the most preferred processed meats with consumption levels rising with income [51]. Our findings follow a similar income/economic pattern showing that high frequency of consumption of red/processed meats was significantly higher among children in middle and high-income schools compared to children in low-income schools and among children in Nairobi compared to children in Kisumu. Nairobi is a larger city with higher economic power [14].
Overall, SSB intake levels were similar to those reported among children in Malawi, but lower than that reported in South Africa, US and Europe [52- 54]. Intake of SSBs, fries/crisps, baked/fried wheat products and confectionaries were not significantly associated with overweight/obesity in this group of children. The lack of significant association in our study may be due to multiple factors, including differences in study design, intake estimation methods and food group classification [55].
Longitudinal studies have reported a positive association between ultra-processed foods and body fat levels, and frequent consumption of fried foods have been associated with higher risk of obesity [56- 59]. Our findings show that income and consumption of restaurant foods were significant predictors of multiple unhealthful dietary behaviors among school children in Kenya. Children in higher income schools were likely to consume more SSBs and processed meats. However, they were least likely to consume fried/baked wheat products. Children in low-income schools may have more access to the more affordable fried wheat products like mandazi and chapatti [60]. Consumption of foods prepared outside the home has been on the rise in many developing countries [61]. However, as our findings have shown, children with high frequency of consumption of restaurant foods were significantly more likely to consume high amounts of SSBs, fries/crisps and confectioneries. Percentage of children who did not walk to school nor meet PA recommendations varied across income levels. However, neither PA nor mode of transportation was associated with overweight/ obesity among this group of children. Studies that have examined the association between PA and overweight/obesity among school children in Africa have overall shown mixed results [27, 29, 62].
4.1 Study strengths and limitations
The study’s strengths are inclusion of children from three different income levels, use of multiple obesity measures, and examination of multiple behaviors. However, it suffers certain limitations. The small number of schools and their purposeful selection may limit generalizability of results; we utilized school- level income categories, yet some children may come from households outside of these income categories; risk factors and outcomes were measured simultaneously making it difficult to determine sequence of event and the recall of children’s behaviors may be affected by recall bias.
4.2 Future research recommendations
We recommend that future studies include a larger number of schools, utilize household-based income indicators, utilize study designs and methodologies that minimize recall bias and uncertainty in temporal sequence of risk factors and outcomes, and explore utilization of more standardized categories of behaviors.
5. Conclusions
Findings of this study contribute to the emerging literature on childhood obesity in Africa. This study highlights the high prevalence of unhealthful behaviors, determinants of these behaviors, and the association between unhealthful behaviors and overweight/obesity among school children in two urban settings in Kenya. These results can help target childhood obesity prevention measures in Kenya and contribute to the Kenyan national strategy for prevention and control of non-communicable diseases [63].
Declarations
Ethical approval and consent to participate
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by Office of Research Subject Protections at George Mason University (#1385824-3), Maseno University Ethics Review Committee (#MSU/DRP/MUERC/ 00679/19), National Commission for Science, Technology and Innovation (NACOSTI). Parental consent and child assent was obtained prior to commencing research study activities.
Conflict of interest
The authors report no conflict of interest
Author contributions
CAG formulated the study, designed and conducted the research, analyzed the data and wrote the paper. ACO facilitated the field activities, conducted the research and edited the paper. ROO facilitated the field activities, conducted the research and edited the paper. LJC formulated the study and wrote the paper. JG formulated the study and wrote the paper.
Availability of data and materials
The data sets used and analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
This work was supported through an unrestricted gift from the Saff Family to LJC at the Johns Hopkins University. No funding body had any role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors thank all study participants.
References
- Jaacks LM, Vandevijvere S, Pan A, et al. The obesity transition: stages of the global Lancet Diabetes Endocrinol 7 (2019): 231-240.
- Kenya National Bureau of Statistics, Ministry of Health/Kenya, National AIDS Control Council/Kenya, Kenya Medical Research Institute, National Council for Population and Development/Kenya, and ICF International (2015).
- Uganda Bureau of Statistics (UBOS), ICF. Uganda Demographic and Health Survey (2016).
- Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS-MIS) (2016).
- Kyallo F, Makokha A, Mwangi Overweight and obesity among public and private primary school children in Nairobi, Kenya. Health 5 (2013): 85-90.
- Muthuri SK, Wachira L-JM, Onywera VO, et Correlates of objectively measured overweight/obesity and physical activity in Kenyan school children: results from ISCOLE-Kenya. BMC Public Health 14 (2014).
- Brauchla M, Juan W, Story J, et al. Sources of dietary fiber and the association of fiber intake with childhood obesity risk (in 2–18 Year Olds) and diabetes risk of adolescents 12–18 year olds: NHANES 2003–2006. J Nutr Metab 2012 (2012): 1-7.
- Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 346 (2012): e7492-e7492.
- Larson NI, Miller JM, Watts AW, et Adolescent snacking behaviors are associated with dietary intake and weight Status. J Nutr 146 (2016): 1348-1355.
- Grigorakis DA, Georgoulis M, Psarra G, et Prevalence and lifestyle determinants of central obesity in children. Eur J Nutr 55 (2016): 1923-1931.
- Ochola S, Masibo Dietary Intake of Schoolchildren and Adolescents in Developing Countries. Ann Nutr Metab 64 (2014): 24-40.
- Onywera VO, Adamo KB, Sheel AW, et al. Emerging evidence of the physical activity transition in J Phys Act Health 9 (2012): 554-562.
- Cappuccio FP, Taggart FM, Kandala N-B, et Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31 (2008): 619-626.
- Kenya National Bureau of Statistics (KNBS). 2019 Kenya Population and Housing Census. Volume II: Distribution of population and administrative units [Internet]. Kenya National Bureau of Statistics (KNBS) (2019).
- Zuilkowski SS, Piper B, Ong’ele S, et al. Parents, quality, and school choice: why parents in Nairobi choose low-cost private schools over public schools in Kenya’s free primary education Oxford Review of Education 44 (2018): 258-274.
- Gewa CA, Onyango AC, Opiyo RO, et al. Food Environment in and around Primary School Children’s Schools and Neighborhoods in Two Urban Settings in IJERPH 18 (2021): 5136.
- NSW Ministry of NSW Schools physical activity and nutrition survey (SPANS) (2015).
- United States Department of Agriculture (USDA). United States Department of Agriculture (USDA) MyPlate (2020).
- Bull FC, Al-Ansari SS, Biddle S, et World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 54 (2020): 1451-1462.
- Chaput J-P, Dutil C, Sampasa-Kanyinga H. Sleeping hours: what is the ideal number and how does age impact this? Nat Sci Sleep 10 (2018): 421-430.
- Centers for Disease Control and Prevention (CDC). National Health and Nutrition Examination Survey (NHANES) Anthropometry Procedures Manual (2007).
- Mercedes de Onis, Adelheid W Onyango, Elaine Borghi, et Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85 (2007): 660-667.
- Monyeki K, Kemper H, Makgae The association of fat patterning with blood pressure in rural South African children: the Ellisras Longitudinal Growth and Health Study. Int J Epidemiol 35 (2006): 114-120.
- Goulding A, Taylor RW, Grant AM, et al. Waist-to-height ratios in relation to BMI z- scores in three ethnic groups from a representative sample of New Zealand children aged 5–14 Int J Obes 34 (2010): 1188-1190.
- Fredriksen PM, Skår A, Mamen A. Waist circumference in 6–12-year-old children: The Health Oriented Pedagogical Project (HOPP). Scand J Public Health 46 (2018): 12-20.
- Serdula MK, Ivery D, Coates RJ, et al. Do obese children become obese adults? A review of the literature. Prev Med 22 (1993): 167-177.
- Mekonnen T, Tariku A, Abebe Overweight/obesity among school aged children in Bahir Dar City: cross sectional study. Ital J Pediatr 44 (2018): 17.
- Taklual W, Baye S, Mekie M, et al. Double burden of malnutrition among female adolescent students in Bahir Dar City, Amhara, Biomed Res Int 2020 (2020): 1-10.
- Worku M, Gizaw Z, Kassahun Belew A, et Prevalence and associated factors of overweight and obesity among high school adolescents in Bahir Dar City, Northwest, Ethiopia: A cross-sectional study. Ardern CI, editor. J Obes 2021 (2021): 1-8.
- Sedibe M, Pisa P, Feeley A, et al. Dietary habits and eating practices and their association with overweight and obesity in rural and urban Black South African Nutrients 10 (2018): 145.
- Fredriksen PM, Skår A, Mamen A. Waist circumference in 6–12-year-old children: The Health Oriented Pedagogical Project (HOPP). Scand J Public Health 46 (2018): 12-20.
- Motswagole B, Ukegbu P, Kruger H, et al. Waist circumference percentiles of black South African children aged 10 - 14 years from different study sites. S Afr J Clin Nutr 13 (2019): 27-35.
- Darfour-Oduro SA, Buchner DM, Andrade JE, et A comparative study of fruit and vegetable consumption and physical activity among adolescents in 49 Low-and-Middle- Income Countries. Sci Rep 8 (2018): 1623.
- Frank SM, Webster J, McKenzie B, et al. Consumption of fruits and vegetables among individuals 15 years and older in 28 low- and middle-income J Nutr 149 (2019): 1252-1259.
- S. Department of Agriculture, U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020- 2025 (2020).
- Kimani-Murage EW, Muthuri SK, Oti SO, et Evidence of a double burden of malnutrition in urban poor settings in Nairobi, Kenya. Nugent RA, editor. PLOS ONE 10 (2015): e0129943.
- Alinia S, Hels O, Tetens The potential association between fruit intake and body weight - a review. Obes Rev 10 (2009): 639- 647.
- He K, Hu FB, Colditz GA, et al. Changes in intake of fruits and vegetables in relation to risk of obesity and weight gain among middle-aged women. Int J Obes 28 (2004): 1569-1574.
- Buijsse B, Feskens EJ, Schulze MB, et al. Fruit and vegetable intakes and subsequent changes in body weight in European populations: results from the project on Diet, Obesity, and Genes (DiOGenes). Am J Clin Nutr 90 (2009): 202-209.
- Ledoux TA, Hingle, Baranowski Relationship of fruit and vegetable intake with adiposity: a systematic review. Obes Rev 12 (2011): e143-e150.
- Rautiainen S, Wang L, Lee I-M, et Higher intake of fruit, but not vegetables or fiber, at baseline Is associated with lower risk of becoming overweight or obese in middle-aged and older women of normal BMI at baseline. J Nutr 145 (2015): 960-968.
- Yuan S, Yu HJ, Liu MW, et The association of fruit and vegetable consumption with changes in weight and body mass index in Chinese adults: a cohort study. Public Health 157 (2018): 121-126.
- González-Castejón M, Rodriguez-Casado A. Dietary phytochemicals and their potential effects on obesity: A review. Pharmacol Res 64 (2011): 438-455.
- Wang S, Moustaid-Moussa N, Chen L, et al. Novel insights of dietary polyphenols and The Journal of Nutritional Biochemistry 25 (2014): 1-18.
- Wang Y, Beydoun M. Meat consumption is associated with obesity and central obesity among US adults. Int J Obes 33 (2009): 621-
- Romaguera D, Ängquist L, Du H, et Food composition of the diet in relation to changes in waist circumference adjusted for body mass index. Calbet JAL, editor. PLoS ONE 6 (2011): e23384.
- Fretts AM, Howard BV, McKnight B, et al. Associations of processed meat and unprocessed red meat intake with incident diabetes: the Strong Heart Family Am J Clin Nutr 95 (2012): 752-758.
- Rohrmann S, Overvad K, Bueno-de- Mesquita HB, et al. Meat consumption and mortality - results from the European Prospective Investigation into Cancer and Nutrition. BMC Med 11 (2013): 63.
- Fretts AM, Howard BV, Siscovick DS, et al. Processed meat, but not unprocessed red meat, is inversely associated with leukocyte telomere length in the Strong Heart Family J Nutr 146 (2016): 2013-2018.
- Wrottesley SV, Pedro TM, Fall CH, et al. A review of adolescent nutrition in South Africa: transforming adolescent lives through nutrition initiative. S Afr J Clin Nutr 33 (2020): 94-132.
- Kenya Markets Kenya meat end- market trends study (2019).
- Kalimbira A, Gondwe E. Consumption of sweetened beverages among school going children in a densely populated township in Lilongwe, Mal Med J 27 (2015): 55.
- Louwrens H, Venter I, Otty C. Soft drink consumption of Grade 4 and Grade 7 learners in the Wynberg area, City of Cape Town, South Africa and the factors influencing the J Fam Ecol Consum Sci 38 (2010).
- Kondaki K, Grammatikaki E, Jiménez- Pavón D, et Daily sugar-sweetened beverage consumption and insulin resistance in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutr 16 (2013): 479-486.
- Bucher Della Torre S, Keller A, Laure Depeyre J, et Sugar-Sweetened Beverages and obesity risk in children and adolescents: a systematic analysis on how methodological quality may influence conclusions. J Acad Nutr Diet 116 (2016): 638-659.
- Guallar-Castillón P, Rodríguez-Artalejo F, Fornés NS, et al. Intake of fried foods is associated with obesity in the cohort of Spanish adults from the European Prospective Investigation into Cancer and Am J Clin Nutr 86 (2007): 198- 205.
- Gadiraju T, Patel Y, Gaziano J, et al. Fried food consumption and cardiovascular health: a review of current Nutrients 7 (2015): 8424-8430.
- Trumbo PR, Rivers CR. Systematic review of the evidence for an association between sugar-sweetened beverage consumption and risk of obesity. Nutr Rev 72 (2014): 566-
- Costa CS, Del-Ponte B, Assunção MCF, et Consumption of ultra-processed foods and body fat during childhood and adolescence: a systematic review. Public Health Nutr 21 (2018): 148-159.
- Mwangi AM, den Hartog AP, Mwadime RKN, et al. Do street food vendors sell a sufficient variety of foods for a healthful diet? The case of Nairobi. Food Nutr Bull 23 (2002): 48-56.
- Nugent R. Bringing agriculture to the table. How agriculture and food can play a role in preventing chronic disease (2011).
- Tluway FD, Leyna GH, Mmbaga Magnitude and factors associated with overweight and obesity among adolescents in in semi-rural area of Babati District, Tanzania. Tanzania J Hlth Res (2018).
- Ministry of Health. Kenya national strategy for the prevention and control of non- communicable diseases 2015-2020 (2015).