Assessment of Valvular Dysfunction and Aortopathy Involvement in Patients with Bicuspid Aortic Valve: Echocardiographic Study
Article Information
Saousan SERBOUT*, Anass MAAROUFI, Hatim ZAHIDI and Rachida Habbal
Department of Cardiology, Ibn Rochd University Hospital, Casablanca, Morocco
*Corresponding author: Saousan SERBOUT, Department of Cardiology, Ibn Rochd University Hospital, Casablanca, Morocco
Received: 01 March 2020; Accepted: 16 March 2020; Published: 20 March 2020
Citation: Saousan SERBOUT, Anass MAAROUFI, Hatim ZAHIDI and Rachida Habbal. Assessment of Valvular Dysfunction and Aortopathy Involvement in Patients with Bicuspid Aortic Valve : Echocardiographic Study. Cardiology and Cardiovascular Medicine 4 (2020): 087-096.
View / Download Pdf Share at FacebookAbstract
Bicuspid aortic valve is relatively common congenital cardiac anomaly, it is found in approximately 0,5-2% of the general population, which 75% of them are male. Was first described by vinci leonard and is defined by the presence of two abnormal leaflets, usually unequal in size, and not three aortic normal leaflets (as in the normal tricuspid valve). A prospective single center study had been performed in the department of Cardiology,Ibn rushd university hospital, to assess the evolution of valvular and aortic diameter in adults patients with bicuspid aortic valve. A total of 106 patients with bicuspid aortic valve were included during a follow up of 10 years. Aortic dimensions and other echocardiographic parameters were obtained from the echocardiography database of department. Patients with bicuspid aortic valve were mainly male (76,4%), with a mean age of 49 +/- 15 years and a significant proportion of hypertensive patients (50.9%). We notice a majoration of the number of patients with aortic stenosis over time (p < 0,001), with an involvement of transthoracic echocardiography parameters of aortic stenosis, a decrease of the aortic valve area, indexed or not, an increase of peak velocity and mean gradien, this progression was significantly higher (p = 0.0025) in subjects with aortic stenosis at inclusion:16cm/s/year against 4.6cm/s/y and an mean gradient of 3.5mmHg/year against 0.6mmHg/y. Whereas the progression of dilatation of sinus of Valsalva and tubular ascending aorta,was also more important in patients with aortic stenosis at inclusion compared with those who had not, aortic diameters between the 1st and the last control, sinus of valsalva: 0,17- 0,3 mm/year, tubular ascending aorta : 0,32 - 0,6 mm/year. A significant progression of aortic dimeter was obreserved in patients with a small aorta at inclusion compared of others. This study reinforces the fact that clinical and echographic surveillance of these patients, even i
Keywords
Bicuspid aortic valve; Transthoracic echocardiography; Valvular dysfunction; Aorthopathy
Bicuspid aortic valve articles, Transthoracic echocardiography articles, Valvular dysfunction articles, Aorthopathy articles
Article Details
Introduction
Bicuspid aortic valve disease (BAV) is now known to be the most common congenital lesion affecting the human heart, with an estimated prevalence of 0,5% to 2% in the general population [1]. Which 75% of them are male (Dargis et al., 2016;Longobardo et al., 2016) [2,3].
It is suggested that the BAV lesion can cause morbidity and mortality more than any other congenital heart disease [4]. It requires serious follow-up; Most patients with a bicuspid aortic valve will develop some complications during life such as aortic stenosis, aortic regurgitation and aortic dissection [4]. The majority of subjects with bicuspid AV will resort to heart surgery at during their life, mainly for an aortic valve disease, more rarely for a pathology of the ascending aorta, aortic dilatation secondary to a BAV is called bicuspid aorthopathy [5]. The disease represents a heterogeneous spectrum, leading to difficulties in the interpretation of follow-up and treatment options [6]. Transthoracic echocardiography (TTE) is the first-line imaging modality used for the diagnosis and monitoring of patients with BAV. It provides data regarding concomitant aorthopaty and valvular dysfunction.
The aim of this work was to study the progression of the disease (valvular and aortic) in a patients with a BAV followed for a prolonged period of observation.
Methods
Between January 2009 and January 2019, 106 consecutive patients suspected or with a previous diagnosis of BAV were included. All patients were in sinus rhythm. The data collected will be extracted from the medical file.
They were excluded all the patients with a history of aortic or valvular surgery, patients with others pathology causing aorthopathy, antecedents of infectious endcarditis, valvulpathy of other etiology in particular rheumatic, a TTE quality inadequate for diagnosing a BAV (severe calcification of the aortic valve).Patients who refused to participate in the study or who were lost to follow-up were also excluded.
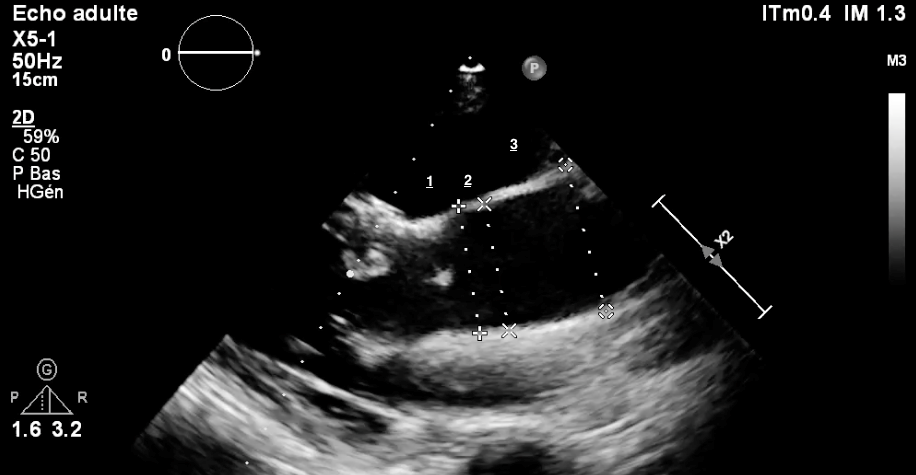
All patients received at least one 1 ETT during follow-up. Echocardiographic studies were carried out using equipment (Philips). The quantification of size and diameter of the heart chambers was determined according to the recommendations of guidelines of the American Society of Echocardiography [7]. The study of the aorta concerned: (1) the aortic valve annulus, (2) the maximal diameter of the sinuses of Valsalva, (3) the sinotubular junction, and averaged at each aortic level, and the results were indexed for body surface area (BSA) (Figure 1).
LV systolic function was assessed with the calculation of the LV ejection fraction using the Simpson biplane method [7].
The degree of aortic stenosis (AS) was graded using Doppler echocardiography (five-chamber view, right parasternal). The primary haemodynamic parameters used for clinical evaluation of AS severity was, AS jet velocity, Mean transaortic gradient, Valve area by continuity equation, velocity ratio, Planimetry of anatomic valve area if is possible andacceleration time/ejection time ratio. Severity of AS was graded as mild in patients with a maximum aortic peak velocity (Vmax) of 2.6 to 2,9 m/second, moderate in those with a Vmax of 3 to 4m/second and severe in those with a Vmax of ≥4 m/ second to evaluate statistical differences, similar to a previous report [7].
Degree of aortic regurgitation (AR) was defined by a composite evaluation of venae contracta, PISA method, Pressure half-time and Diastolic flow reversal in the descending aorta according to guidelines [8].
The ascending aorta is dilated if its diameter exceeding 39 mm [9] and a sinus of Valsalva with a diameter greater than 40 mm is estimated to be dilated [10]. the measurements were indexed to small body size, and diameter was determinatd to be 22 mm / m² and 19 mm / m² for sinus of valsalva and for the ascending aorta respectively.
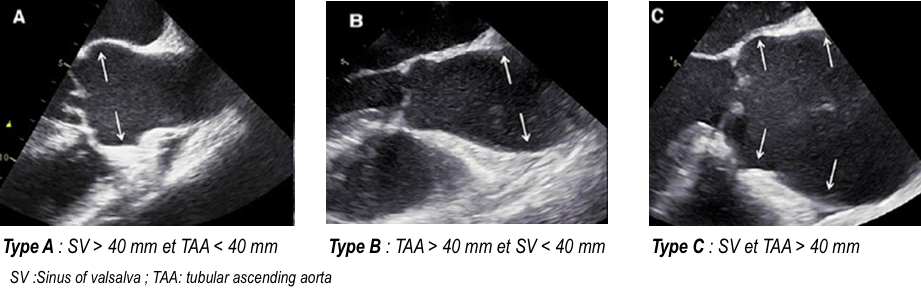
Three different patterns of bicuspid aortic valve aortopathy were difined by Park, [11] based on the tract(s) involved in the dilatation: enlargement of only the Tubular portion of the ascending aorta, enlargement of both the tubular portion and root, and enlargement of only sinus of valsalva (Figure 2).
All analyses were performed using SPSS for Mac, Version 21.0 (SPSS Inc., Chicago, IL, USA).
Figure 2: Park’s classification of aorthopathy: The classification of aortopathy: dilatation of the aortic root (including sinus of Valsalva or sinotubular junction) (A), isolated dilatation of the ascending aorta (B), and diffuse dilatation of the aortic root and ascending aorta (C). The arrows indicate the dilated levels.
Results
Patient characteristics
Table 1 displays the baseline characteristics of the study population.
Patients with bicuspid aortic valve were mainly male (76,4%), the median age of the study group was 49 years (range: 34–64 years). It was a significant proportion of hypertensive patients (50.9%).The frequency of hypertension, diabetes mellitus, dyslipidemia and symptoms is presented in Table 1. In total, 35 (33%) patients had mild AS, and 4 (4 %) had moderate-to-severe AR.
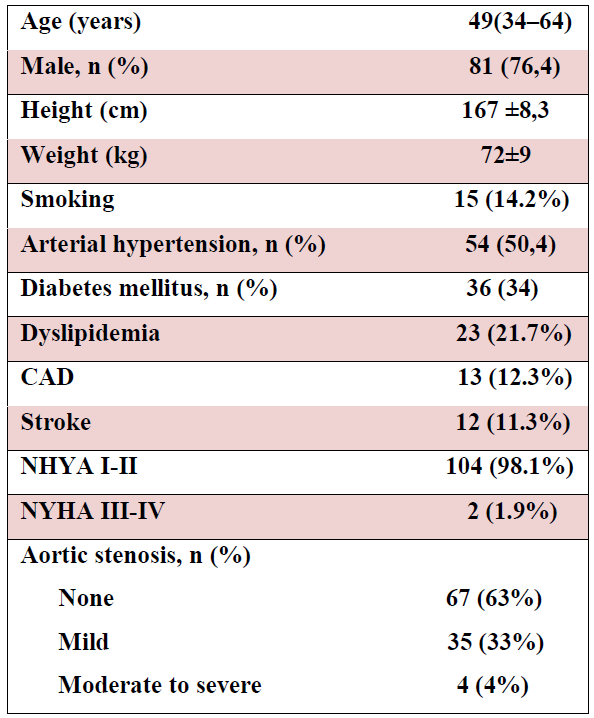
Table 1: Demographic variables and echocardiographic findings in patients with bicuspid aortic valve.
Echocardiography
Aortic diameters at last follow-up echocardiography were 40 ± 0.6 ans 41± 0.6 mm at sinuses and ascending level, respectively (Table2).
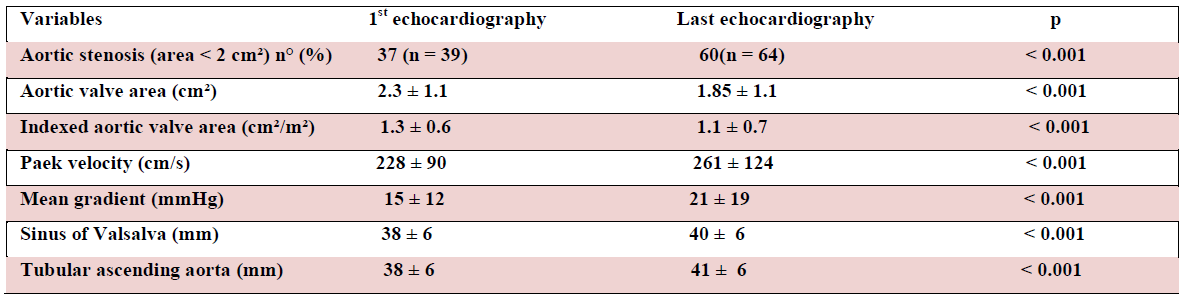
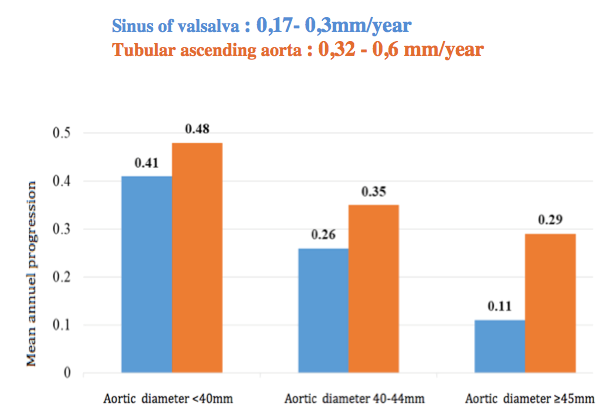
Table 2: TTE parametrs progression over time
Whereas the progression of dilatation of sinus of Valsalva and tubular ascending aorta,was also more important in patients with aortic stenosis at inclusion compared with those who had not, aortic diameters between the first and the last control, sinus of valsalva: 0,17- 0,3 mm/year, tubular ascending aorta : 0.32 – 0.6 mm/year. A significant progression of aortic dimeter was obreserved in patients with a small aorta at inclusion compared of others. (Figure 3).
The aortic root diameter increased over time in 41% of patients, and the ascending diameter increased in 55%. In 32% of patients, no growth was observed at any level. Also, we notice a majoration of the number of patients with aortic stenosis over time (p < 0,001), with an involvement of transthoracic echocardiography parameters of aortic stenosis, a decrease of the aortic valve area, indexed or not, an increase of peak velocity and mean gradient (Table 2). This progression was significantly higher in subjects with aortic stenosis at inclusion:16cm/s/year against 4.6cm/s/year and an mean gradient of 3.5mmHg/year against 0.6mmHg/year. (p = 0.0025) (Table 3).
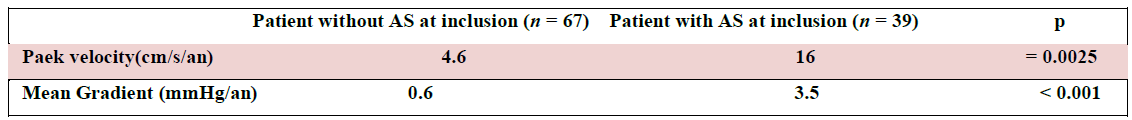
Table 3: Aortic stenosis progression
Complications
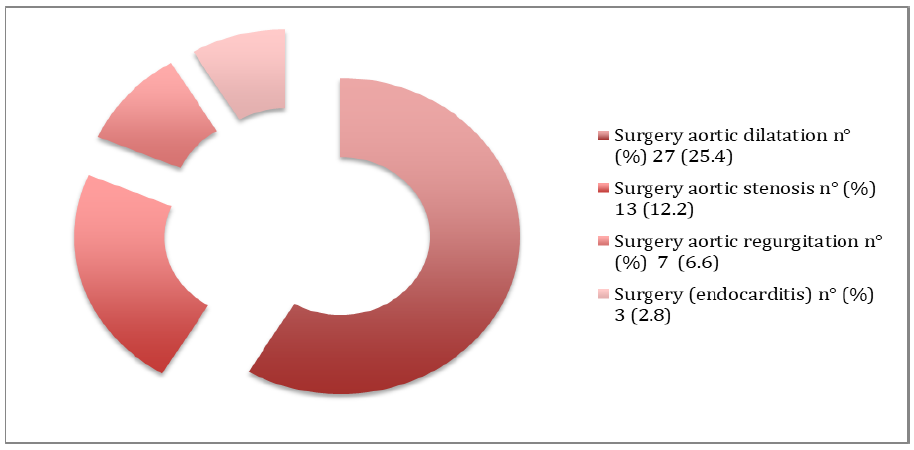
During follow-up of 10 years, 9 patients with BAV developed infectious endocarditis corresponding to a rate of 8.5%. This complication was higher in men than in women (P = 0.037). However, none of the patients underwent aortic dissection or rupture in this series. 48 patients underwent a surgical procedure regardless of whether it was an aortic valve replcement alone or associated with an aortic replacement.All other patients are still under continuous surveillance (Figure 4).
Discussion
Like most studies, this work confirm the male predominance of BAV with a male/ female ratio of 3/1 [12], the GenTAC registry presented at the 2015 American Heart Association Scientific Sessions meeting showed that men had more frequently type 1 BAV with fusion between the left and right coronary cusps than women 81.5% versus 69.0%, P=0.03), whereas type 1 BAV with fusion between the right and noncoronary cusps was more frequently observed in women (18.5% versus 31.0%, P=0.03) [13], but we have non studies that explain sex differences of bicuspid aortic valve morphology and the frequency of male. The exact pathogenesis of the formation of bicuspid aortic valves is not yet fully clair and understood.
Most patients with a bicuspid aortic valve will develop some complication during life, most relaesed studies has been concentreted to evaluate two important complications: aortic dissection and aortic rupture[14,15].Conversely, Few small study sought to identify risk factors for rapid growth of the ascending aorta in patients with bicuspid aortic valve. It is important to note that dissection can also occur at small aortic diameters.
Earlier surgery has been recommended for patients with aortic diameter increase >2 mm/year [16]. In the present series, mean growth rates fell within the range of previously reported values [17,18]. Thus, even this cutoff might be too high. Although typically progressive in its nature (diameters remained stable over time in only 1/3 of patients), Bicuspid aortic valve aortopathy was generally an indolent disease, with slow mean growth rates. Nevertheless, the mean ascending diameter increase in our fast progression group was 0.6 mm/year and 0.3mm respectively in tubular ascending aorta and sinus of valsalva; therefore, our definition successfully identified patients at higher risk of requiring surgery [14].
As other complication, bicuspid aortic valve was involved in mild to severe AS. TTE has been recommended in bicuspid aortic valve patients with symptoms. It could provide precise diagnosis and severity of AS, abnormal hemodynamic, left ventricle function, left stroke volume, and, TTE might be used to decide the surgical intervention time and speculate prognosis [19]. In our series porgression of AS was significant ( p <0.001).
Recently, Michelena, et al. [5] suggested that morbidity (including aortic valve and / or ascending thoracic aorta replacement surgeries, the presence of severe AR and / or AS, thoracic aortic aneurysm but also aortic dissections as well as endocarditis) would be more important in man while mortality would be higher in women (HR = 1.22 (95% CI: [1.02-1.45]; p = 0.026) and HR = 1.44 (95% CI: [1.15-1, 79]; p = 0.001)) in the two cohorts analyzed. In our study there were no deaths.
Several studies have raised the hypothesis of the BAV phenotype and its role in the rapid progression of valve dysfunction and especially in the evolution of arterial diameters [20], however, the results in the literature are still ambiguous.
The contradictory results of the studies as well as the low numbers of patiets studied [20,21] did not allow the creation of a guideline to suggest carrying out a precise valvular phenotyping of the BAV and to organize follow-up intervals specific for different phenotypes, so the use of TEE for this approach was not specifically recommended, except in certain situations [22].
Conclusion
This study reinforces the fact that clinical and echographic surveillance of these patients, even if they are asymptomatic, thus fundamental and necessary to better prevent complications.
What is already know on this topic
Risk of aortic events for aortic aneurysm in BAV.
What this study adds
Echographic surveillance of patients with bicuspid aortic valve is fondamental to prevent complications even with small aortic diameters.
Competing interests
The authors declare no competing interest.
Funding
We have no funding sources to declare
Authors’ contributions
The contributions of authors is as follows:
Design of the study: Serbout,Maaroufi and Zahidi
Aquisition of data: all authors
Analysis and interpretation of data: Serbout, Maaroufi and Habbal
Statical analysis: Serbout, Maaroufi and zahidi
drafting the work or revising it critically for important intellectual content: all authors.
References
- Baumgartner H, Bonhoeffer P, De Groot NM, de Haan F, Deanfield JE, et al.ESC Guidelines for the management of grown-up congenital heart disease.Eur Heart J 31 (2010): 2915-57.
- Dargis N, Lamontagne M, Gaudreault N, Sbarra L, Henry C, Pibarot P, Mathieu P, Bossé Y.Identification of Gender-Specific Genetic Variants in Patients With Bicuspid Aortic Valve.Am J Cardiol 117 (2016): 420-6.
- Longobardo L, Jain R, Carerj S, Zito C, Khandheria BK.Bicuspid Aortic Valve: Unlocking the Morphogenetic Puzzle.Am J Med 129 (2016): 796-805.
- Ward C.Clinical significance of the bicuspid aortic valve.Heart 83 (2000): 81-85.
- Michelena HI, Della Corte A, Prakash SK, Milewicz DM, Evangelista A, Enriquez-Sarano M.Bicuspid aortic valve aortopathy in adults: Incidence, etiology, and clinical significance.Int J Cardiol 201 (2015): 400-7.
- Fedak PW, Barker AJ, Verma S. Year in review: bicuspid aortopathy. Curr Opin Cardiol 31 (2016):132–8.
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, et al.Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging.J Am Soc Echocardiogr 28 (2015): 1-39.e14
- Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, et al.2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.Circulation 129 (2014): 2440-92.
- Della Corte A, Bancone C, Dialetto G, Covino FE, Manduca S, Montibello MV, De Feo M, Buonocore M, Nappi G.The ascending aorta with bicuspid aortic valve: a phenotypic classification with potential prognostic significance.Eur J Cardiothorac Surg 46 (2014): 240-7.
- Kang JW, Song HG, Yang DH, Baek S, Kim DH, et al.Association between bicuspid aortic valve phenotype and patterns of valvular dysfunction and bicuspid aortopathy: comprehensive evaluation using MDCT and echocardiography.JACC Cardiovasc Imaging 6 (2013): 150-61.
- Park CB, Greason KL, Suri RM, Michelena HI, Schaff HV, Sundt TM 3rd.Fate of nonreplaced sinuses of Valsalva in bicuspid aortic valve disease.J Thorac Cardiovasc Surg 142 (2011): 278-84.
- McKellar SH, Michelena HI, Li Z, Schaff HV, Sundt TM 3rd.Long-term risk of aortic events following aortic valve replacement in patients with bicuspid aortic valves.Am J Cardiol 106 (2010): 1626-33.
- Roman MJ, Pugh NL, Devereux RB, Eagle KA, Holmes K, et al.Aortic Dilatation Associated With Bicuspid Aortic Valve: Relation to Sex, Hemodynamics, and Valve Morphology (the National Heart Lung and Blood Institute-Sponsored National Registry of Genetically Triggered Thoracic Aortic Aneurysms and Cardiovascular Conditions).Am J Cardiol 120 (2017): 1171-1175.
- Michelena HI, Khanna AD, Mahoney D, Margaryan E, Topilsky Y, Suri RM, Eidem B, Edwards WD, Sundt TM 3rd, Enriquez-Sarano M.Incidence of aortic complications in patients with bicuspid aortic valves.JAMA 306 (2011): 1104-12.
- Elefteriades JA, Farkas EA.Thoracic aortic aneurysm clinically pertinent controversies and uncertainties.J Am Coll Cardiol 55 (2010): 841-57.
- Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, et al.Guidelines on the management of valvular heart disease.Eur Heart J 33 (2012): 2451-96.
- Thanassoulis G, Yip JW, Filion K, Jamorski M, Webb G, Siu SC, Therrien J.Retrospective study to identify predictors of the presence and rapid progression of aortic dilatation in patients with bicuspid aortic valves.Nat Clin Pract Cardiovasc Med 5 (2008): 821-8.
- Etz CD, Zoli S, Brenner R, Roder F, Bischoff M, Bodian CA, DiLuozzo G, Griepp RB.When to operate on the bicuspid valve patient with a modestly dilated ascending aorta.Ann Thorac Surg 90 (2010): 1884-90.
- Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, et al.2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines.Circulation 135 (2017): e1159-e1195.
- Fernandes SM, Khairy P, Sanders SP, Colan SD.Bicuspid aortic valve morphology and interventions in the young.J Am Coll Cardiol 49 (2007): 2211-4.
- Schaefer BM, Lewin MB, Stout KK, Gill E, Prueitt A, Byers PH, Otto CM.The bicuspid aortic valve: an integrated phenotypic classification of leaflet morphology and aortic root shape.Heart 94 (2008): 1634-8.
- Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, et al.2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC).Eur Heart J 35 (2014): 2873-926.