Assessment of Impact of Coronary Artery Calcium On Cardiovascular Risk Stratification in an Indian Cohort
Article Information
Abhishek Gaikwad1*, Yasmin Khan1, Anupam Kumar Singh2
1Metro hospital and cancer research centre, Jabalpur, India
2Santosh medical college,Ghaziabad
*Corresponding author: Abhishek Gaikwad, Metro hospital and cancer research centre, Jabalpur, India
Received: 15 September 2019; Accepted: 19 September 2019; Published: 27 September 2019
Citation: Abhishek Gaikwad, Yasmin Khan, Anupam Kumar Singh. Assessment of Impact of Coronary Artery Calcium On Cardiovascular Risk Stratification in an Indian Cohort. Cardiology and Cardiovascular Medicine 3 (2019): 373-385.
View / Download Pdf Share at FacebookAbstract
Background: Cardiovascular diseases are emerging as a major cause of mortality and disability in India. Coronary artery Calcium (CAC) has been proposed as an additional tool for risk re-stratification for Primary prevention. However, there is a lack of data for its incremental value assessment in Indian patients.
Methods: This study included 150 patients presenting with risk factors for Cardiovascular Diseases or Symptoms. 10-year risk of CVD was calculated using risk assessment models Revised American College of Cardiology/American Heart Association (Risk ACC/AHA) and WHO Risk Prediction Charts. CT Angiography and Coronary Artery Calcium Scoring was done in each patient.
Results: 48.2 % (28/57) of patients in Statins recommended category (10 yr ASCVD Risk >7.5 %) and 11/17 (64.7%) in Statin Considered group (ASCVD Risk 5-7.5 %) according to guidelines had CAC Zero. 13/75 (17.3 %) of patients in whom statin was not recommended had a non-zero Coronary artery Calcium. A total of 52/150 (34.6%) (Statin not needed with CAC non-zero -13, Statin considered and recommended with CAC zero - 39) would be risk restratified using CAC.
Conclusion: One Third Patients would be risk restratified using Coronary Artery Calcium Score as an additional tool to convention Cardiovascular Risk Scores.
Keywords
Coronary Artery; Cardiovascular Risk
Article Details
Introduction
Cardiovascular risk assessment is the keystone of primary prevention of atherosclerotic CV disease (ASCVD) [1,2]. Future risk assessment is typically calculated in 10 year or lifetime basis and helps in tailoring the therapy. Population based risk calculators like pooled cohort risk equation, WHO-ISH Risk score and Framingham Risk Score have been typically used for these calculations. Newer tools like CACS (coronary artery calcium Score), CIMT (Carotid Intima Media thickness) and hsCRP have been proposed for adjuvants for better risk stratification [3-5].
CACS has been shown to be an excellent predictor of CV Risk events [6-11] which considerably helps in risk restratification in these cohorts. Some studies have suggested using ‘power of zero’ [12-16]; using Zero calcium Score to downgrade statin therapy in various primary prevention cohorts. In a recent meta-analysis the event rate in 29,312 individuals was very low (0.47 %) over a period of mean follow up of 50 years and these individuals had a relative risk of 0.15 in comparison to CACS > 0, thereby implying an 85% lower risk for individuals with zero calcium score [17].
Recent AHA update for primary prevention [18] suggests that CACS be now used as a two-way tool for moving individuals both up and down the risk spectrum) for individuals in whom treatment might be considered. A recent study suggests up to half of patients in the intermediate risk group could be taken off statins (as they have CAC of zero) using this approach [17].
However, we could find no Indian studies in literature evaluating the effect of this approach on primary prevention strategy.
Hence this study was undertaken to evaluate the incremental effect of CACS on Risk assessment strategies for primary prevention in our cohort.
Material and Methods
Our Cohort included 150 consecutive patients presenting to Outpatient Department of a tertiary Hospital between February 2018 to Jan 2019.
The patients with known Atherosclerotic Cardiovascular disease (MI,Stroke, Peripheral Arterial Disease were excluded from Study).
History and clinical examination were done in each patent especially with respect to the presence of significant CVD risk factors. Physical examination consisted of General Physical examination and examination of Cardiovascular (CV) system. Height and body weight were measured and body mass index (BMI) was calculated. Smoking, diabetes and hypertension were defined according to the National Health Interview Survey (NHIS).
Biochemical parameters Fasting and Random blood sugar, Lipid profile was performed in every patient. Systolic and diastolic Blood pressure was recorded in each patient.
Risk Score calculation
Two risk calculators (WHO ISH RISK and Risk ACC/AHA) were used to calculate 10-year risk of having a major CV event (CV death, MI or stroke) for every patent. InRisk ACC/AHA calculator, the race was taken into account as an additional factor.
Calculators were available on the following websites (https://www.framingham heartstudy.org/risk-functions/cardiovascular-disease/10-yearrisk.php#, https://sanjaybasu.shinyapps.io/ascvd/). whoshRsk R package. Was used to calculated WHO-ISH RISK. Using different risk calculators, 10-year CVD risks were divided into the five sub- categories -low risk (<10%,10-20%) and high risk (20-30%,30-40%,>=40%) groups in each model to identify which model maximally identifies the high-risk groups.
Coronary Artery Calcium Scoring
All patients underwent 64 slice Coronary CT Angiogram including the asymptomatic subjects with risk factors. The images were obtained with ECG-gating. Each slice has a 3mm thickness,tube voltage of 120 kVs with a radiation dose less than 2 mSv. All studies were interpreted by radiologists and cardiologists with speciality in Cardiovascular imaging.
Patients were classified as (a) normal (no calcific or soft plaque), (b) thick plaque and moderate CAD (<50% stenosis), (c) obstructive coronary disease (>50% stenosis).Coronary artery calcium report was simultaneously noted in all patients
Statistical analysis
Statistical analysis was carried out by using R version 3.5.0. Values are expressed as mean± standard deviation or as percentages. A p-value <0.05 was considered statistically significant
Results
Our Cohort had 150 patients baseline Variables were as follows: Middle aged Population (Mean = 51.77, SD = 10.28, IQR [27.00, 76.00]), SBP (Mean = 132.15, SD = 14.68 IQR[96.00, 180.00]), DBP (Mean = 89.43, SD = 9.70, [67.00, 124.00])
Around ? population was male, 42% Diabetics,28% Smokers. 24.6% had a family history of CAD. CT Angiography was abnormal in 12% patients. Further Details are shared in Table 1.
|
Variable |
levels |
|
|
Age |
Mean (SD) |
51.8 (10.3) |
|
Alcohol |
NO |
110 (73.3) |
|
YES |
40 (26.7) |
|
|
current_smoker |
NO |
108 (72.0) |
|
YES |
42 (28.0) |
|
|
SBP |
Mean (SD) |
132.1 (14.7) |
|
DBP |
Mean (SD) |
89.4 (9.7) |
|
Family_History |
NO |
113 (75.3) |
|
YES |
37 (24.7) |
|
|
HDL |
Mean (SD) |
43.0 (10.4) |
|
LDL |
Mean (SD) |
130.5 (34.0) |
|
TG |
Mean (SD) |
164.1 (30.2) |
|
Total_Cholesterol |
Mean (SD) |
206.4 (35.7) |
|
Sex |
FEMALE |
59 (39.3) |
|
MALE |
91 (60.7) |
|
|
Diabetes |
0 |
87 (58.0) |
|
1 |
63 (42.0) |
|
|
Framingham Risk Score |
Mean (SD) |
18.3 (14.7) |
|
Smoking |
0 |
108 (72.0) |
|
1 |
42 (28.0) |
|
|
ASCVD Risk Score |
Mean (SD) |
8.8 (10.2) |
|
ASCVD_Category |
< 5 % |
75 (50.0) |
|
5 - <7.5 % |
17 (11.3) |
|
|
7.5 - <20% |
40 (26.7) |
|
|
> 20% |
18 (12.0) |
|
|
CAC Category |
0 |
101 (67.3) |
|
1-100 |
30 (20.0) |
|
|
>100 |
19 (12.7) |
|
|
CAC_Zero |
0 |
101 (67.3) |
|
>0 |
49 (32.7) |
|
|
symptoms |
Atypical Chest Pain |
81 (54.0) |
|
Dyspnea |
16 (10.7) |
|
|
Palpitation |
10 (6.7) |
|
|
Typical Chest Pain |
43 (28.7) |
|
|
CT_Angiography |
Abnormal |
18 (12.0) |
|
Normal |
132 (88.0) |
|
|
Vessels_involved |
Double |
12 (8.0) |
|
None |
132 (88.0) |
|
|
Single |
5 (3.3) |
|
|
Triple |
1 (0.7) |
|
|
ASCVD_AHA |
Statin Not Needed |
75 (50.0) |
|
Statin Considered |
17 (11.3) |
|
|
statin Recommended |
58 (38.7) |
|
|
WHO_ISH Risk |
<10% |
116 (77.3 %) |
|
10 - <20% |
14(9.3 %) |
|
|
20 - <30% |
12(8 %) |
|
|
30 - <40% |
4(2.6 %) |
|
|
> 40% |
4(2.6 %) |
Table 1: Baseline Demographic characteristic
Association between CAC and ASCVD Score
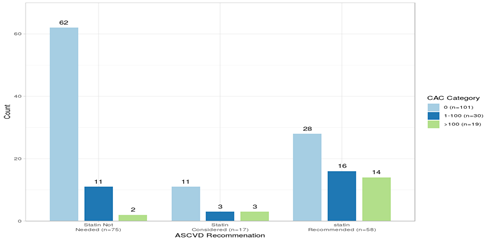
The Dodged bar chart represents individual counts representing frequency of CAC_Cat categories 1-100,0 and >100 in ASCVD categories Statin Not Needed(ASCVD < 5 %), Statin Considered (5- 7.5 %) and statin Recommended (>7.5 %).
CAC 0 has the highest percentage in all three groups, however with decreasing trend: 62/75 (82.67 %) in group Statin Not Needed. 11/17 (64.71 %) in group Statin Considered and 28/58 (48.28 %) in group statin Recommended.
Thus we see that even in Statin recommended group, Half patients have CAC Zero.
To formally check for association between groups we performed pearson chi-square test. We found a Significant association between CAC category and ASCVD category. The chi-square statistic was 20.83. The degree of freedom was 4 and P value was <0.001.Contingency and Proportion table are shown below (Table 2 and Table 3)
|
AHA Recommendation |
CAC Category |
n |
percentage |
95 % Confidence Interval |
|
Statin Not Needed |
0 |
62 |
62/75 ( 82.67 %) |
72.95% - 89.92% |
|
Statin Not Needed |
1-100 |
11 |
11/75 ( 14.67 %) |
8.05% - 23.95% |
|
Statin Not Needed |
>100 |
2 |
2/75 ( 2.67 %) |
0.56% - 8.28% |
|
Statin Considered |
0 |
11 |
11/17 ( 64.71 %) |
41.14% - 83.71% |
|
Statin Considered |
1-100 |
3 |
3/17 ( 17.65 %) |
5.23% - 40.01% |
|
Statin Considered |
>100 |
3 |
3/17 ( 17.65 %) |
5.23% - 40.01% |
|
statin Recommended |
0 |
28 |
28/58 ( 48.28 %) |
35.76% - 60.96% |
|
statin Recommended |
1-100 |
16 |
16/58 ( 27.59 %) |
17.37% - 39.97% |
|
statin Recommended |
>100 |
14 |
14/58 ( 24.14 %) |
14.56% - 36.22% |
Table 2: Contingency Table of Statin Recommendation and CAC risk stratification
Risk Restratification
Using New AHA guideline recommendation a total of 52/150 (Statin not needed with CAC non-zero -13, Statin considered and recommended with CAC zero - 39) would be risk re-stratified. Around (13/75) 17.3 % patients in statin not-needed group might be recommended statins, while 39/75 (52%) patients in statin considered or recommended group,would be considered for risk downgrade.
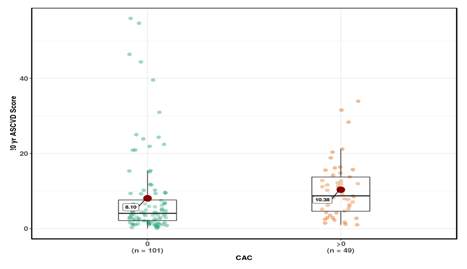
ASCVD Risk Score in CAC Categories
The mean in Group CAC =0 [8.1 ± 11.20] was significantly lower than Group CAC >0 [10.38 ± 7.54]. The mean difference was -2.28 and 95 % confidence interval of the difference was (-5.34 - -0.79). The p value was 0.04. The t statistic was -2.1 and degree of freedom of the Welch unpaired two-sample t test was 132.7.In Formal statistical notation this result is expressed as : t(132.7) = -2.1, p= 0.04.
Association of CAC with WHO ISH Risk Category
There was a Non-significant association between CAC category. andwho_risk. The chi-square statistic was 10.04 . The degree of freedom was 6 and P value was 0.12. The distribution is described in Table below.
|
who_risk |
CAC_Cat |
n |
value |
95 % Confidence Interval |
|
<10% |
0 |
82 |
82/116 ( 70.69 %) |
61.97% - 78.39% |
|
<10% |
1-100 |
20 |
20/116 ( 17.24 %) |
11.21% - 24.88% |
|
<10% |
>100 |
14 |
14/116 ( 12.07 %) |
7.09% - 18.91% |
|
10% to <20% |
0 |
7 |
7/14 ( 50 %) |
25.89% - 74.11% |
|
10% to <20% |
1-100 |
6 |
6/14 ( 42.86 %) |
20.29% - 68.06% |
|
10% to <20% |
>100 |
1 |
1/14 ( 7.14 %) |
0.78% - 28.84% |
|
20% to <30% |
0 |
7 |
7/12 ( 58.33 %) |
31.19% - 81.95% |
|
20% to <30% |
1-100 |
2 |
2/12 ( 16.67 %) |
3.63% - 43.62% |
|
20% to <30% |
>100 |
3 |
3/12 ( 25 %) |
7.59% - 52.92% |
|
30% to <40% |
0 |
1 |
1/4 ( 25 %) |
2.85% - 71.62% |
|
30% to <40% |
1-100 |
2 |
2/4 ( 50 %) |
12.28% - 87.72% |
|
30% to <40% |
>100 |
1 |
1/4 ( 25 %) |
2.85% - 71.62% |
Table 3: Contingency Table of 10 yr WHO predicted Risk Score and CAC risk stratification
Association between CAC Zero and Risk Factors
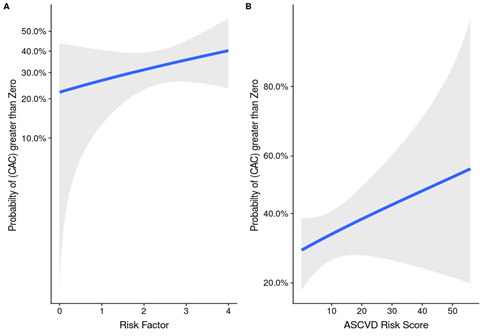
We can see in Figure 3, Probability of CAC > Zero rises when number of Risk factors increase.
|
Risk Factors |
CAC_Zero |
n |
|
0 |
0 |
1 |
|
0 |
>0 |
1 |
|
1 |
0 |
16 |
|
1 |
>0 |
5 |
|
2 |
0 |
47 |
|
2 |
>0 |
18 |
|
3 |
0 |
28 |
|
3 |
>0 |
22 |
|
4 |
0 |
9 |
|
4 |
>0 |
3 |
Table 4: Association of risk factors and CAC score
Discussion
We found that 48.2 % of Our patients in whom Statins was recommended (10 yr ASCVD Risk >7.5 %) as per ACC/AHA guidelines had Coronary Artery Calcium of zero. Around ?rd of the patients in which Statins were Considered (ASCVD Risk 5-5.5 %) according to guidelines had CAC Zero. Around one fifth of patients in whom statin was not recommended had a non-zero Coronary artery Calcium. Since previous studies in MESA Cohort have shown that people with CAC Zero have very low event rate (1.3% to 5.6 %) [17], our findings can be used to down-grade individual statin recommendation for intermediate (AHA 7.5 %-20%) and downgrade intensity of Statins for very high risk individuals (>20%). To our knowledge, this is the first Indian Study to explore potential reclassification of new heterogenous AHA/ASCVD Risk Profile with CAC Score.
Our Findings are similar to study by Nasir et al [17], where almost half of the patients who were recommended Statins had CAC of Zero. If we combine statin considered and recommended groups, then percentage of people with CAC zero was 52 % which is slightly higher than f44% seen in study by Nasir et al.
In our study, Around one third patients [34.6 %] would be risk re-stratified using CAC Scoring.
Other studies also report reclassification in range of 30-50%. A recent meta-analysis of 4 prospective cohort studies by Grandhi et al, demonstrated >50% lower ASCVD risk in statin eligible subjects with CAC = 0 compared to those with CAC > 0. These results support emerging consensus that CAC = 0 reclassifies risk of statin candidates below the threshold of statin recommendation (i.e. <5%), allowing flexibility in management decisions [19]. In a study by Alashi et al almost 41 % patients were reclassified on comparing MESA -CAC with ASCVD Risk Scores [20].
The ability of CAC to downgrade risk profile in almost half of the patients as observed in our study and other cohorts can be of considerable importance, given the new AHA guidelines and help in keeping them off statins and can be cost-effective as well as shown in some studies.
There are many strengths of our study: determination of quantum of risk re-stratification in an Indian population in a new cohort, use of new modified Pooled cohort equation not used in other studies and assessment of WHO-ISH risk scores as well.
There are some limitations of our study; ‘Derisking‘ with CAC is still not recommended guidelines in diabetics, smokers and individuals with a history of premature cardiovascular disease[21], though strategy is not supported by randomized clinical trial, though trials in this area have been proposed, and there is risk of exposing patients to radiation (current exposure from a CAC scan (0.89 mSv)), though this is almost one third of annual background radiation exposure.
Conclusion
Our study shows that almost one third of the population will be re-stratified regarding their lifetime use if CAC Scoring is used in addition to 10 yr ASCVD Score for use of statins as mode of primary prevention in Indian Population.
References
- Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation 97 (1998): 1837–1847.
- D’AgostinoSr RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: [24_TD$ IF] the Framingham heart study. Circulation 117 (2008): 743–753.
- Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation 92 (1995): 2157–2162.
- Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation 74 (1986): 1399–1406.
- Persson J, Formgren J, Israelsson B, Berglund G. Ultrasound-determined intima-media thickness and atherosclerosis. Direct and indirect validation. Arterioscler Thromb 14 (1994): 261–264.
- Budoff MJ, Young R, Burke G, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ascvd) events: the multi-ethnic study of atherosclerosis (mesa). Eur Heart J 39 (2018): 2401–2408.
- Erbel R, Mohlenkamp S, Moebus S, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf recall study. J Am CollCardiol 56 (2010): 1397–1406.
- Vliegenthart R, Oudkerk M, Hofman A, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation 112 (2005): 572–577.
- Ferencik M, Pencina KM, Liu T, et al. Coronary artery calcium distribution is an independent predictor of incident major coronary heart disease events: [results from the Framingham heart study. Circ Cardiovasc Imaging 2017: 10.
- Carr JJ, Jacobs Jr DRJr, Terry JG, et al. Association of coronary artery calcium in adults aged 32–46 years with incident coronary heart disease and death. JAMA Cardiol 2 (2017): 391–399.
- Manson JE, Allison MA, Carr JJ, et al. Calcium/vitamin d supplementation and coronary artery calcification in the women’s health initiative. Menopause 17 (2010): 683–691.
- Blaha MJ, Cainzos-Achirica M, Greenland P, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: [47_TD$ IF] the multi-ethnic study of atherosclerosis (mesa). Circulation 133 (2016): 849–858.
- Sarwar A, Shaw LJ, Shapiro MD, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2 (2009): 675–688.
- Nasir K, Rubin J, Blaha MJ, et al. Interplay of coronary artery calcification and traditional risk factors for the prediction of all-cause mortality in asymptomatic individuals. Circ Cardiovasc Imaging 5 (2012): 467–473.
- Valenti V, Ó Hartaigh B, Heo R, et al. A 15-year warranty period for asymptomatic individuals without coronary artery calcium: a prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging 8 (2015): 900–909.
- Blaha MJ, Blumenthal RS, Budoff MJ, Nasir K. Understanding the utility of zero coronary calcium as a prognostic test: a bayesian approach. Circ CardiovascQual Outcomes 4 (2011): 2153–256.
- Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American college of cardiology/ American heart association cholesterol management guidelines: Mesa (multi-ethnic study of atherosclerosis). J Am CollCardiol 66 (2015): 1657–1668.
- Grundy SM et al. AHA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. JACC 73 (2019): e285-350.
- Grandhi G et al . Risk reclassification with absence of coronary artery calcium among statin candidates according to american college of cardiology/american heart association (acc/aha) guidelines: systematic review and meta-analysis. Journal of the American College of Cardiology 71 (2018): A1675.
- Alashi A, Lang R, Seballos R, Feinleib S, Sukol R, Cho L, Schoenhagen P, Griffin BP, Flamm SD, Desai MY. Reclassification of coronary heart disease risk in a primary prevention setting: traditional risk factor assessment vs. coronary artery calcium scoring. Cardiovascular Diagnosis and Therapy 9 (2019): 214-220.
- Bittencourt MS, Blaha MJ, Nasir K. Coronary artery calcium-from screening to a personalized shared decision-making tool: the new American prevention guidelines. Arquivosbrasileiros de cardiologia 112 (2019): 1-2.