Assessment of C-reactive Protein, Lipid Profile and Body Mass Index in Type2 Diabetes Mellitus in Sudanese Patients
Article Information
Alhussein Alsayed Mukhtar Garrashy1*, Omer Fudal Idris2, Mustafa Salimeen3, Ibrahim Eltirafi4
1Department of Biochemistry, College of veterinary medicine, University of Bahri, Khartoum, Sudan
2Department of Biochemistry, Faculty of science and technology, Al-Neelain University, Khartoum, Sudan
3Department of Radiology, Dongola teaching hospital, University of Dongola, Dongola, Sudan
4Department of internal medicine, Asia Hospital, Omdurman city, Sudan
*Corresponding author: Alhussein Alsayed Mukhtar Garrashy, Department of biochemistry, College of veterinary medicine, University of Bahri, Khartoum, Sudan
Received: 01 May 2021; Accepted: 11 May 2021; Published: 22 May 2021
Citation:
Alhussein Alsayed Mukhtar Garrashy, Omer Fudal Idris, Mustafa Salimeen, Ibrahim Eltirafi. Assessment of C-reactive Protein, Lipid Profile and Body Mass Index in Type2 Diabetes Mellitus in Sudanese Patients. Archives of Internal Medicine Research 4 (2021): 125-133.
View / Download Pdf Share at FacebookAbstract
Background and aim: Diabetes mellitus (DM) is a disease characterized by chronic hyperglycemia caused by a lack of insulin or resistance, resulting in metabolism dysregulation, which accounts for the symptoms and complications of diabetes. The present study aimed to assess some biochemical markers such as C-reactive protein (CRP), lipid profile, and body mass index (BMI) in type 2 diabetes mellitus (T2DM) in Sudanese patients.
Patients and methods: The study included 104 patients with type two diabetes mellitus (56 men and 48 women, 40 to 70 years old) and 104 non-diabetic healthy volunteers (56 men, 48 women, 40 to 70 years old). Anthropometric measurements were assessed, and blood samples were collected for analysis of lipid profile and C-reactive protein (CRP).
Result: The result showed a significant increase in CRP, BMI, total cholesterol (TC), triglycerides (TGs), non-HDL-C, and LDL-C in the diabetic patients when compared with the healthy control group (P-value 0.000). The study also showed a significant increase in BMI, CRP, TC, non-HDL-C, TGs, and LDL-C in female patients in comparison with male patients with (P-value 0.014, 0.037, 0.003, 0.026, 0.046, and 0.014 respectively). Moreover, the study showed that CRP had a positive correlation with TC, non-HDL-C, TGs, LDL-C, and BMI, with (P-value 0.001, 0.000, 0.000, 0.008, and 0.000 respectively).
Conclusion: The study finally concludes the coexistence of dyslipidemia, overweight, obesity, and inflammation in diabetes, in general, and with more frequent in female diabetes when compared with their male counterparts.
Keywords
Type 2 Diabetes Mellitus, Lipid Profile, C-Reactive Protein, Body Mass Index
Article Details
1. Introduction
Diabetes mellitus (DM) is a condition characterized by chronic hyperglycemia caused by a lack of or insulin resistance, resulting in dysregulation of carbohydrate, protein, and lipid metabolism, which accounts for the symptoms and complications of diabetes. Diabetes is expected to be the seventh leading cause of death by 2030, according to the World Health Organization [1]. According to recent estimates, diabetes affects 1.4 million people in Sudan, with a prevalence of 7.7% and more than 25,000 diabetes-related deaths [2]. However, Type 2 diabetes mellitus (T2DM) is accounted for about 90% of all diabetes cases worldwide. There is a well-established correlation between diabetes and systemic inflammation, which may be reflected in circulating c-reactive protein (CRP) levels [3]. Hepatocytes synthesize and release C- reactive protein, which is regulated by cytokines such as IL-6, IL-1, and TNF-, which are formed by adipocytes CRP, a responsive physiological marker of subclinical systemic inflammation, has been linked to hyperglycemia, insulin resistance, and overt T2DM in studies [4]. Furthermore, increased CRP levels have been identified in adult T2DM patients [5]. A recent study discovered a connection between CRP and the onset of T2DM. Obesity and hypertension were found to interact with each other in the older population ( > 50 years ) [6].
Previous research has attempted to link blood glucose levels to lipid abnormalities in the serum [7]. Lipid abnormalities are common in diabetes mellitus since insulin deficiency or resistance affects key enzymes and pathways in lipid metabolism. Furthermore, study findings indicate that the rise in the prevalence of T2DM among the body composition components is primarily due to body fats [8]. According to a recent study [9], hypercholesterolemia, hypertriglyceridemia, elevated LDL-C, and reduced HDL-C are all symptoms of dyslipidemia caused by diabetes. These results suggest that hyperlipidemia predominates over the higher prevalence of diabetic dyslipidemia. Furthermore, a recent cross-sectional study [10] found a high prevalence of obesity among diabetics, along with elevated levels of triglycerides, LDL-C, and CRP, implying that dyslipidemia and inflammation are coexisting in diabetes. Diabetics were 5.6 times more likely than non-diabetics to have elevated CRP levels, according to their results. They discovered that CRP levels had an important positive relationship with LDL-C and BMI (BMI). However, the relationship between certain biochemical markers and CRP in those patients is unclear. This study aimed to see whether there is a correlation between these biochemical markers, such as lipid profile, BMI, and C-reactive protein, and T2DM in Sudanese patients.
2. Materials and Methods
2.1 Study population
One hundred four patients with type two diabetes mellitus (56 men and 48 women, 40 to 70 years old) were randomly selected. The patients have no history of coronary heart disease, liver dysfunction, renal dysfunction, cardiac valvular disease, heart failure, tumor, immune diseases. A total number of 104, healthy individuals (56 men, 48 women, 40 to 70 years old) were recruited to represent the control group, with no history of diabetes mellitus or other diseases.
2.2 Study design
This study is an analytical case-control hospital-based study.
2.3 Ethical consideration
Permission to carry out this research was obtained from health authorities, and blood sample collection was carried out under the full supervision of medical doctors. All subjects included in this study were fully informed about the aim of this study.
2.4 Reagents and devices
Reagents and devices used in this study included: total cholesterol kits, high-density lipoprotein cholesterol kits, low-density lipoprotein kits, Triglycerides kits. COBAS INTEGRA: Cat. No. 20764930 322, C-Reactive Protein (Latex): System-ID 07 6493 0. A calibrated spectrophotometer (Awareness Technology, model No. 1904 plus, serial No 1904-5252), COBAS INTEGRA 700 analyzer, and a properly calibrated high-quality electronic digital scale.
2.5 Biochemical measurements
Biochemical measurements were carried out using standard methods according to the procedures recommended by the manufacturer. CRP was measured turbid-metrically. Serum total cholesterol, HDL-C, LDL-C, and triglycerides were determined by spectrophotometry using standard enzymatic methods. Non-HDL-C, obtained by subtracting HDL-C from the
total cholesterol.
2.6 Measurement of body weight, height, and calculating BMI
A proper calibrated of the high-quality electronic digital scale was used for measurement of both body weight (Kg) and height (cm). After collecting an individual's height and weight, the BMI was calculated as follow: B MI = Weight (Kg)/(Height in meters)2.
2.7 Statistical methods
Statistical package for social science (SPSS), was used for data analysis. The data were expressed as means ± standard deviation. The one-way analysis of variance (ANOVA) was used to compare all parameters for the patient and control groups, and multiple comparisons were used to find the significance between the two groups.
3. Results
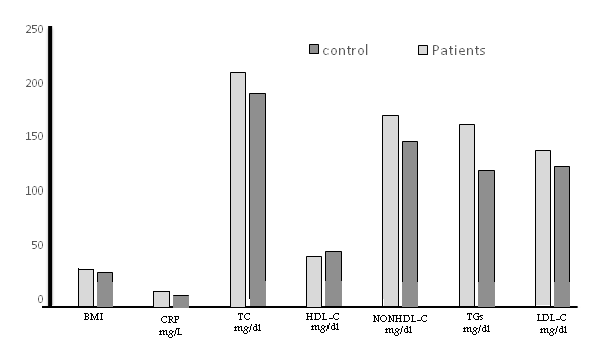
Table (1) and Figure (1) represents the mean concentration of study parameters comparison in patients versus control, as fellow:
- 1 A significant increase in the mean concentration of total cholesterol in patients than controls, being 209.83 ± 44.23 mg/dl and 190.71 ± 16.35 mg/dl for patients and controls respectively, (P-value 0.000). A significant increase in the mean of triglycerides concentration over control value was also seen, being 161.96 ± 57.28 mg/dl and 118.66 ± 25.91 mg/dl for patients and controls respectively, (P-value 0.000).
- 2 A significant decrease in patients means serum HDL-C concentration compared with the control value, being 39.7 ± 9.92 mg/dl and 44.44 ± 5.00 mg/dl for patients and controls respectively, (P-value 0.000), by contrast, a significant increase in the mean of concentration of non-HDL-C over control value was seen, being 170.13 ± 41.78 mg/dl and 146.27 ± 17.58 mg/dl for patients and controls respectively, (P-value 0.000).
- 3 A significant increase in the mean concentration of LDL-C in patients than controls, being 137.71 ± 36.73 mg/dl and 122.47 ± 16.19 mg/dl for patients and controls, (P-value 0.000). Also, a significant increase in the mean of CRP concentration over the control value was seen, being 7.38 ± 4.08 mg/dl and 4.13 ± 4.08 mg/dl for patients and controls respectively, (P-value 0.000).
- 4 A significant increase in the mean of BMI over control value, being 27.69 ± 5.56 and 24.89 ± 3.41 for patients and controls respectively, (P-value 0.000).
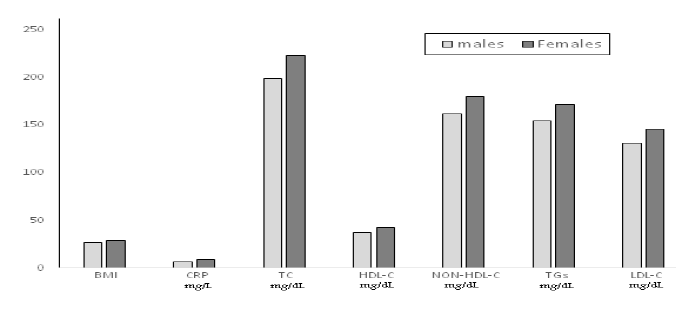
Table (2) and Figure (2) show the values of variables in male and female patients. It revealed a significant increase in BMI, CRP, TC, HDL-C, non-HDL-C, TGs, and LDL-C in female patients compared with male patients. In which the mean concentration of total cholesterol 198.9 ± 39.4 mg/dl for males and 222.5 ± 46.5mg/dl for females (P-value 0.003) , and the mean concentration of HDL-C 37.1 ± 9.6 mg/dl for males and 42.7 ± 9.5 mg/dl for females (P-value 0.0280) , and the mean concentration of non-HDL-C 161.8 ± 38.5 mg/dl and179.8 ± 43.7 mg/dl for males and females respectively , (P-value 0.026) , and the mean concentration of LDL-C 131.1 ± 34.3 mg/dl for males and 145.5 ± 38.3 mg/dl for females (P-value 0.014) . The mean concentration of CRP 6.2 ± 3.4 mg/L and 8.7 ± 4.5 mg/L for males and females respectively, (P-value 0.037). The mean value of BMI 26.5 ± 5.1 for males and 29.1 ± 5.8 for females (P-value 0.014). Table (3) represents a correlation between CRP and study variables. In which there was a highly significant correlation between CRP and BMI, TC, non-HDL-C, TGs, LDL-C.
|
Variables |
Cases (Mean ± SD) N=104 |
Control (Mean ± SD) N=104 |
P-value |
|
BMI |
27.69 ± 5.56 |
24.89 ± 3.41 |
0.000 |
|
CRP (mg/L) |
7.38 ± 4.08 |
4.13 ± 4.08 |
0.000 |
|
Total Cholesterol (mg/d) |
209.83 ± 44.23 |
190.71 ± 16.35 |
0.000 |
|
HDL (mg/dl) |
39.70 ± 9.92 |
44.44 ± 5.00 |
0.000 |
|
NON-HDL (mg/dl) |
170.13 ± 41.78 |
146.27 ± 17.58 |
0.000 |
|
Triglycerides (mg/dl) |
161.96 ± 57.28 |
118.66 ± 25.91 |
0.000 |
|
LDL (mg/dl) |
137.71 ± 36.73 |
122.47 ± 16.19 |
0.000 |
Table 1: Mean concentration of study parameters comparison in cases versus control group.
|
Parameters |
Patients Male (Mean ± SD) |
Patients female (Mean ± SD) |
P-value |
|
BMI |
26.5 ± 5.1 |
29.1 ± 5.8 |
0.014 |
|
CRP (mg/L) |
6.2 ± 3.4 |
8.7 ± 4.5 |
0.037 |
|
Total Cholesterol (mg/d) |
198.9 ± 39.4 |
222.5 ± 46.5 |
0.003 |
|
HDL (mg/dl) |
37.1 ± 9.6 |
42.7 ± 9.5 |
0.028 |
|
NON-HDL (mg/dl) |
161.8 ± 38.5 |
179.8 ± 43.7 |
0.026 |
|
Triglycerides (mg/dl) |
154.0 ± 171.3 |
171.3 ± 55.5 |
0.046 |
|
LDL (mg/dl) |
131.1 ± 34.3 |
145.5 ± 38.3 |
0.014 |
Table 2: Mean concentration of study parameters comparison in male and female patient.
|
Parameters |
R-value |
P-value |
|
BMI |
0.377** |
0.000 |
|
Total Cholesterol (mg/d) |
0.331** |
0.001 |
|
HDL (mg/dl) |
0.06 |
0.548 |
|
NON-HDL (mg/dl) |
0.336** |
0.000 |
|
Triglycerides ( mg/dl) |
0.389** |
0.000 |
|
LDL (mg/dl) |
0.260** |
0.008 |
** Highly significance
Table 3: correlation between CRP levels and study parameters.
4. Discussion
Diabetes is characterized by chronic hyperglycemia and disturbances of carbohydrate, lipid, and protein metabolism. Many studies have established that complications are mainly due to chronic hyperglycemia that exerts its effects through several mechanisms including dyslipidemia, platelet activation, and altered endothelial metabolism [11]. Deregulated lipid metabolism in type2 diabetes mellitus has been reported in many studies. Elevated mean total cholesterol, triglycerides, LDL-C, and lower HDL-C levels have been described in diabetes when compared with healthy non-diabetics [12], which is in line with our findings which is showed significantly higher mean serum levels of total cholesterol, triglycerides, LDL-C, and lower HDL-C in T2DM patients when compared with non-diabetics group. In diabetes, many factors may affect blood lipids levels because of the interrelationship between carbohydrate and lipid metabolism. Therefore, any disorder in carbohydrate metabolism leads to a disorder in lipid metabolism and vice versa. However, several studies showed that insulin affects the liver lipoproteins production and regulates the enzymatic activity of lipoprotein lipase and cholesterol ester transport protein, which is causes dyslipidemia in diabetes mellitus. Moreover, insulin deficiency may reduce the activity of hepatic lipase and several steps in the production of biologically active lipoprotein lipase [13].
Hypertriglyceridemia usually accompanies decreased HDL-C, which is also a prominent feature of plasma lipid abnormalities seen in an individual with diabetes. The possible mechanism responsible for hypertriglyceridemia may be due to increased hepatic secretion of very-low-density lipoprotein(VLDL) and delayed clearance of triglyceride-rich lipoproteins, which predominantly due to increased levels of substrate for triglycerides production, free fatty acids, and glucose [14]. In this study, a higher prevalence of obesity and overweight were observed in the diabetic group. This high prevalence supports the link between T2DM and obesity and had been reported to be a common finding in diabetic patients [15]. It has been well known that glucose disposal by lean body mass is markedly reduced and glucose metabolism was impaired in obese adults, while plasma concentration of non-esterified fatty acids and blood glycerol were high due to insulin resistance. Our finding of raised CRP in Sudanese withT2DM is consistent with studies in other populations [10, 16]. High CRP, dyslipidemia and LDL-C are reported to be the main risk factors for the chronic complications of T2DM. Prevalence of obesity and overweight in our study, together with elevation of triglycerides and CRP, suggests the coexistence of dysregulated lipids metabolism and inflammation in diabetes patients. Obesity in diabetic patients affects the CRP levels probably through hormonal changes linked to obesity. The high serum CRP concentration in diabetes reported in this study and by other authors could be due to an increase in adipose tissue mass that enhances cytokines production by adipocytes, cytokines production is known to stimulate the hepatic synthesis of CRP [17]. In this study, following other studies [18, 19] we observed a significant correlation between BMI and serum concentration of CRP in T2DM patients. It has been suggested that obesity and hyperglycemia induce oxidative stress [20], which results in the generation of free radicals in diabetic patients that could cause damage to the cell membrane and hence are associated with elevation of CRP a mediator of inflammation. Therefore, the effect of obesity and hyperglycemia could underline the elevation of c-reactive protein.
In this study lipid profile, BMI and CRP were higher in women compared with aging men. However, adverse changes induced by T2DM in HDL-C, LDL-C are more pronounced in women than men. In a recent study [21], significantly higher levels of total cholesterol and LDL-C were observed in female diabetics when compared with their male counterparts. These observations agree with earlier studies [22]. Several clinical studies suggested that their metabolic interaction between insulin and female sex hormones, for example, the low levels of female sex steroids associated with menopause are related to a decline in whole-body insulin-mediated glucose uptake. However, the exact cellular mechanisms behind this state of insulin resistance and the role of low female sex steroids are not fully understood [23]. Therefore, the decline in ovarian steroid function could result in alteration in circulating insulin levels and/or insulin receptor sensitivity. These disturbances of glucose homeostasis after ovariectomy were associated with serious derangement in lipid profile as indicated by a significant increase in serum total cholesterol, triglycerides, and LDL-C. An earlier study [24] demonstrated that, at a younger age, the relative risk of hypercholesterolemia is lower in women compared with men. During menopause total cholesterol and LDL-C levels rise by 10 and 14% respectively. Above 60 years of age, mean LDL-C is higher in women compared with men. At all ages, HDL-C levels are 0.26 to 0.36mmol/L higher in women compared with aging men. A recent study [25] reported that central obesity with an increase in visceral fats occurs more frequently after menopause, with a higher presence of comorbid risk factors and components of metabolic syndrome in women compared with aging men. However, abdominal visceral adipocytes produce systemic IL-6, IL-1, and TNF-α. Consequently, adipose tissue could play important role in the regulation of circulating CRP levels via interleukin-6 (IL-6) production. This study has a range of limitations it is a relatively small sample size. The clinical evidence such as HBA-1C and liver enzymes particularly ALT and AST levels were not assessed in our participants.
5. Conclusion
In this study T2DM induced hyperlipidemia such as hypercholesterolemia, hypertriglyceridemia, elevated LDL-C, and decreased HDL-C. Also, higher serum levels of CRP and its combination with obesity and overweight were significantly associated with an incident of T2DM. The study has shown that mean lipid profile components, obesity, overweight, and CRP were significantly higher in female diabetes when compared with their male counterparts. However, the prevalence of obesity and overweight in our study, together with elevation of lipid profile components and CRP, concludes the coexistence of dysregulated lipids metabolism, overweight, obesity, and inflammation in diabetes patients. Further research in a large study population of type2 diabetics is needed to test our findings.
Acknowledgment
We would like to thank the staff members of the Department of Biochemistry, College of Veterinary medicine, the University of Bahri for their support during the study.
Conflict of Interest
Authors declare they have no competing interest.
Funding
This work did not receive any fund.
References
- Inada H, Li Q, Bachani A, et al. Forecasting global road traffic injury mortality for 2030. Inj Prev 26 (2020): 339-343.
- Brugos-Larumbe A, Aldaz-Herce P, Guillen-Grima F, et al. Assessing variability in compliance with recommendations given by the International Diabetes Federation (IDF) for patients with type 2 diabetes in primary care using electronic records. The APNA study. Prim Care Diabetes 12 (2018): 34-44.
- Bertoni AG, Burke GL, Owusu JA, et al. Inflammation and the incidence of type 2 diabetes: The Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 33 (2010): 804-810.
- Su SC, Pei D, Hsieh CH, et al. Circulating pro-inflammatory cytokines and adiponectin in young men with type 2 diabetes. Acta Diabetol 48 (2011): 113-119.
- Naser W, Adam I, Rayis DA, et al. Serum magnesium and high-sensitivity C-reactive protein as a predictor for gestational diabetes mellitus in Sudanese pregnant women. BMC Pregnancy Childbirth 19 (2019): 1-5.
- Kanmani S, Kwon M, Shin MK, et al. Association of C-Reactive Protein with Risk of Developing Type 2 Diabetes Mellitus, and Role of Obesity and Hypertension: A Large Population-Based Korean Cohort Study. Sci Rep 9 (2019): 1-8.
- Made Junior Rina Artha I, Bhargah A, Dharmawan NK, et al. High level of individual lipid profile and lipid ratio as a predictive marker of poor glycemic control in type-2 diabetes mellitus. Vasc Health Risk Manag 15 (2019): 149-157.
- Elnasri HA, Ahmed AM. Patterns of lipid changes among type 2 diabetes patients in Sudan. East Mediterr Heal J 14 (2008): 314-324
- Ozder A. Lipid profile abnormalities seen in T2DM patients in primary healthcare in Turkey: A cross-sectional study. Lipids Health Dis 13 (2014): 1-6.
- Dongway AC, Faggad AS, Zaki HY, et al. C-reactive protein is associated with low-density lipoprotein cholesterol and obesity in type 2 diabetic Sudanese. Diabetes, Metab Syndr Obes Targets Ther 8 (2015): 427-435.
- Taskinen MR. Diabetic dyslipidaemia: From basic research to clinical practice. Diabetologia 46 (2003): 733-749.
- Yadav NK, Thanpari C, Shrewastwa MK, et al. Comparison of lipid profile in type-2 obese diabetics and obese non-diabetic individuals. A hospital based study from Western Nepal. Kathmandu Univ Med J 10 (2012): 44-47.
- Sunil B, Ashraf AP. Dyslipidemia in Pediatric Type 2 Diabetes Mellitus. Curr Diab Rep 20 (2020): 1-9.
- Basu D, Bornfeldt KE. Hypertriglyceridemia and Atherosclerosis: Using Human Research to Guide Mechanistic Studies in Animal Models. Front Endocrinol (Lausanne) 11 (2020): 1-19.
- Bays HE, Chapman RH, Grandy S. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: Comparison of data from two national surveys. Int J Clin Pract 61 (2007): 737-747.
- Wen J, Liang Y, Wang F, et al. C-reactive protein, gamma-glutamyltransferase and type 2 diabetes in a Chinese population. Clin Chim Acta 411 (2010): 198-203.
- Sabanayagam C, Shankar A, Lim SC, et al. Serum C-reactive protein level and prediabetes in two Asian populations. Diabetologia 54 (2011): 767-775.
- Barchetta I, Cimini FA, Ciccarelli G, et al. Sick fat: the good and the bad of old and new circulating markers of adipose tissue inflammation. J Endocrinol Invest 42 (2019): 1257-1272.
- Bawadi H, Katkhouda R, Tayyem R, et al. Abdominal fat is directly associated with inflammation in persons with type-2 diabetes regardless of glycemic control - a jordanian study. Diabetes, Metab Syndr Obes Targets Ther 12 (2019): 2411-2417.
- Furukawa S, Fujita T, Shimabukuro M, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 114 (2004): 1752-1761.
- Aderibigbe MA, Obafemi TO, Olaleye MT, et al. Effects of gender, age and treatment duration on lipid profile and renal function indices in diabetic patients attending a teaching hospital in South-Western Nigeria. Afr Health Sci 18 (2018): 900-908.
- Agulló V, Domínguez-Perles R, García-Viguera C. Sweetener influences plasma concentration of flavonoids in humans after an acute intake of a new (poly) phenol-rich beverage. Nutr Metab Cardiovasc Dis 31 (2021): 930-938.
- Clegg DJ, Brown LM, Woods SC, et al. Erratum: Gonadal hormones determine sensitivity to central leptin and insulin (Diabetes (2006) 55 (978-987)). Diabetes 56 (2007): 2649
- Sánchez-Rodríguez MA, Zacarías-Flores M, Castrejón-Delgado L, et al. Effects of hormone therapy on oxidative stress in postmenopausal women with metabolic syndrome. Int J Mol Sci 17 (2016).
- Kip KE, Marroquin OC, Kelley DE, et al. Clinical Importance of Obesity Versus the Metabolic Syndrome in Cardiovascular Risk in Women: A Report from the Women’s Ischemia Syndrome Evaluation (WISE) Study. Circulation 109 (2004): 706-713.