Application of the Clinical Reasoning Process for the Rehabilitation of a Case with Cervicogenic Pain
Article Information
Md Waliul Islam1*, Md Kutub Uddin2, Faruq Ahmed1, Md Shujayt Gani1, Mohammad Nazmul Hasan1, Md Jubair Hassan3
1Department of Physiotherapy, Centre for the Rehabilitation of the Paralised,Dhaka, Bangladesh
2Department of Physiotherapy,SAIC College of Medical Science & Technology, Dhaka, Bangladesh
3Handicap International (Humanity & Inclusion), Bangladesh
*Corresponding author: Md Waliul Islam, Department of Physiotherapy, Centre for the Rehabilitation of the Paralised, Bangladesh. Email: olee32@gmail.com
Received: 11 August 2022; Accepted: 19 August 2022; Published: 19 September 2022
Citation: Md Waliul Islam, Md Kutub Uddin,Faruq Ahmed, Md Shujayt Gani, MohammadNazmul Hasan, Md Jubair Hassan. Application of the Clinical Reasoning Process for the Rehabilitation of a Case with Cervicogenic Pain. Fortune Journal of Health Sciences 5 (2022): 539-543.
View / Download Pdf Share at FacebookAbstract
Background: The method through which a therapist engages with a patient is known as clinical reasoning. During this process, the therapist gathers data, develops, and tests hypotheses, and then uses this data to determine the best course of action for diagnosis and therapy. It is described as an inferential procedure used by practitioners to gather and assess information and make decisions on the diagnosis and treatment of patient problems.
Aim: The aim of this study is to describe the rehabilitation of a solo case with cervical radiculopathy by using clinical reasoning process
Method: A case study of typical cervical radiculopathy managed by using clinical reasoning process and advance evidence-based physiotherapy treatment to reduce pain, increase ROM and improve functional ability.
Result: After six weeks of treatment, there was a reduction in pain, an increase in range of motion, and a change in disability status as measured by the neck disability index.
Conclusion: Finally, this case study states that application of the clinical reasoning process is beneficial for rehabilitation programs.
Keywords
Cervical radiculopathy, Hypothetico deductive reasoning, Neck Disability Index
Article Details
1. Background
Clinical reasoning, which integrates cognitive thinking and the decision-making process of health professionals, takes place throughout a practitioner's professional career [1]. Clinical reasoning is a process in which a therapist works with the patient and relevant parties and facts, as well as with the patient, a multidisciplinary team goal, management or organization strategic plan based on the clinical report and the data provided by the patient, client choice and expert judgment, knowledge, and experience. Despite the complexity of various facts and circumstances, clinical reasoning enables a practitioner to come to the optimal decision for the improvement of patient health, which is why it is referred to as a wise decision. [2].
Neck pain is the second most prevalent musculoskeletal condition experienced by the general population who has musculoskeletal pathology, behind low back pain. [3]. According to literature, statistics show that five people out of ten people experience neck pain every year, and more than 60 percent of the population experiences neck pain at a certain period of life. Half of the people will not fully recover from chronic neck pain symptoms [4]. The current study aims to explore the understanding of clinical reasoning by solving a single case of cervical pathology.
2. History
This case was about 47 years old. She was a housewife. She came to the physiotherapy department with her daughter as her husband was staying abroad. Her chief complaints were pain, weakness, and numbness radiating from her right arm and some forearm and difficulty in daily living activities for 3 months. Initially, it was localized and tolerable, but gradually it worsened and now she has difficulty sleeping. She took medicine prescribed by a general practitioner, but it was only symptomatic relief for a short time.
2.1 Baseline assessment
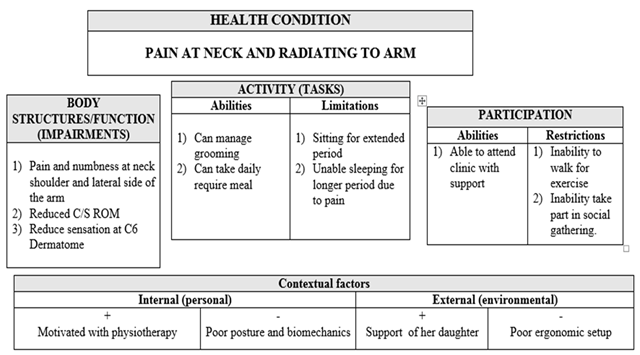
Client came with the complaint of pain, weakness and mild numbness was her impairment. That caused by anatomical and body function restriction. She was not able to maintain her activity of daily living due to her disability. She also limited her social participation live attending the social program, tour, etc.
As impairments in body structure and functions, patient came to me complained of intermittent severe radiating pain and mild numbness at her right upper limb for about 3.5 months that day by day increases. She also noticed that her pain as like as electric shock which make his life untearable. On assessment, her pain at the right side of the neck and severe radiating at the lateral aspect of the forearm and intermittent mild numbness at the thumb and index finger. According to VAS scale, resting was 8 out of 10 and mild decrease range of motion of cervical right-side rotation, side bending and flexion. There is no muscle wasting as well as reflex also normal. The activity limitation include pain aggravated by household activities such as washing clothes, cooking and watching TV program. She also faced participation restriction as like social gathering, family program. Her environmental factor was poor ergonomics set up of kitchen, place of TV and her daily activities. All of these difficulties and situation make him depressed, worried and less confidence. I found her neck disability index (NDI) was 41%, which indicates severe disability.
3. Hypothetico deductive reasoning
As this was a complex case to detect initially, diagnosis and management plan carried out systematically. Even though there was, propositional knowledge but there is limited non-propositional knowledge about this case
Cue acquisition: Initially patient asked many questions and gathered answer to find out the best possible clue that related to my case. Those questions given below:
- Is the pain constant, intermittent, and early morning stiffness & sleep disturbance? The reason for asking this question to identify causes of pain such as mechanical, non-mechanical, pathological involvement or any kind of arthritis.
- Is the pain gradual or sudden onset and unilateral or bilateral referred? The intendant to ask this question was to detect the source of symptoms.
- Which activities aggravate or relieve your symptom?
- Which site are you fell pain at first? These two questions asked for to identify the exact which structure is involved and to see the severity of symptom.
- Can you explain me your nature of pain such as burning, tingling, dull-aching, electric shock & lancinating like? This question asked to understand the characteristics and nature of pain so that I can easily distinguish between somatic, visceral or radicular pain.
- Does your pain influence by cough, sneezing or deep breathing? This question asked to see the relationship with dural involvement.
- Any sequence of trauma or fell disturbance during walking? This question asked to find out any cord compression.
4. Hypothesis generation:
Hypothesis generation was vital part of the systematic problem-solving process. It was an inductive reasoning, which provides a set of specific observation to a generalization. After cue, acquisition and getting the answers few hypothesis enerated in the clinician mind, which are given below:
- There may have an association of pathological cause due to early morning stiffness and sleep disturbance influence this hypothesis
- Thoracic outlet syndrome may be another reason, intermittent numbness at her thumb and radiating pain at right forearm indicates this hypothesis.
- Cervical spondylosis may have strong relationship of symptom. Patient’s age, gradual onset and radiating pain may have probabilities this hypothesis.
- Cervical discs prolapse with C6 radicular symptom may be main pain generator source. Pain on coughing and intermittent unilateral symptom such as numbness, radiating pain. In addition, pain characteristics was electric shock like and lancinating type pain according to the dermatome distribution. All these provocative this hypothesis
- Cue interpretation:
It involves in appropriately evaluating which cues are most relevant to my specific hypothesis under consideration. According to evidence a three-point scale for cue interpretation where ‘+1’ cue confirms hypothesis, ‘-1’ disconfirms hypothesis and ‘0’ cue does not contribute to hypothesis [5]. The cue interpretation is given below:
- Patient had no significant weight loss, pyrexia, systemic illness and pathological report. In this way the hypothesis of pathological involvement disconfirms (-1).
- Even though, there is radiating pain at the lateral aspect of the forearm and thumb, the adson’s test (specificity 87% and sensitivity 94%) was negative and X-ray do not show any cervical rib [6].
- The radiological findings do not show any degenerative change such as osteophytic formation, intervertebral discs space. These finding exclude the possibilities of cervical spondylosis.
- The Dural symptom (pain on coughing) was positive. Clinicians perform spurling test (40%-60% Sensitivity, 85%-95% specificity) by lateral flexion and rotation to the affected side with axial compression of the head reproduces radicular pain and found positive. Clinician also performed neck distraction test (40%-50% Sensitivity, 90% specificity) and found relief of radicular symptoms when grasps patient’s head under occiput and chin and then lifts, applying axial traction [7]. Examiner also noticed that her pain location according to the C6 nerve root that means pain at the neck, lateral aspect of the forearm and first and second digit. Examiner also performed upper limb tension test (ULNT1) for C6 symptom, and this test done by shoulder depression, shoulder abduction 110°, wrist and finger extension, shoulder lateral rotation, elbow extension, contralateral lateral flexion of the cervical spine where the sensitivity of 0.97 and a specificity of 0.69 [8]. Moreover, active range of motion of cervical ipsilateral rotation, lateral flexion decreased. Conversely, Babinski sign was negative. All of these cues strongly confirm the hypothesis no IV (+1).
4. Hypothesis evaluation:
The final stage of hypothetico deductive approach was hypothesis evaluation. Clinician weighing up the advantage and disadvantage of each possible explanation for patient’s sign and symptom and choosing the favored one by the evidence. After completion of all ideas, hypothesis number IV support the evidence. Thoomes et al. (2018) stated that although radiculopathy and radicular commonly occur together, radiculopathy can occur in the absence of pain, and radicular pain can occur in the absence of radiculopathy. Radicular pain is usually caused by compression of the nerve root due to cervical disc herniation. The pain quality was lancinating and electric shock like which is radicular pain. A double blinded randomized clinical trial (RCT) to find out the efficacy of neural mobilization with manual cervical traction (NMCT) for reducing cervical radiculopathy patient’s pain. They found significant difference between control group and experimental group and suggested that NMCT can pain relief and increase range of motion. Experimental group received manual cervical traction simultaneously with neural mobilization and conventional physiotherapy and control group received manual cervical traction along with conventional physiotherapy [9].
5. Intervention
Intervention was started with the Mckenzie Mechanical Diagnosis and Therapy (MDT) of cervical spine. Then neural mobilization with manual traction, cervical stability training and postural reeducation. The description of these interventions is given below.
Neural mobilization with cervical traction (NMCT): Manual spinal traction and neural mobilization are administered by two physical therapists while they are both lying down. The slider technique is used to mobilize neural tissue. For one minute, the mobilization is applied smoothly and rhythmically. Between each pair of repeats, there was a 30-second break. For ten minutes, the maneuver is performed six more times To slide the median nerve, the patient's shoulder is abducted to 90 degrees and laterally rotated. Elbow flexion (which unloads the median nerve) is alternated with wrist and finger extension (which loads the median nerve), and elbow extension (which loads the median nerve) is alternated with wrist and finger flexion (which unloads the median nerve) for six sets of repetitions. There was a 30-second break in between each series of slow, oscillatory movements. Six sessions per week for two weeks.
6. Outcome measurement
Outcome measurement tool included visual analogue scale (VAS) for pain intensity Goniometer for range of motion (ROM) and Manual muscle testing technique by using OXFORD muscle grade scale to assess the muscle strength of cervical spine. The reliability of VAS is 0.94 [11].
On the other hand, Neck Disability Index (NDI) measured disability. NDI is a commonly used outcome measure to demonstrate the actual level of disability among patients with neck pain and also it has higher level of validity and reliability.
Table 2: Outcome measurement
|
Timeline > /Variable |
Assessment (1st day) |
Mid way (3rd week) |
Final (6th week) |
Measurement tools |
|
Pain |
||||
|
Resting pain |
7 |
2 |
1 |
VAS scale |
|
Pain with activity |
9 |
6 |
1 |
|
|
Manual muscle testing (MMT) of cervical spine |
||||
|
Flexion |
3 |
3+ |
4 |
Manual muscle testing (MMT) |
|
Extension |
3 |
3 |
4 |
|
|
Right flexion |
3 |
3+ |
4 |
|
|
Left flexion |
3 |
3 |
4 |
|
|
Right rotation |
3 |
3+ |
4 |
|
|
Left rotation |
3 |
3+ |
4 |
|
|
Disability status in neck disability index (NDI) |
||||
|
Disability status |
55 % |
35% |
20% |
NDI |
Discussion
Among the musculoskeletal disorders, cervical radiculopathy is one of the most painful clinical scenarios. Patients suffering from radiculopathy typically have symptoms such as neck pain, arm pain, or both. In the current study, the diagnosis of this condition was made with a single case. This includes an overview of the overall findings on the patient's history and physical examination. The study discussed relevant clinical syndromes. The natural history of cervical radiculopathy is reviewed, and evidence-based management is discussed. Clinical reasoning in physical therapy refers to professional judgments made before, during, and after clinical sessions, and it promotes professional autonomy [12]. This method is a content-specific procedure that needs rules and text- and context-specific information. The types of change are based on various clinical conditions or issues. To decide the next step in the protocol, it involves comparing, testing, and analyzing the case.
Conclusion:
Finally, this case study states that application of the clinical reasoning process is beneficial for rehabilitation programs. In addition, the application and clinical reasoning processes can be useful and cost-effective. This cycle continues until the desired outcome is obtained.
Author contributions
Md. Waliul Islam: Critical intellectual input, read and approval of the final submission, study concept and design, methodology, writing manuscript draft, study supervision.
Faruq Ahmed: Critical intellectual input, read and approval of the final submission, study concept and design, methodology.
Md. Kutub Uddin: Critical intellectual input, read and approval of the final submission, revision for critically intellectual content.
Mohammad Nazmul Hasan: Critical intellectual input, read and approval of the final submission, writing manuscript draft.
Md Shujayt Gani: Critical intellectual input, read and approval of the final sub- mission, study concept and design, methodology.
Md. Jubair Hassan: Critical intellectual input, read and approval of the final sub- mission, study concept and design, methodology.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
ORCID
https://orcid.org/0000-0003-1062-5349
https://orcid.org/0000-0003-0239-0113
https://orcid.org/ 0000-0001-8241-815
References
- Banning M. Clinical reasoning and its application to nursing: Concepts and research studies. Nurse education in practice. 2008 May 1;8(3):177-83.
- Eva KW. What every teacher needs to know about clinical reasoning. Medical education. 2005 Jan;39(1):98-106.
- Al-Hadidi F, Bsisu I, AlRyalat SA, Al-Zu’bi B, Bsisu R, Hamdan M, Kanaan T, Yasin M, Samarah O. Association between mobile phone use and neck pain in university students: A cross-sectional study using numeric rating scale for evaluation of neck pain. PloS one. 2019 May 20;14(5): e0217231.
- Hoy D, Protani M, De R, Buchbinder R. The epidemiology of neck pain. Best practice & research Clinical rheumatology. 2010 Dec 1;24(6):783-92.
- Cunningham S, Litwin B, Fernandez-Fernandez A, Canbek J. Influence of residency training on the clinical reasoning development of Kenyan physiotherapists. Journal of Manual & Manipulative Therapy 27 (2019): 237-44.
- Dessureault-Dober I, Bronchti G, Bussieres A. Diagnostic accuracy of clinical tests for neurogenic and vascular thoracic outlet syndrome: a systematic review. Journal of Manipulative and Physiological Therapeutics 41 (2018): 789-99.
- Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. an updated list of essential items for reporting diagnostic accuracy studies. Clinical chemistry 61 (2015): 1446-52.
- Apelby-Albrecht M, Andersson L, Kleiva IW, Kvåle K, Skillgate E, Josephson A. Concordance of upper limb neurodynamic tests with medical examination and magnetic resonance imaging in patients with cervical radiculopathy: a diagnostic cohort study. Journal of manipulative and physiological therapeutics 36 (2013): 626-32.
- Kim DG, Chung SH, Jung HB. The effects of neural mobilization on cervical radiculopathy patients’ pain, disability, ROM, and deep flexor endurance. Journal of back and musculoskeletal rehabilitation 30 (2017): 951-9.
- Clare HA, Adams R, Maher CG. Reliability of McKenzie classification of patients with cervical or lumbar pain. Journal of Manipulative and Physiological therapeutics 28 (2005): 122-7.
- Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis care & research 63 (2011): S240-52.
- Öberg U, Hörnsten Å, Isaksson U. The Self-Management Assessment Scale: Development and psychometric testing of a screening instrument for person-centred guidance and self-management support. Nursing Open 6 (2019): 504-13.