Analysing the clinical relevance and impact of subsidence seen with standalone cages for cervical disc surgeries – A study of fusion rates in 118 patients
Article Information
Vishnu Vikraman Nair1*, Vishal Kundnani2, Mukul Jain1, Sunil Shamjibhai Chodavadiya1, Abhijit Shetty1, Jenil Patel1, Nikhil Dewnany3
1FELLOW in Spine Surgery, Department of Orthopaedics, Bombay hospital and medical research institute
2Consultant Spine Surgeon, Department of Orthopaedics, Bombay hospital and medical research institute
3MBBS, K J Somaiya medical college, Mumbai
*Corresponding Author: Dr Vishnu Vikraman Nair, FELLOW in Spine Surgery, Department of Orthopaedics, Bombay hospital and medical research institute.
Received: 21 June 2023; Accepted: 26 June 2023; Published: 28 June 2023
Citation: Vishnu Vikraman Nair, Vishal Kundnani, Mukul Jain, Sunil Shamjibhai Chodavadiya, Abhijit Shetty, Jenil Patel, Nikhil Dewnany. Analysing the clinical relevance and impact of subsidence seen with stand-alone cages for cervical disc surgeries – A study of fusion rates in 118 patients. Journal of Spine Research and Surgery 5 (2023): 51-57.
View / Download Pdf Share at FacebookAbstract
Background and Aim:
The objective of this study is to examine the short and long term impact of subsidence after anterior cervical discectomy and fusion for compressive cervical disc disease, utilizing solely non-locking stand-alone titanium cage and to analyze the fusion rates.
Methods:
The single-center retrospective study included one and two-level Anterior cervical discectomy and fusion (ACDF) cases from July 2014 to June 2019. Minimum 2-year follow-up was included and titanium cage with autologous bone graft was used. Interbody height (IBH), subsidence and fusion rates were analysed at follow up. Clinically, VAS score for neck and arm, mJOA score for myelopathy, C2-C7 cobb angle for lordosis improvement were analyzed.
Results:
A sample of 118 patients, was subjected to analysis. The fusion rate was observed to be 96.6%. Eleven instances of subsidence were observed at the 3-month follow-up (p= 0.89). All 11 patients with subsidence had excellent/good functional outcomes on analyzing Odom’s criteria. The study observed a noteworthy enhancement in the (VAS) for neck and arm pain, as well as in the (mJOA) score among patients with myelopathy, with a statistical significance of p<0.05. There was significant reduction in IBH in the subsidence group in comparison to non-subsidence group. Segmental kyphosis angles were also seen to be higher in the subsidence group(p<0.05)
Conclusion:
According to our study, the subsidence observed did not have a significant clinical impact on outcome scores or patient satisfaction. The utilisation of a stand-alone cage devoid of screw or plate instrumentation has demonstrated favourable long-term outcomes with nearly complete fusion rates. Furthermore, there is no significant difference in outcomes between the subsidence and non-subsidence groups.
Keywords
Subsidence; Standalone Cage; ACDF; cervical DDD; Titanium; Discectomy; Fusion
articles about Subsidence Research articles about Subsidence review articles about SubsidenceSubsidence PubMed articles Subsidence PubMed Central articles Subsidence 2024 articles Subsidence 2025 articles Subsidence Scopus articles Subsidence impact factor journals Subsidence Scopus journals Subsidence PubMed journals Subsidence medical journals Subsidence free journals Subsidence best journals Subsidence top journals Subsidence free medical journals Subsidence famous journals Subsidence Google Scholar indexed journals articles about Standalone Cage Research articles about Standalone Cage review articles about Standalone CageStandalone Cage PubMed articles Standalone Cage PubMed Central articles Standalone Cage 2025 articles Standalone Cage 2026 articles Standalone Cage Scopus articles Standalone Cage impact factor journals Standalone Cage Scopus journals Standalone Cage PubMed journals Standalone Cage medical journals Standalone Cage free journals Standalone Cage best journals Standalone Cage top journals Standalone Cage free medical journals Standalone Cage famous journals Standalone Cage Google Scholar indexed journals articles about ACDF Research articles about ACDF review articles about ACDFACDF PubMed articles ACDF PubMed Central articles ACDF 2026 articles ACDF 2027 articles ACDF Scopus articles ACDF impact factor journals ACDF Scopus journals ACDF PubMed journals ACDF medical journals ACDF free journals ACDF best journals ACDF top journals ACDF free medical journals ACDF famous journals ACDF Google Scholar indexed journals articles about cervical DDD Research articles about cervical DDD review articles about cervical DDDcervical DDD PubMed articles cervical DDD PubMed Central articles cervical DDD 2027 articles cervical DDD 2028 articles cervical DDD Scopus articles cervical DDD impact factor journals cervical DDD Scopus journals cervical DDD PubMed journals cervical DDD medical journals cervical DDD free journals cervical DDD best journals cervical DDD top journals cervical DDD free medical journals cervical DDD famous journals cervical DDD Google Scholar indexed journals articles about Titanium Research articles about Titanium review articles about TitaniumTitanium PubMed articles Titanium PubMed Central articles Titanium 2028 articles Titanium 2029 articles Titanium Scopus articles Titanium impact factor journals Titanium Scopus journals Titanium PubMed journals Titanium medical journals Titanium free journals Titanium best journals Titanium top journals Titanium free medical journals Titanium famous journals Titanium Google Scholar indexed journals articles about Discectomy Research articles about Discectomy review articles about DiscectomyDiscectomy PubMed articles Discectomy PubMed Central articles Discectomy 2029 articles Discectomy 2030 articles Discectomy Scopus articles Discectomy impact factor journals Discectomy Scopus journals Discectomy PubMed journals Discectomy medical journals Discectomy free journals Discectomy best journals Discectomy top journals Discectomy free medical journals Discectomy famous journals Discectomy Google Scholar indexed journals articles about Fusion Research articles about Fusion review articles about FusionFusion PubMed articles Fusion PubMed Central articles Fusion 2030 articles Fusion 2031 articles Fusion Scopus articles Fusion impact factor journals Fusion Scopus journals Fusion PubMed journals Fusion medical journals Fusion free journals Fusion best journals Fusion top journals Fusion free medical journals Fusion famous journals Fusion Google Scholar indexed journals articles about MRI Research articles about MRI review articles about MRIMRI PubMed articles MRI PubMed Central articles MRI 2031 articles MRI 2032 articles MRI Scopus articles MRI impact factor journals MRI Scopus journals MRI PubMed journals MRI medical journals MRI free journals MRI best journals MRI top journals MRI free medical journals MRI famous journals MRI Google Scholar indexed journals articles about posterior longitudinal ligament Research articles about posterior longitudinal ligament review articles about posterior longitudinal ligamentposterior longitudinal ligament PubMed articles posterior longitudinal ligament PubMed Central articles posterior longitudinal ligament 2032 articles posterior longitudinal ligament 2033 articles posterior longitudinal ligament Scopus articles posterior longitudinal ligament impact factor journals posterior longitudinal ligament Scopus journals posterior longitudinal ligament PubMed journals posterior longitudinal ligament medical journals posterior longitudinal ligament free journals posterior longitudinal ligament best journals posterior longitudinal ligament top journals posterior longitudinal ligament free medical journals posterior longitudinal ligament famous journals posterior longitudinal ligament Google Scholar indexed journals
Article Details
Introduction
Anterior cervical discectomy and fusion (ACDF) is a frequently utilized surgical intervention for addressing compressive pathologies of the disc that result in neurological symptoms, whether they be single, double, or multi-level in nature. It is utilized for the treatment of a range of cervical spinal ailments, such as compressive myelopathy, herniated discs, degenerative disease, and trauma. ACDF is considered to be the most frequently performed surgical procedure in this domain[1,2]. In comparison to contemporary times, owing to technological progressions and enhanced surgical education, Anterior Cervical Discectomy and Fusion (ACDF) has displayed a reduced frequency of adverse events and has exhibited positive outcomes of fusion during the postoperative phase[4,5]. The objective of anterior cervical discectomy and fusion (ACDF) is to alleviate radicular pain and halt the advancement of myelopathy, which may result from the compression of neural structures. This is achieved by decompressing the affected spinal structures and stabilizing the impacted segments.
The isolated application of decompression has been found to elevate the likelihood of intervertebral space collapse, which subsequently leads to a reduction in neural foramen height due to an increase in kyphosis[6]. The utilization of iliac crest bone grafts in anterior cervical discectomy and fusion (ACDF) procedures was previously established as the standard of care, with the Smith and Robinson approach being widely acknowledged[3]. The surgeries were deemed unsuccessful due to increased donor site morbidity, substantial subsidence, resulting in a reduction in foramina height and an increase in kyphosis[7]. Consequently, interbody devices were employed to facilitate the preservation of interbody heigh and proper alignment.
Over the years the options for interbody fusion techniques became better with the use of autograft in isolation, the use of autograft in conjunction with anterior plating, and the use of allograft with or without anterior plating. The selection of methodology is contingent upon the quantity of disease stages and the specific diagnosis. The utilization of plate and screw fixation is a common practice in conjunction with multilevel cervical discectomy. This approach serves to preserve spinal curvature and enhance the rate of graft fusion[8]. Nevertheless, the utilization of plates and screws in surgical procedures may result in various complications, including screw breakage, screw pull-out, perforation of the esophagus, and injury to the spinal cord or nerves[9,10].
In recent times, the employment of a self-contained cage filled with local auto bone graft in ACDF has yielded positive outcomes[11,12][13]. reported that utilizing a stand-alone cage filled with local bone graft during anterior cervical discectomy and fusion (ACDF) yields favorable clinical and radiological results, while avoiding the potential complications and elevated expenses associated with iliac donor site usage. Nevertheless, certain complications such as nonunion and subsidence into the endplates have been documented in association with this procedure [11][14]. conducted a study on a stand-alone cage filled with cancellous iliac bone graft. The study revealed that 25.5% and 14.9% of the cases experienced subsidence and nonunion, respectively. Notwithstanding the potential hazards of subsidence and nonunion, the clinical outcomes were comparatively favorable in the respective groups, as per their reports.
The purpose of this present study is to see the functional outcomes of stand-alone alone cages to achieve bony fusion in ACDF surgeries and study the occurrence of subsidence and to evaluate any impact of radiological subsidence in the overall clinical outcomes on the patients.
Methods
This study retrospectively examined the medical records of 118 patients who underwent treatment for degenerative cervical spine disc disease using Anterior cervical discectomy and fusion (ACDF) with a stand-alone titanium cage. The analysis was conducted in a prospective manner. Prior to the surgical procedure, all patients were subjected to conservative treatment for a minimum duration of 3-6 months. The treatment regimen encompassed the utilization of non-steroidal anti-inflammatory drugs (NSAIDs), neuroprotective interventions such as Gabapentin/Pregabalin, and a comprehensive cervical spine rehabilitation programme that was overseen by a specialized physiotherapist. Surgical intervention was considered only for patients who did not experience relief from the conservative therapies mentioned earlier. The surgical interventions were performed by an individual surgeon at a sole medical institution.
Subsequent to the surgical intervention, patients were directed to utilize a cervical soft collar for a period of one week. Furthermore, conventional antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) were dispensed as deemed appropriate. Data pertaining to patient demographics, medical history, clinical symptoms, surgical technique, and post-operative outcomes and complications were systematically collected. Ethical approval from the local institutional review board was obtained prior to the commencement of this retrospective study. Informed consent was obtained from the patients with regards to the utilization of their data in future research studies.
Inclusion and Exclusion criteria
The present study involved patients who had undergone unsuccessful medical and conservative management for progressive or persistent radiculopathy and/or myelopathic symptoms. The inclusion criteria required confirmation of single or double level disc disease through plain X-ray and Magnetic Resonance Imaging (MRI) images, a minimum of 2 years of follow-up imaging and clinical data for enrolled patients, and the inclusion of patients who had developed acute neurological deficits.
The study's exclusion criteria involved patients with more than two affected levels, developmental stenosis of the cervical spine in combination with ossification of the posterior longitudinal ligament, prior cervical surgery, significant osteoporosis (as defined by a T score of less than -2.5 at dual-energy X-ray absorptiometry), infection, tumor, or deformity of the cervical spine.
Demographics
The present study is a retrospective investigation that entailed the retrieval of demographic information from patients' medical records, as well as plain X-ray and MRI scans of the cervical spine. The preoperative evaluation involved the utilization of plain radiographs and MRI of the cervical spine to assess the extent of degenerative disc disease and identify the cervical level affected. In addition, demographic data such as age, gender, symptomatology, and affected level were recorded. The recorded symptoms included neck pain, radiculopathy, and neurological impairments that exhibited a strong clinic-radiological correlation. The demographics that were gathered aided in furnishing a thorough depiction of the patient cohort that was encompassed in this investigation.
Surgical technique
During the administration of general anesthesia, the patient's head was rendered immobile using a horseshoe head support, while maintaining a supine position. Utilizing the Smith Robinson approach and fluoroscopy confirmation, a horizontal incision was executed at the disc level on the left side, granting access to the vertebrae. The methodology employed in this study entailed the utilization of a microscope to aid in the discectomy and decompression procedures. Additionally, a Caspar distractor was utilized to manipulate the adjacent vertebral bodies. The excision of ventral and dorsal, or dorsolateral, syndesmophytes was performed, along with the dissection and excision of the posterior longitudinal ligament as necessary. Adequate decompression of the nerve roots was confirmed. The process entailed the precise elimination of the cartilaginous end plates, with the objective of preserving the structural soundness of the osseous end plates. The dimensions of the cage were assessed using experimental cages, and the final cage was surgically implanted along with autologous bone graft obtained from osteophytes. No additional allograft or synthetic bone graft was utilized. After the final placement of the cage, the Caspar distractor was deactivated, and the stability of the cage was confirmed. Subsequent to the surgical intervention, the resumption of routine activities was promptly initiated, contingent upon the patient's individual tolerance threshold. The healthcare provider prescribed the use of a soft cervical collar for a duration of one week with the aim of averting undue extension.
Follow up and assessment
Prior to the surgical intervention, radiological and clinical monitoring was conducted. Postoperative follow-up assessments were conducted at 12 and 24 months. Prior to surgery, all patients underwent magnetic resonance imaging (MRI) scans of the cervical spine. During the follow-up appointments, radiological evaluation was conducted using plain X-ray imaging in both anterior-posterior and lateral projections, with a focus on the operated segment. If any irregularities were detected, supplementary lateral flexion-extension radiographs were conducted. A radiographic evaluation was conducted by an impartial interpreter to mitigate any potential bias. The radiographs were subjected to analysis, which involved the quantification of various parameters such as the absolute segmental height, kyphosis angle, subsidence and fusion. The measurement of the inter-body height ratio entails determining the combined vertical height of the two vertebral bodies that constitute the movement segment and dividing this value by the anterior-posterior (AP) diameter of the upper vertebral body, as observed on a lateral radiograph. This procedure mitigates the potential impact of magnification discrepancies on radiographic measurements. The absolute anteroposterior diameter of the upper vertebral body can be measured using pre-operative MRI scans. By utilizing this numerical quantity, the absolute segmental height can be computed for all radiographic images. The semiquantitative method is utilized to document the inclination towards subsidence. The term subsidence was operationally defined as a condition in which the cage penetrated the endplate with a depth exceeding 3 mm. The direction of subsidence is documented in instances where it occurs.
Clinical Outcomes
The clinical follow-up was conducted utilizing VAS (Visual analogue score), mJOA(modified Japanese Orthopaedic Association) and Odom's criteria, which involves assigning a grade ranging from excellent to poor across four distinct groups. The administration of (Odom I) was prescribed for patients who did not exhibit any cervical spine symptoms and whose daily activities were not impaired. The term "Good (Odom II)" refers to patients who experience intermittent discomfort, but do not experience any significant interference with their work. Fair (Odom III) classification was utilized to grade cases based on subjective improvement, while significant limitation of physical activities and no improvement or worse compared with the condition before surgery were indicative of poor outcomes (Odom IV) for patients.
Statistical Analysis
The statistical analysis was conducted utilizing SPSS version 17 for Windows, developed by SPSS Inc. located in Chicago, IL, USA. The data were reported in the format of mean values with their corresponding standard deviations. The paired t-test was utilized to identify significant disparities between the interbody height and segmental angle values obtained immediately after the operation and those obtained during the last follow-up. The statistical analysis employed in this study involved the utilization of two-tailed hypothesis testing, with a predetermined level of significance set at p ≤ 0.05.
Results
A total of 120 patients were included in the study and 2 patients were lost to follow up. A total of 118 cases ( 77 males, 41 females) were included in study.(Table 1) The level of fusion was single level in 86 cases, two level in 32 cases. Mean age of patients was 55.5±9.5 years (range 31- 70 years). All participants included in the study were subjected to a minimum follow-up period of 2 years, with an average follow-up duration of 5.3 years.
The average interbody height (IBH) recorded immediately after the surgical procedure was 29.81±0.69. However, the IBH value decreased to 27.61±0.71 mm during the final follow-up assessment. The study found that the average loss of interbody height (IBH) from the time immediately after surgery to the last follow-up was 2.20±0.70 mm. However, this difference was not statistically significant (p>0.05).
|
Variables |
Mean+ SD (n) |
P-value (>0.05 not significant) |
|
Number of patients |
118 |
>0.05 |
|
Age |
55.5 ± 9.5 |
>0.05 |
|
Gender |
77 (Male), 41 (Female) |
>0.05 |
|
Levels |
150 (Total) |
|
|
86 (Single levels) |
>0.05 |
|
|
32 (Double levels) |
>0.05 |
|
|
Symptoms |
20 (Myelopathy) |
|
|
98 (Radiculopathy) |
>0.05 |
|
|
Affected level. |
|
|
|
1. C4-C5 |
34 (22.66%) |
|
|
2. C5-C6 |
88 (58.56%) |
>0.05 |
|
3. C6-C7 |
27 (18%) |
Table 1: Demographic distribution
The average Cobb angle of the C2-C7 region prior to the surgical intervention was 9.2±2.5 degrees. The postoperative radiographs demonstrated a notable increase in this angle (mean 14.2°±3.0, p <0.05), which remained significant during the final follow-up. The obtained result indicates a mean value of 13.9±2.8 degrees with a statistical significance level of p<0.05.
Upon evaluating Odom's criteria across all cases, it was found that a significant proportion of patients (74%) achieved excellent outcomes, while a smaller percentage of patients (19.33%) achieved good outcomes and a minority (6.67%) achieved fair outcomes.(Figure 1) Out of the 11 instances of notable subsidence, merely 2 cases (18.18%) resulted in favourable outcomes, while the remaining 9 cases (81.81%) yielded excellent outcomes. Following the surgical procedure, there was a notable decrease in axial neck discomfort, as evidenced by the Visual Analogue Scale (VAS neck), which yielded an average score of 2.1±1.10 and a p-value of less than 0.05. In addition, the ultimate evaluation demonstrated a sustained enhancement in axial neck discomfort, as evidenced by a mean VAS neck score of 1.8±1.07 and a statistically significant p-value of less than 0.05. The results of the study demonstrate a significant improvement in radiculopathy symptoms, as assessed by the VAS arm, subsequent to the surgical intervention. The mean VAS arm was 1.7±1.20, and the p-value was <0.05. Furthermore, a subsequent enhancement in the overall condition was noted during the ultimate follow-up, as evidenced by a mean VAS arm score of 1.2±1.11 and a statistically significant p-value of less than 0.05.(Table 2)
|
Variables |
Pre-Op |
Post-Op |
Final follow up |
P-value (Pre-Op VS Post-Op) |
P value (Post Op vs Final Follow Up) |
|
VAS Neck |
7.1±1.76 |
2.1±1.10 |
1.8±1.07 |
<0.05 |
<0.05 |
|
VAS Arm |
7.5±1.65 |
1.7±1.20 |
1.2±1.11 |
<0.05 |
<0.05 |
|
mJOA |
11.2±1.45 |
14.1±1.22 |
15.2±1.26 |
>0.05 |
<0.05 |
|
C2-C7 Cob |
9.2±2.5 |
14.2±3.0 |
13.9±2.8 |
<0.02 |
<0.02 |
Table 2: Comparison of VAS for Neck, VAS for Arm, mJOA and Cobbs angle at pre-op, post-op and final follow up
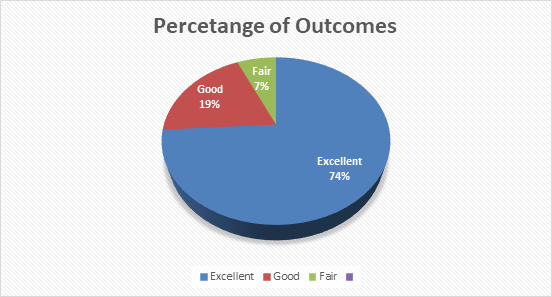
Figure 1: Odoms criteria outcome percentages
The findings demonstrate that there was an enhancement in the modified Japanese Orthopaedic Association (mJOA) score among all individuals diagnosed with myelopathy (mean 14.1±1.22, p<0.05) in contrast to their preoperative score of 11.2±1.45. The final evaluation resulted in an average mJOA score of 15.2±1.26, which was found to be statistically significant with a p-value of <0.05.(Table 2)
The subsidence group had a loss of IBH from (26.91 ± 0.54) to (26.12 ± 0.31) at the final follow up while the non-subsidence group had a loss from (27.32 ± 0.85) to (27.74 ± 0.57). (p-value<0.05) Also there was a statistically significant increase in the segmental kyphosis angle in the subsidence group (3.8 ± 4.8) in comparison to the other group(0.8 ± 5.2)
|
Subsidence Group |
Non-Subsidence Group |
P-value |
|
|
Number of patients |
11 (out of 118) |
107 (out of 118) |
- |
|
Gender |
- |
||
|
Male |
8 |
68 |
|
|
Female |
3 |
41 |
|
|
Age (In years) |
58.4 ± 8.48 |
54.3 ± 9.65 |
0.62 |
|
(31-70) |
(24-65) |
||
|
Kyphosis Segmental Angle |
|||
|
Pre-op |
0.95 ± 4.55 |
0.69 ± 3.94 |
0.97 |
|
Post-op |
-0.7 ± 5.8 |
-0.3 ± 4.6 |
0.54 |
|
Final Follow Up |
3.8 ± 4.8 |
0.8 ± 5.2 |
0.02 |
|
C2-C7 Cervical Angle |
|||
|
Pre-op |
-11.1 ± 9.4 |
-12.4 ± 6.7 |
0.72 |
|
Post-op |
-11.9 ± 10.2 |
-13.8 ± 4.5 |
0.91 |
|
Final Follow Up |
-10.8 ± 11.5 |
-13.6 ± 10.2 |
0.84 |
|
Interbody height |
|||
|
Pre-op |
26.91 ± 0.54 |
27.32 ± 0.85 |
0.12 |
|
Post op |
29.82 ± 0.62 |
29.81 ± 0.70 |
0.98 |
|
Final Follow up |
26.12 ± 0.31 |
27.74 ± 0.57 |
0.01 |
Table 3: Comparison of Segmental kyphosis angle, Cobbs angle and Interbody height in both groups
After a period of three months, the fusion rate was found to be 92%, with 138 out of 150 levels successfully fused. Successful fusion was observed in all cases except 4 cases that had asymptomatic pseudoarthrosis at follow-up assessment. Eleven instances of subsidence were observed, representing 9.32% of the total 118 cases (p-value >0.05). This consisted of eight instances of single-level fusion and three instances of two-level fusion. Of the single level anterior cervical discectomy and fusion (ACDF) procedures performed, 5 out of 8 resulted in subsidence greater than 4 millimetres and were accompanied by segmental kyphosis. In contrast, only 1 out of 3 double level ACDF procedures resulted in subsidence greater than 4 millimetres. The remaining five cases exhibited a maximum subsidence of 3 mm and presented with segmental kyphosis. The subsidence did not exceed 5 mm in any instance.
Discussion
The fundamental objective of an anterior cervical discectomy and fusion (ACDF) procedure remains consistent, which is to alleviate the compression on neural structures and establish stability to the operated segment. Over the course of time, it is imperative to consider addressing cervical alignment, kyphosis, and subsidence. Despite the high fusion rates observed in conventional bone grafting techniques, the significant probability of donor site morbidity has prompted surgeons to shift away from such procedures. The utilisation of interbody devices, aided by screws and plates for fusion, as well as stand-alone cages, has gained popularity due to its efficacy in maintaining interbody height and preventing root compression caused by foraminal narrowing. The utilisation of stand-alone cages has become increasingly prevalent due to their ability to mitigate various complications associated with plate assisted fusion or screw insertion, including screw back out, irritation of the oesophagus, and dysphagia[9,10].
The primary issue under investigation in our study pertains to the frequently observed complications associated with stand-alone cages, namely subsidence and non-union. The investigation revealed that there were 11 instances of subsidence exceeding 3mm during the final follow-up, accounting for approximately 9.32% of the total patient population. (Fig 2) None of the patients who experienced subsidence exhibited a noteworthy decrease in functional activity. Among the cohort of 11 patients who experienced subsidence, 9 individuals exhibited a favourable recuperation as determined by Odom's criteria, while the remaining 2 patients demonstrated satisfactory outcomes.
A study published in 2022 shows a subsidence of 21% out of 144 total disc spaces operated[16]. The average occurrence rate of subsidence was 21.1%, with a range of reported rates from 0% [17,18,19,20] to a single study reporting a rate of 83% [21] in their study of stand-alone PEEK cages with autografting showed an incidence of 22.6% of subsidence but in corelation with Odom’s criteria, all the patients with Radiological subsidence had good clinical and functional outcomes. On the contrary another study performed by Chiang et al showed that the patients with subsidence had a lower satisfaction rate at final follow up[22].
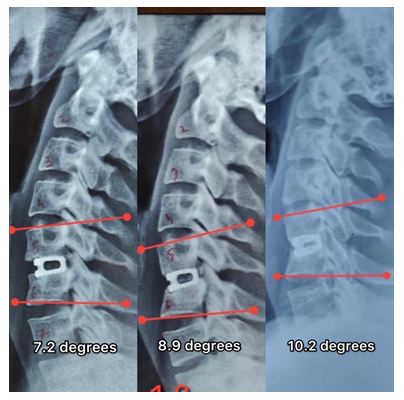
Figure 2: Case with series of xrays at Post operative, 6 months and 2 year follow up showing mild segmental kyphosis and subsidence
Our study yielded a fusion rate of 96.6% at final follow up. Four instances of pseudoarthrosis were observed. In another study, Wang and colleagues documented a pseudoarthrosis rate of approximately 5.4% for single-level fusions and 7.1% for two-level fusions[26]. The study conducted by Fraser and colleagues reported a statistically significant increase in the fusion rate for both single level and multilevel anterior cervical discectomy and fusion procedures when an additional anterior plate was utilized[27]. The fusion rates observed in our study are comparable to those reported in the majority of studies that employ a plate device for fusion attainment. The results indicate that there was a statistically significant improvement in VAS Neck and VAS Arm both after the surgical procedure and at the final follow-up (p<0.05). The improvement in mJOA score was statistically significant (p<0.05) after a mean follow-up period of 5.3 years.
The present study involved the selection of cage size based on the surgeon's experience with the necessary distraction force or alignment, utilising a trial-and-error approach. Nonetheless, there exists a lack of objective criteria for ascertaining the appropriate dimensions of a cage or for prognosticating the clinical result. Several factors have been linked to a heightened risk of subsidence, including suboptimal surgical technique, such as excessive distraction, and the use of an incorrect cage size[23]. Research findings indicate that the elimination of the endplate results in early consolidation, whereas a fusion rate of 80% can be attained within a period of 6 months without the removal of the endplate[24]. Bartels et al also gave an insight about higher rates of subsidence seen at C5-C6 levels due to higher stress at this level[11]. Following anterior cervical discectomy and fusion (ACDF) using only a cage, the average disc height experiences an initial increase, as reported in several studies[23,25]. However, it is observed that the disc height subsequently decreases and may either remain above the preoperative value or fall below it[23,25]. The findings of our investigation revealed a mean elevation in intervertebral space immediately after the surgical procedure, followed by a subsequent reduction in intervertebral height at the final follow-up assessment.
The study's constraints encompass its retrospective. Furthermore, the present study did not incorporate osteoporosis as a potential risk factor that could impact cage subsidence. Also, the precision of linear measurements on a picture archiving and communication system (PACS) is deemed satisfactory for computed tomography (CT) scans, but it is deemed insufficient for digital plain radiographs unless an internal calibration is employed. Despite the limitations, the considerable volume of cases performed by a solitary surgeon utilising a consistent technique that yields favourable functional results in instances of subsidence has significant implications for research on anterior cervical discectomy and fusion (ACDF) procedures. However, it is imperative to investigate variable intraoperative factors such as end plate preparation and excision of the posterior longitudinal ligament (PLL).
Conclusion
Subsidence is a common occurrence in ACDF (anterior cervical discectomy and fusion) surgeries that utilise stand-alone cages. Most of the academic literature documents this discovery. According to our study, the subsidence observed did not have a significant clinical impact on outcome scores or patient satisfaction. The utilisation of a stand-alone cage devoid of screw or plate instrumentation has demonstrated favourable long-term outcomes with nearly complete fusion rates.
Source(s) of support:
None
Conflicting Interest (If present, give more details):
None
References
- Mummaneni PV, Kaiser MG, Matz PG, et al. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine 11 (2009): 130-141.
- Wang JC, McDonough PW, Endow KK, et al. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 25 (2000): 41-45.
- Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40 (1958): 607-624.
- Nambiar M, Phan K, Cunningham JE, et al. Locking stand-alone cages versus anterior plate constructs in single-level fusion for degenerative cervical disease: a systematic review and meta-analysis. European Spine Journal 9 (2017): 2258-2266.
- Banwart JC, Asher MA, Hassanein RS. Iliac crest bone graft harvest donor site morbidity: a statistical evaluation. Spine 20 (1995): 1055-1060.
- Siddiqui AA, Jackowski A. Cage versus tricortical graft for cervical interbody fusion. A prospective randomised study. J Bone Joint Surg Br 85 (2003): 1019-1025
- Bertalanffy H, Eggert HR. Clinical long-term results of anterior discectomy without fusion for treatment of cervical radiculopathy and myelopathy. A follow-up of 164 cases. Acta Neurochir 90 (1998): 127-135.
- Wang JC, McDonough PW, Endow KK, et al. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine 26 (2001): 643-647.
- Eleraky M, Lianos C, Sonntag VKH. Cervical corpectomy: report of 185 cases and review of literature. J Neurosurg (Spine 1) 90 (1999): 35-41.
- Hanc? M, Toprak M, Sar?oglu AC. Esophageal perforation subsequent to anterior cervical spine screw/plate fixation. Paraplegia 33 (1995): 606–609.
- Bartels RH, Donk RD, Feuth T : Subsidence of stand-alone cervical car¬bon fiber cages. Neurosurgery 58 (2006): 502-508.
- Ha SK, Park JY, Kim SH, et al. Radiologic assess¬ment of subsidence in stand-alone cervical polyetheretherketone (PEEK) cage. J Korean Neurosurg Soc 44 (2008): 370-374.
- Shad A, Leach JC, Teddy PJ, et al. Use of the Solis cage and local autologous bone graft for anterior cervical discectomy and fu¬sion : early technical experience. J Neurosurg Spine 2 (2005): 116-122.
- Yang JJ, Yu CH, Chang BS, et al: Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg 3 (2011): 16-23.
- Lee CH, Hyun SJ, Kim MJ, et al. Compar¬ative analysis of 3 different construct systems for single-level anterior cervical discectomy and fusion : stand-alone cage, iliac graft plus plate augmentation, and cage plus plating. J Spinal Disord Tech 26 (2013): 112-118.
- Godlewski B, Bebenek A, Dominiak M, et al. Subsidence following cervical discectomy and implant-to-bone ratio. BMC Musculoskelet Disord 23 (2022): 750.
- Akula M, Taha M, Mathew B, et al. The plate cage Benezech implant as an alternative to autologous bone graft in the treatment of cervical spondylosis: clinical and functional outcome. Br J Neurosurg 22 (2008): 542-545.
- Ba Z, Zhao W, Wu D, et al. Box cages packed with local decompression bone were efficient in anterior cervical discectomy and fusion: five- to 10-year follow-up. Spine 37 (2012): E1260-E1263.
- Dufour T, Huppert J, Louis C, et al. Radiological analysis of 37 segments in cervical spine implanted with a peek stand-alone device, with at least one year follow-up. Br J Neurosurg 24 (2010): 633–640.
- Elsawaf A, Mastronardi L, Roperto R, et al. Effect of cervical dynamics on adjacent segment degeneration after anterior cervical fusion with cages. Neurosurg Rev 32 (2009): 215-224.
- Park JI, Cho DC, Kim KT, et al. Anterior cervical discectomy and fusion using a stand-alone polyetheretherketone cage packed with local autobone : assessment of bone fusion and subsidence. J Korean Neurosurg Soc 54 (2013): 189-193.
- Chiang CJ, Kuo YJ, Chiang YF, et al. Anterior cervical fusion using a polyetheretherketone cage containing a bovine xenograftp: three to five-year follow-up. Spine 33 (2008): 2524-2428.
- Kulkarni AG, Hee HT, Wong HK. Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J 7 (2007): 205-209.
- Porto Filho MR, Pastorello MT, Defino HL. Experimental study of the participation of the vertebral endplate in the integration of bone grafts. Eur Spine J 14 (2005): 965-970.
- Kast E, Derakhshani S, Bothmann M, et al. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev 32 (2009): 207-214.
- Wang M, Chou D, Chang C, et al. Anterior cervical discectomy and fusion performed using structural allograft or polyetheretherketone: pseudarthrosis and revision surgery rates with minimum 2-year follow-up, Journal of Neurosurgery: Spine SPI 32 (2020): 562-569.
- Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: A metaanalysis of fusion rates. J Neurosurg Spine 6 (2007): 298-303.
