An Innocuous Solitary Neck Node: Case Report of an Occult Papillary Thyroid Microcarcinoma Presenting with Nodal Metastasis
Article Information
Jiayi Weng1*, KonVoi Tay2, Thomas WaiThong Ho3, MeiYi Low4
1Yong Loo Lin School of Medicine, National University of Singapore, Singapore
2Consultant, General Surgery Department, Woodlands Health Campus, Singapore
3Senior Consultant, Mount Alvernia Hospital, Singapore
4Consultant, Otolaryngology Department, KK Women’s and Children’s Hospital, Singapore
*Corresponding Author: Jiayi Weng, Yong Loo Lin School of Medicine, National University of Singapore, 10 Medical Dr, 117597, Singapore
Received: 07 October 2021; Accepted: 21 October 2021; Published: 01 November 2021
Citation: Jiayi Weng, KonVoi Tay, Thomas WaiThong Ho, MeiYi Low. An Innocuous Solitary Neck Node: Case Report of an Occult Papillary Thyroid Microcarcinoma Presenting with Nodal Metastasis. Archives of Clinical and Medical Case Reports 5 (2021): 771-777.
View / Download Pdf Share at FacebookAbstract
Background: Occult primary head and neck cancer constitutes 5-10% of all patients with carcinoma of unknown primary and presents as both a diagnostic challenge and management dilemma to clinicians. We present one case of papillary thyroid microcarcinoma where the only presenting sign was a painless enlarged cervical lymph node, with no evidence of the primary site of malignancy after initial evaluations.
Case Presentation: A sixty-five-year-old female patient presented with a two-month history of painless swelling on the left side of the neck with no change in size. Ultrasonography detected a left level V lymph node and a left level IV lymph node with suspicious features for malignancy but did not detect any thyroid nodules. Excision biopsy of the lymph node and bilateral tonsillectomy revealed a diagnosis of metastatic papillary carcinoma with a primary from the thyroid. A repeat focused ultrasonography of the thyroid revealed two nodules. Total thyroidectomy and selective left neck dissection (levels IIVI) were performed. The final diagnosis was multifocal papillary thyroid carcinoma with metastasis to seven out of twenty-four lymph nodes excised. The TMN stage was pT1aN1bM0. The patient was discharged on postoperative day three uneventfully. Adjuvant radioactive iodine was planned for the patient at a dose of 100 mCi at one month postoperatively.
Conclusion: Occult primary PTMC presenting as isolated cervical lymphadenopathy and diagnosed only on histology is a rare entity. When initial clinical and radiological evaluations reveal no thyroid abnormalities, FNAC and excision of lymph nodes are useful steps in establishing the diagnosis and primary site of the tumour. Total thyroidectomy with a therapeutic neck dissection is the appropriate next step in treatment for these patients. With postoperative radioactive
Keywords
Occult papillary thyroid microcarcinoma; Solitary neck node
Occult papillary thyroid microcarcinoma articles; Solitary neck node articles
Occult papillary thyroid microcarcinoma articles Occult papillary thyroid microcarcinoma Research articles Occult papillary thyroid microcarcinoma review articles Occult papillary thyroid microcarcinoma PubMed articles Occult papillary thyroid microcarcinoma PubMed Central articles Occult papillary thyroid microcarcinoma 2023 articles Occult papillary thyroid microcarcinoma 2024 articles Occult papillary thyroid microcarcinoma Scopus articles Occult papillary thyroid microcarcinoma impact factor journals Occult papillary thyroid microcarcinoma Scopus journals Occult papillary thyroid microcarcinoma PubMed journals Occult papillary thyroid microcarcinoma medical journals Occult papillary thyroid microcarcinoma free journals Occult papillary thyroid microcarcinoma best journals Occult papillary thyroid microcarcinoma top journals Occult papillary thyroid microcarcinoma free medical journals Occult papillary thyroid microcarcinoma famous journals Occult papillary thyroid microcarcinoma Google Scholar indexed journals microcarcinoma articles microcarcinoma Research articles microcarcinoma review articles microcarcinoma PubMed articles microcarcinoma PubMed Central articles microcarcinoma 2023 articles microcarcinoma 2024 articles microcarcinoma Scopus articles microcarcinoma impact factor journals microcarcinoma Scopus journals microcarcinoma PubMed journals microcarcinoma medical journals microcarcinoma free journals microcarcinoma best journals microcarcinoma top journals microcarcinoma free medical journals microcarcinoma famous journals microcarcinoma Google Scholar indexed journals Solitary neck node articles Solitary neck node Research articles Solitary neck node review articles Solitary neck node PubMed articles Solitary neck node PubMed Central articles Solitary neck node 2023 articles Solitary neck node 2024 articles Solitary neck node Scopus articles Solitary neck node impact factor journals Solitary neck node Scopus journals Solitary neck node PubMed journals Solitary neck node medical journals Solitary neck node free journals Solitary neck node best journals Solitary neck node top journals Solitary neck node free medical journals Solitary neck node famous journals Solitary neck node Google Scholar indexed journals lymph node articles lymph node Research articles lymph node review articles lymph node PubMed articles lymph node PubMed Central articles lymph node 2023 articles lymph node 2024 articles lymph node Scopus articles lymph node impact factor journals lymph node Scopus journals lymph node PubMed journals lymph node medical journals lymph node free journals lymph node best journals lymph node top journals lymph node free medical journals lymph node famous journals lymph node Google Scholar indexed journals PTMC articles PTMC Research articles PTMC review articles PTMC PubMed articles PTMC PubMed Central articles PTMC 2023 articles PTMC 2024 articles PTMC Scopus articles PTMC impact factor journals PTMC Scopus journals PTMC PubMed journals PTMC medical journals PTMC free journals PTMC best journals PTMC top journals PTMC free medical journals PTMC famous journals PTMC Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals lymphadenopathy articles lymphadenopathy Research articles lymphadenopathy review articles lymphadenopathy PubMed articles lymphadenopathy PubMed Central articles lymphadenopathy 2023 articles lymphadenopathy 2024 articles lymphadenopathy Scopus articles lymphadenopathy impact factor journals lymphadenopathy Scopus journals lymphadenopathy PubMed journals lymphadenopathy medical journals lymphadenopathy free journals lymphadenopathy best journals lymphadenopathy top journals lymphadenopathy free medical journals lymphadenopathy famous journals lymphadenopathy Google Scholar indexed journals Radioembolization articles Radioembolization Research articles Radioembolization review articles Radioembolization PubMed articles Radioembolization PubMed Central articles Radioembolization 2023 articles Radioembolization 2024 articles Radioembolization Scopus articles Radioembolization impact factor journals Radioembolization Scopus journals Radioembolization PubMed journals Radioembolization medical journals Radioembolization free journals Radioembolization best journals Radioembolization top journals Radioembolization free medical journals Radioembolization famous journals Radioembolization Google Scholar indexed journals Case Report articles Case Report Research articles Case Report review articles Case Report PubMed articles Case Report PubMed Central articles Case Report 2023 articles Case Report 2024 articles Case Report Scopus articles Case Report impact factor journals Case Report Scopus journals Case Report PubMed journals Case Report medical journals Case Report free journals Case Report best journals Case Report top journals Case Report free medical journals Case Report famous journals Case Report Google Scholar indexed journals
Article Details
Abbreviations:
MRI- Magnetic resonance imaging; PET- Positron emission tomography; FNAC- Fine needle aspiration cytology; SCC- squamous cell carcinoma; CT- computed tomography; U/S- ultrasound; PTC- Papillary thyroid carcinoma; PTMC- Papillary thyroid microcarcinoma.
1. Background
Occult primary head and neck cancer refers to metastatic carcinoma in a cervical lymph node without an identifiable primary site after appropriate investigations. This constitutes 5-10% of all patients with carcinoma of unknown primary and presents as both a diagnostic challenge and management dilemma to clinicians [1]. We present one case of papillary thyroid microcarcinoma where the only presenting sign was a painless enlarged cervical lymph node, with no evidence of the primary site of malignancy after initial evaluation. Metastatic papillary microcarcinoma with thyroid origin was only confirmed after total thyroidectomy with ipsilateral cervical node clearance.
2. Case Presentation
A sixty-five-year-old female patient presented with a two-month history of painless swelling on the left side of the neck with no change in size. A non-tender, mobile lymph node measuring approximately 1.5cm was noted at the left posterior cervical region. There were no apparent inflammatory or infectious causes, and constitutional symptoms. Ultrasonography detected a left level V lymph node measuring 12.6mm and a left level IV lymph node measuring 11.5mm with suspicious features for malignancy (Figure 1). The thyroid gland was normal in size with no suspicious nodule on ultrasound. Flexible nasendoscopy showed no abnormal findings. Magnetic resonance imaging (MRI) of the neck detected a bulky left tonsil in addition to the two abnormal lymph nodes. A positron emission tomography (PET) scan reported uptake only in the two cervical nodes. Fine needle aspiration cytology (FNAC) of the larger node revealed atypical cells suspicious for squamous cell carcinoma (SCC).
Excision of the left level V lymph node and bilateral tonsillectomy was performed to obtain tissue samples for histological diagnosis. Macroscopically, a lymph node measuring 1.5cm in maximum dimension with an area of cystic degeneration measuring up to 0.7cm was detected. Histologically, the lymph node showed a cystic nodule with complex papillary branching fronds and a fine vascular core, covered by a single layer of cells with ovoid crowded to overlapping nuclei. There were occasional nuclear pseudo inclusions and nuclear grooves. The tumour measured 10mm in maximum length without extranodal extension and stained with PAX8 and with TT. The lymph node was diagnosed as metastatic papillary carcinoma with a primary from the thyroid. Microscopic examination of the tonsillar specimens revealed reactive lymphoid hyperplasia with no malignancy.
A repeat focused ultrasonography of the thyroid revealed two non-suspicious nodules, one in the right lobe middle pole measuring 5.4mm, and one in the right lobe lower pole measuring 12.0mm. There were no overt nodules in the left lobe and no lymphadenopathy on the right side. Total thyroidectomy and selective left neck dissection (levels II-VI) were performed. Macroscopic examination of the right thyroid lobe shows a whitish ill-defined 3 x 3 mm nodule in the mid pole and a 1cm hemorrhagic nodule in the left lobe. Microscopically, multifocal papillary thyroid carcinoma was detected with one 3 mm foci in the right lobe and another 3 mm foci in the left lobe. In addition, several foci measuring less than 1 mm were also seen scattered in the right lobe. All foci were consistent with a classical variant with no vascular invasion and minimal extrathyroidal extension. A hyperplastic nodule measuring 11mm was also present in the left lobe. Twenty-four lymph nodes were obtained from the left neck dissection. Seven of twenty-four lymph nodes were metastatic, with no extranodal extension seen. The TMN stage was determined to be pT1aN1bM0. The patient was discharged on postoperative day three uneventfully. Adjuvant radioactive iodine was planned at a dose of 100 mCi at one month postoperatively. The patient will be placed on thyroxine suppression therapy subsequently.
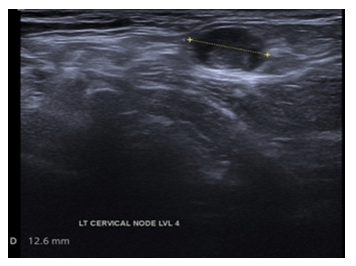
Figure 1: Left level 5 lymph node suspicious of malignancy.
3. Discussion
Although the lymphatic drainage of the head and neck region is well studied, localizing occult primaries in this region remains a diagnostic challenge. Failure to identify a primary tumour site complicates subsequent investigation and management and is associated with significant morbidity [1]. Metastases to lymph nodes in the upper and middle neck (levels I, II, III and V) generally originate from head and neck cancers, while the involvement of lymph nodes in the lower neck (level IV) suggests a primary site below the clavicles [2].
Fine needle aspiration biopsy of cervical lymph nodes and subsequent staining helps determine the tumour’s histological subtype and hence play a pivotal role in localizing the primary site. Approximately 90% [3] of these occult primaries are squamous cell carcinoma (SCC), with the remainder being adenocarcinoma, melanoma, and other rare histologic variants. SCC most likely originates from head and neck mucosa, thus necessitating a thorough evaluation with panendoscopy and blind biopsies from potential primary sites, including Waldeyer ring. Bilateral tonsillectomy [4] is often advocated as 25% of occult primary tumours can be attributed to the tonsils. Other diagnostic modalities in detecting occult primary with cervical lymph metastases include computed tomography (CT), MRI, PET and PET-CT fusion scan. PET is useful in locating the primary tumour in one-quarter of all patients [5]. Walton et al. showed that a whole-body PET scan can achieve a success rate of 14.6% in detecting primary tumours, while a PET-CT fusion study increases this rate to 44.2%. However, the highest yield in identifying primary tumour sites (59.6%) was achieved using a combination of PET-CT and panendoscopy with directed biopsies.
Focused ultrasound (U/S) examination of the thyroid is another important diagnostic tool in localizing potential primary sites. The incidence of thyroid cancer has been increasing on the background of declining incidence of most head and neck cancers, possibly due to the increased diagnosis of small papillary carcinomas [4, 6-8]. Reasons for thyroid malignancy presenting as occult primary tumours include small tumour size, tumour regression and ectopic thyroid tissue, with papillary thyroid carcinoma (PTC) comprising the majority of thyroid carcinoma arising in ectopic sites such as the thyroglossal duct cyst [9]. The presence of BRAF V600E mutation is associated with a higher incidence (80%) of cervical lymph node metastasis in PTMC [10]. This suggests that staining for BRAF V600E after lymph node biopsy may help locate the thyroid’s primary tumour site.
PTC is the most common well-differentiated thyroid carcinoma and is known to metastasize via the lymphatic system to regional lymph nodes [11]. Cancers smaller than 1cm are termed papillary thyroid microcarcinoma (PTMC) [12]. Given the small size, PTMC cannot be felt clinically, is difficult to detect radiologically and generally remains latent [13-16]. Cervical lymphadenopathy was the sole presenting sign in 4.39% and 7.78% [17] of PTCs and PTMCs respectively. In another large series, Wada et al reported a 9.3% of PTMC presenting solely with palpable lymphadenopathy [18]. It is noteworthy that our patient had a similar presentation to the 13 cases described by Garrel et al [17] in that the PTMC was neither clinically nor radiologically apparent but diagnosed only on histology. Such a presentation by PTMC is exceedingly rare.
Clinical management for papillary thyroid microcarcinoma should be personalised based on risk stratification [19]. The standard treatment for PTMC with nodal metastasis includes total thyroidectomy, central compartment and lymph node clearance, as well as subsequent radioiodine ablation and TSH suppression thyroid replacement therapy [20, 21]. While most PTMC bear an excellent prognosis with greater than 90% disease-free survival after long term follow- up, those with high-risk characteristics have a higher recurrence rate and poorer prognosis [22]. High-risk characteristics include multifocality, bilateral lesions, extrathyroidal extension, vascular invasion, lymph node metastases, extranodal extension and distant metastases [23]. These high-risk characteristics, if present, influence the extent of surgery required for treatment [24] and warrant more radical treatments. Wada et al analysed the benefits of a prophylactic versus therapeutic neck dissection in their series of PTMC cases. Their findings suggest that cancers from non-palpable lymph nodes remain indolent and rarely become clinically significant [18]. Thus, they did not recommend a prophylactic node dissection as was our treatment for the contralateral neck in our patient.
4. Conclusion
Occult primary PTMC presenting as isolated cervical lymphadenopathy is a rare entity. When initial clinical and radiological evaluations reveal no thyroid abnormalities, FNAC and excision of lymph nodes are useful steps in establishing the diagnosis and primary site of the tumour. Total thyroidectomy with a therapeutic neck dissection is the appropriate next step in treatment for these patients. With postoperative radioactive iodine ablation and life-long suppressive thyroxine, the outcome is usually favourable.
Ethics Approval and Consent to Participate
NA
Consent for Publication
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Availability of Data and Materials
NA
Competing Interests
NA
Funding
NA
Authors' Contributions
JW did literature search and manuscript draft. KT assisted with literature search and critique. TWH and ML interpreted the patient's data and assisted with manuscript critique. All authors read and approved the manuscript before submission.
Acknowledgements
NA
References
- Calabrese L, Jereczek-Fossa BA, Jassem J, et al. Diagnosis and management of neck metastases from an unknown primary. Acta Otorhinolaryngol Ital 25 (2005): 2-12.
- López F, Rodrigo JP, Silver CE, et al. Cervical lymph node metastases from remote primary tumor sites. Head Neck 38 Suppl 1 (2016): E2374-E2385.
- Jereczek-Fossa, Barbara A, et al. Cervical lymph node metastases of squamous cell carcinoma from an unknown primary. Cancer Treatment Reviews 30 (2004): 153-164.
- Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA 295 (2006): 2164-2167.
- Waltonen JD, Ozer E, Hall NC, et al. Metastatic Carcinoma of the Neck of Unknown Primary Origin: Evolution and Efficacy of the Modern Workup. Arch Otolaryngol Head Neck Surg 135 (2009): 1024-1029.
- Davies L, Welch HG. Epidemiology of head and neck cancer in the United States. Otolaryngol Head Neck Surg 135 (2006): 451-457.
- Hughes DT, Haymart MR, Miller BS, et al. The most commonly occurring papillary thyroid cancer in the United States is now a microcarcinoma in a patient older than 45 years. Thyroid 3 (2011): 231-236.
- Pacini F. Thyroid microcarcinoma. Best Pract Res Clin Endocrinol Metab 26 (2012): 421-429.
- Ibrahim NB, Milewski PJ, Gillett R, et al. Benign thyroid inclusions within cervical lymph nodes: an alarming incidental finding. Aust N Z J Surg 51 (1981): 188-189.
- Virk RK, Van Dyke AL, Finkelstein A, et al. BRAFV600E mutation in papillary thyroid microcarcinoma: a genotype-phenotype correlation. Mod Pathol 26 (2013): 62-70.
- Smith VA, Sessions RB, Lentsch EJ. Cervical lymph node metastasis and papillary thyroid carcinoma: does the compartment involved affect survival? Experience from the SEER database. J Surg Oncol 106 (2012): 357-362.
- Bradley NL, Wiseman SM. Papillary thyroid microcarcinoma: the significance of high risk features. BMC Cancer. 17 (2017): 142.
- Singh A, But R, Lopez R. Metastatic papillary thyroid carcinoma with the absence of tumour focus in the thyroid gland. Am J Case Rep 14 (2013): 73-75.
- Boucek J, Kastner J, Skrivan J, et al. Occult thyroid carcinoma. Acta Otorhinolaryngol Ital 29 (2009): 296-304.
- Bomeli SR, LeBeau SO, Ferris RL. Evaluation of a thyroid nodule. Otolaryngol Clin North Am 43 (2010): 229-vii.
- Pakdaman MN, Rochon L, Gologan O, et al. Incidence and histopathological behavior of papillary microcarcinomas: study of 429 cases. Otolaryngol Head Neck Surg 139 (2008): 718-722.
- Garrel R, Tripodi C, Cartier C, et al. Cervical lymphadenopathies signaling thyroid microcarcinoma. Case study and review of the literature. Eur Ann Otorhinolaryngol Head Neck Dis 128 (2011): 115-119.
- Wada N, Duh QY, Sugino K, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237 (2003): 399-407.
- Gao R, Jia X, Liang Y, et al. Papillary Thyroid Micro Carcinoma: The Incidence of High-Risk Features and Its Prognostic Implications. Front Endocrinol (Lausanne) 10 (2019): 74.
- Murthy SP, Balasubramanian D, Subramaniam N, et al. Prevalence of adverse pathological features in 1 to 4 cm low-risk differentiated thyroid carcinoma. Head Neck 40 (2018): 1214-1218.
- Kluijfhout WP, Pasternak JD, Lim J, et al. Frequency of high-risk characteristics requiring total thyroidectomy for 1–4 cm well-differentiated thyroid cancer. Thyroid 26 (2016): 820-824.
- Liu FH, Kuo SF, Hsueh C, et al. Postoperative recurrence of papillary thyroid carcinoma with lymph node metastasis. J Surg Oncol 112 (2015): 149-154.
- Cheng F, Chen Y, Zhu L, et al. Risk Factors for Cervical Lymph Node Metastasis of Papillary Thyroid Microcarcinoma: A Single-Center Retrospective Study. Int J Endocrinol (2019): 8579828.
- Haugen E, Alexander E, Bible K, et al. American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26 (2015): 1-133.
