After Years of Medical Wandering, A Diagnosis of Chronic Babesiosis Saves A Patient
Article Information
Alexis LACOUT*, 1, Ahed ZEDAN2, Christian PERRONNE3
1Diagnostic Center, ELSAN, Medical-Surgical Center, 83 avenue Charles de Gaulle, Aurillac, France
2Competence Center for Tick-Vectored Diseases (CCMVT), Saint Côme Polyclinic, Compiègne, France
3Infectious and tropical diseases, Paris, France
*Corresponding author: Alexis LACOUT, Diagnostic Center, ELSAN, Medical-Surgical Center, 83 avenue Charles de Gaulle, Aurillac, France
Received: 15 September 2023 Accepted: 29 September 2023 Published: 01 November 2023
Citation: Alexis LACOUT, Ahed ZEDAN, Christian PERRONNE. After Years of Medical Wandering, A Diagnosis of Chronic Babesiosis Saves A Patient. Archives of Microbiology and Immunology. 7 (2023): 246-249.
View / Download Pdf Share at FacebookAbstract
This is the case of a 36-year-old immunocompetent, non-splenectomized female patient presenting with a "polymorphic persistent syndrome after a possible tick bite" (SPPT), a syndrome officially recognized by the French High Authority for health (HAS). The patient’s syndrome combined major asthenia, neurological and cognitive disorders (concentration and memory difficulties) and polymorphic somatic signs (muscular, joint and neurological pain, night sweats, chills, etc.) which had been evolving for several years. Babesia serology and PCR were positive. After an initial exacerbation of symptoms, a combined treatment was spectacularly effective. The patient has now been in complete remission for several years
Keywords
High Authority for health (HAS), SPPT, Blood smears, PCR
Article Details
1. History of the disease
This 36-year-old patient, a self-employed nurse in a rural area of Auvergne and a former top-level cycling athlete, had been suffering from unexplained polymorphic symptoms for many years, associated with incapacitating asthenia.
In 2005, she left on a one-month humanitarian mission to Maripassoula in the Amazon rainforest, on the border between French Guiana and Surinam. As soon as she arrived, she suffered from numerous leg bites which did not heal during the entire stay, due to the very precarious hygiene conditions. Three days after returning to France, she developed a high fever with chills. Eight days later, she was diagnosed with impetiginized insect bites with Staphylococcus aureus, which was treated with roxithromycin and local care with an antiseptic and fusidic acid. In 2012, she presented with a vertiginous syndrome suggestive of vestibular neuritis, treated with 3,000 mg of cortisone over 3 days (multiple sclerosis was suspected). The dizziness subsided, but extreme fatigue, intestinal problems, muscle and joint pain persisted.
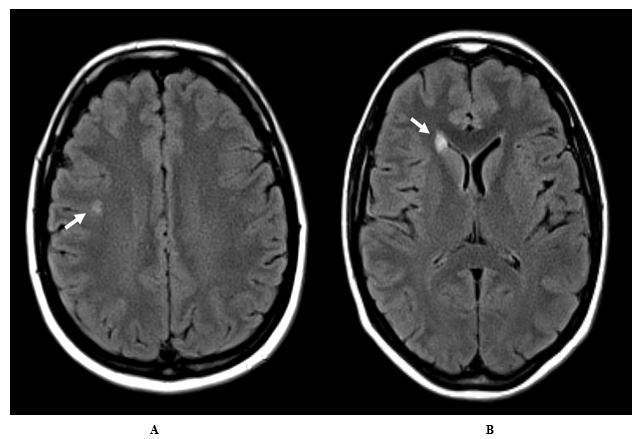
At the end of 2013, a consultation at the nearest university hospital ruled out Whipple's disease. HIV, CMV, EBV, hepatitis B and C, aspergillosis and Campylobacter serologies came back negative, as did Lyme serology (ELISA and Western blot). A test for syphilis was doubtful; however, there was no evidence of lupus. Cerebral MRI revealed a few non-specific FLAIR hyperintensities (Figure 1) in the white matter, which did not suggest leukoaraiosis-type vascular damage in this young patient. The clinical neurological examination was normal. A suspicion of multiple sclerosis was finally ruled out. A chronic fatigue syndrome was diagnosed.
Subsequently, despite negative serology, an empiric antibiotic treatment was carried out in the context of a possible Lyme disease, using doxycycline combined with chloroquine with a good response. The good response to treatment with chloroquine subsequently prompted a rheumatology consultation, which ruled out rheumatic and autoimmune pathologies. Since then, there have been alternating episodes of intense asthenia accompanied by muscular pain and intestinal problems. Recurrent vagal malaise appeared, with significant drops in blood pressure and paleness at a distance from physical exertion. The electrocardiogram was normal. The cardiovascular work-up was reassuring: hypotension favoured by physical effort during recovery, of unknown origin. Anti-nuclear antibodies were positive (1/ 640), with a mixed, homogeneous, speckled fluorescence pattern; anti-native DNA and anti extractable nuclear antigen (ENA) antibodies were negative. The pneumological work-up showed a functional restrictive syndrome. Avian, hay and aspergillus precipitins, brucellosis were negative. Lyme disease serologies remained negative. A thoracic abdominal and pelvic CT scan showed no significant abnormalities.
2. Clinical presentation
It was in this context of several years of diagnostic wandering, without a synthesis of the various elements, that she presented herself for a consultation at the end of 2017. On examination, the patient was found to have abnormal, incapacitating asthenia, with no depressive syndrome. The patient was anxious, presented with brain fog, concentration and memory problems, and speech disorders with a lack of words. Sleep was disturbed and unrefreshing, with difficulty falling asleep and waking up at night. Somatically, she complained of cramps, impatient legs and muscular fasciculations. She also complained of chest tightness with dyspnea, palpitations, hyperacusis, photophobia, visual disturbances, neurological pain with paresthesias and burning sensations, and digestive disturbances, especially diarrhea and heartburn. The patient reported abnormal chilliness, chills, cold extremities, profuse night sweats, sometimes febrile. In addition to neurological pain, the patient complained of fluctuating articular, muscular, spinal and sometimes intercostal pain. All these complaints were aggravated by the intake of alcoholic beverages. There were no abnormalities on clinical examination. All in all, the patient's quality of life was severely impaired, as she was dependent on her family and friends, and could not even climb the stairs at home. In the absence of a diagnosis, an infectious disease investigation was undertaken, with a particular focus on tick-borne pathogens, as the patient lived on a farm in an exposed rural environment. A diagnosis of "polymorphic persistent syndrome after a possible tick bite" (“syndrome polymorphe après possible piqûre de tique”, SPPT), a syndrome officially recognized by the French High Authority for health (Haute Autorité de Santé, HAS) was mentioned. This syndrome is rather similar to PTLDS (post-treatment Lyme disease syndrome).
Bartonella, Coxiella, Ehrlichia and Chlamydia pneumoniae serologies were negative. Mycoplasma pneumoniae serology was IgG positive. Babesia serology was strongly positive. PCR were performed for Borrelia (Borrelia burgdorferi s.l., B. miyamotoi, B. hermsii); Bartonella (Bartonella spp., B. quintana, B. henselae); Babesia; Mycoplasma; Candida spp, in blood, urine and saliva. A PCR showed the presence of Babesia divergens in blood (2.7 10E7 /ml; CT of 22.82); Mycoplasma was detected in saliva (225000 / ml; CT of 29.5). The patient never had anemia.
Before learning of the highly suggestive results of babesiosis (positive PCR and serology), in view of the polymorphic symptomatology suggestive of Lyme disease, and of a previous effective treatment (doxycycline and chloroquine), a treatment combining doxycycline (200 mg twice daily) and hydroxychloroquine (200 mg daily) was instituted for one month. Immediately afterwards, a treatment specifically against Babesia was started, combining atovaquone (250 mg) and proguanil (100 mg) (Malarone*), three times a day, and azithromycin, 250 mg once a day; a total of two 8-day courses were carried out. Tinidazole (500 mg once a day for 8 days) was also prescribed for its efficacy on persistent forms of Borrelia (cystic forms and biofilms), although the serology was negative, bearing in mind that there are false negatives to the serological test. Hydroxychloroquine was maintained at a dose of 200 mg daily for the duration of treatment. She also took by herself phytotherapy with Artemisia annua, containing compounds active against Plasmodium and Babesia parasites. The first course of atovaquone and proguanil was marked by an intense reaction with asthenia, very profuse daytime and night-time sweating and severe back pain, lasting a few days. Improvement was rapidly spectacular. By the end of the second treatment, the patient was completely asymptomatic. She returned to nursing within a year. A few months later, a minimal relapse occurred, treated again with two courses of atovaquone (250 mg) and proguanil (100 mg), one of 8 days and one of 15 days, due to the good tolerance of the treatment. Then, for consolidation, she received two courses of artemether (20 mg) and lumefantrine (120 mg) (Riamet *), 4 tablets morning and evening for 3 days.
Control PCRs were performed: Blood PCRs were performed on: Borrelia burgdorferi, B. miyamotoi, B. hermsii; Bartonella spp, B. quintana, B. henselae; Babesia spp; Rickettsia spp; Ehrlichia spp; Anaplasma spp; Coxiella burnetii; Mycoplasma spp, M. pneumoniae; Brucella spp; Francisella tularensis; Candida spp; EBV; CMV; HHV-3; Theileria spp; Candidatus neoehrlichia; Chlamydia spp. Chlamydia pneumoniae. Only Mycoplasma spp. returned positive (1.70E 02 CT: 35.23). The patient has been asymptomatic for approximately 5 years and has not relapsed.
3. Discussion
This is a particularly severe case of babesiosis (piroplasmosis) in an immunocompetent patient with a spleen. Babesia is a protozoan, unicellular parasite closely related to Plasmodium, the agent of malaria, often transmitted by ticks [1]. However, there may be other vectors, such as horseflies [2]. Although the patient traces the history of her illness back to her stay in Amazonia, an infestation in Auvergne could not be ruled out. Babesiosis is usually described in patients who have undergone splenectomy, and the clinical picture in these cases is particularly acute and severe, with disseminated intravascular coagulation, splenic infarction or rupture, leading to a clinical picture of septic shock [3, 4]. Nevertheless, in our experience, it is a frequent infestation in immunocompetent patients presenting with persistent polymorphic syndrome after a possible tick bite (SPPT).
Patients presenting with piroplasmosis often complain of chills, hot-cold sensations, profuse sweating, sometimes febrile, shortness of breath; arthralgias and myalgias are also described [4-6]. The clinical picture may suggest attenuated malaria, which is not surprising given the parasite's kinship with Plasmodium. SPPT is often due to a combination of Borrelia with other crypto-infections (co-infections) [7, 8]. In our experience, patients with severe and chronic forms of Lyme disease present with multiple co-infections, Babesia, Bartonella, Ehrlichia, Anaplasma, Rickettsia, Coxiella for example. In a series of 105 patients, 41% had positive serology for Babesia, and this parasite was detected, by PCR, in 6 out of 50 patients (12%) [7]. These results differ from a seroprevalence study looking for both Babesia microti and Babesia divergens carried out between 2002 and 2003 in a subgroup 810 forestry workers in the Grand-Est region of France (seropositive for at least one of the following: Borrelia burgdorferi s.l., Francisella tularensis, tick-borne encephalitis virus, Anaplasma phagocytophilum or Bartonella henselae), which found a seroprevalence of 0.1% for Babesia divergens and 2.5% for Babesia microti (9). These workers were not necessarily suffering from SPPT. It should be noted that there are other parasites close to Babesia, such as Theileria spp. which we found by PCR in 17 of the 33 patients for whom the test was carried out, 5 times in capillary blood (29.4%), once in urine (5.9%) and 11 times in saliva (64.7%) [8]. The efficacy of the first treatment with doxycycline and chloroquine could have led to this diagnosis, among others. However, hydroxychloroquine, which has some efficacy on Babesia, is also effective on Borrelia, and potentiates the action of antibiotics by alkalinizing the phagolysosome [10, 11]. Hydroxychloroquine also has its own anti-inflammatory and anti-infectious action.
Treatment was spectacularly effective, with complete remission rapidly achieved. It should be noted that treatment was accompanied by a temporary recrudescence of symptoms, with lumbar pain and very heavy sweating, which we interpreted as a Jarisch-Herxheimer reaction specific to Babesia infestation [12]. There was only one clinical relapse, not microbiologically documented; it is possible that treatment needs to be spread out long enough, perhaps 120 days, the lifespan of a red blood cell (as it is electively invaded by the parasite). Overall, therefore, diagnosis remains difficult, as little is known about this condition, due to its polymorphous clinical presentation, and the difficulty of obtaining a reliable biological diagnosis (serology only tests for antibodies to Babesia divergens, not Theileria, and furthermore smear and PCR tests are not performed in routine practice). We believe that patients presenting with SPPT or a suggestive clinical presentation (chills, unexplained profuse sweating) should be tested by serology and PCR several days in a row (to sensitize the diagnosis) and in several different matrices (blood, urine, saliva, capillary blood) [8]. Cautious empiric treatment can also always be discussed on a case-by-case basis.
5. Conclusion
Babesiosis is a diagnosis to be evoked, particularly in patients presenting with SPPT with chills, unexplained sweats, febrile illness, even in the absence of a history of splenectomy. Blood smears, serology and PCR can be helpful in making the diagnosis. Given the current difficulty of microbiological diagnosis, an empiric treatment with anti-piroplasmic drugs may also be considered.
Funding
The authors declare that this study received funding from Association Bon Sens to cover the publication fees.
References
- Westblade LF, Simon MS, Mathison BA, Kirkman LA. Babesia microti: from Mice to Ticks to an Increasing Number of Highly Susceptible Humans. J Clin Microbiol 55 (2017): 2903-2912.
- François Fournier, Frédéric Durand, Eric Estramon, Yannick Lequette, Christian Perronne, Michel Franck, et al. Real Time Micro Organisms Pcr in 82 Horseflies in France. Archives of Microbiology and Immunology 7 (2023): 83-95.
- Hatcher JC, Greenberg PD, Antique J, Jimenez-Lucho VE. Severe babesiosis in Long Island: review of 34 cases and their complications. Clin Infect Dis 32 (2001): 1117-25.
- Cunha BA, Nausheen S, Szalda D. Pulmonary complications of babesiosis: case report and literature review. Eur J Clin Microbiol Infect Dis 26 (2007): 505-8.
- Svensson J, Lazarevic V, Bläckberg J, Olsson M, Persson K. Babesia-infektion kan vara vanligare i Sverige än vi tidigare trott - Parasiten kan spridas via fästingar och blodtransfusion [Babesiosis could be more common in Sweden than previously thought]. Lakartidningen 116 (2019): FL4D.
- Berghoff W. Chronic Lyme Disease and Co-infections: Differential Diagnosis. Open Neurol J 6 (2012): 158-78.
- Alexis Lacout, Marie Mas, Michel Franck, Véronique Perronne, Julie Pajaud, Pierre Yves Marcy, et al. Serological and PCR evidence of Infection in 105 Patients with SPPT. Archives of Microbiology & Immunology 5 (2021): 139-150.
- Lacout A, Mas M, Pajaud J, Perronne V, Lequette Y, Franck M, Perronne C. Real time micro-organisms PCR in 104 patients with polymorphic signs and symptoms that may be related to a tick bite. Eur J Microbiol Immunol (Bp) 11 (2021): 62–75.
- Rigaud E, Jaulhac B, Garcia-Bonnet N, Hunfeld KP, Féménia F, Huet D, et al. Seroprevalence of seven pathogens transmitted by the Ixodes ricinus tick in forestry workers in France. Clin Microbiol Infect 735 (2016): 735.
- Brorson O, Brorson SH. An in vitro study of the susceptibility of mobile and cystic forms of Borrelia burgdorferi to hydroxychloroquine. Int Microbiol 5 (2002): 25-31.
- Rizk MA, El-Sayed SA, AbouLaila M, Tuvshintulga B, Yokoyama N, Igarashi I. Large-scale drug screening against Babesia divergens parasite using a fluorescence-based high-throughput screening assay. Vet Parasitol 30 (2016): 93-7.
- Pound MW, May DB. Proposed mechanisms and preventative options of Jarisch-Herxheimer reactions. J Clin Pharm Ther 30 (2005): 291-5.