Adenocarcinomatous Transformation of a Retroperitoneal Teratoma Mimicking an Adrenal Incidentaloma in an Adult Female: a Case Report and Literature Review
Article Information
Babwah F*, Kumar V, Evans M, Karnik U, Bhatnagar A, Garnham A, Buch H
Department of Medicine, The Royal Wolverhampton NHS Trust, Wolverhampton, England, United Kingdom
*Corresponding Author: Dr. Babwah F, Department of Medicine, The Royal Wolverhampton NHS Trust, Wolverhampton, England, United Kingdom
Received: 14 July 2019; Accepted: 29 July 2019; Published: 30 September 2019
Citation: Babwah F, Kumar V, Evans M, Karnik U, Bhatnagar A, Garnham A, Buch H. Adenocarcinomatous Transformation of a Retroperitoneal Teratoma Mimicking an Adrenal Incidentaloma in an Adult Female: a Case Report and Literature Review. Archives of Clinical and Medical Case Reports 3 (2019): 372-381.
View / Download Pdf Share at FacebookAbstract
Retroperitoneal teratomas are extremely rare in adults and are typically benign tumors. We describe a case of a 48-year-old lady who initially presented with abdominal discomfort 18 years ago and was found to have a large right-sided supra-renal mass suspected to be an adrenal lesion. Following initial biochemical and imaging studies a diagnosis of non-functioning adrenal adenoma was made and she was managed conservatively. After being lost to follow up and remaining clinically well for many years, she once again presented with worsening abdominal pain. A right adrenalectomy was performed and the histology surprisingly confirmed a mature cystic teratoma with malignant transformation into a moderately-differentiated intestinal-type adenocarcinoma as well as having a focus of carcinoid tumour. She was admitted shortly afterwards with widespread metastatic disease and sadly passed away before any treatment could be instituted. Only a handful of cases of primary retroperitoneal teratomas have described adenocarcinomatous transformation. A carcinoid tumour within a teratoma is even less common and typically does not manifest systemic features. This case underlines the broad differential diagnosis of an adrenal mass and highlights several unusual aspects of a teratoma. We present the current literature and discuss the appropriate investigations, management and challenges involved in such rare cases.
Keywords
Teratoma; Adrenal Incidentaloma; Malignant Ttansformation; Carcinoid
Teratoma articles Teratoma Research articles Teratoma review articles Teratoma PubMed articles Teratoma PubMed Central articles Teratoma 2023 articles Teratoma 2024 articles Teratoma Scopus articles Teratoma impact factor journals Teratoma Scopus journals Teratoma PubMed journals Teratoma medical journals Teratoma free journals Teratoma best journals Teratoma top journals Teratoma free medical journals Teratoma famous journals Teratoma Google Scholar indexed journals Adrenal Incidentaloma articles Adrenal Incidentaloma Research articles Adrenal Incidentaloma review articles Adrenal Incidentaloma PubMed articles Adrenal Incidentaloma PubMed Central articles Adrenal Incidentaloma 2023 articles Adrenal Incidentaloma 2024 articles Adrenal Incidentaloma Scopus articles Adrenal Incidentaloma impact factor journals Adrenal Incidentaloma Scopus journals Adrenal Incidentaloma PubMed journals Adrenal Incidentaloma medical journals Adrenal Incidentaloma free journals Adrenal Incidentaloma best journals Adrenal Incidentaloma top journals Adrenal Incidentaloma free medical journals Adrenal Incidentaloma famous journals Adrenal Incidentaloma Google Scholar indexed journals Malignant Ttansformation articles Malignant Ttansformation Research articles Malignant Ttansformation review articles Malignant Ttansformation PubMed articles Malignant Ttansformation PubMed Central articles Malignant Ttansformation 2023 articles Malignant Ttansformation 2024 articles Malignant Ttansformation Scopus articles Malignant Ttansformation impact factor journals Malignant Ttansformation Scopus journals Malignant Ttansformation PubMed journals Malignant Ttansformation medical journals Malignant Ttansformation free journals Malignant Ttansformation best journals Malignant Ttansformation top journals Malignant Ttansformation free medical journals Malignant Ttansformation famous journals Malignant Ttansformation Google Scholar indexed journals health articles health Research articles health review articles health PubMed articles health PubMed Central articles health 2023 articles health 2024 articles health Scopus articles health impact factor journals health Scopus journals health PubMed journals health medical journals health free journals health best journals health top journals health free medical journals health famous journals health Google Scholar indexed journals Carcinoid articles Carcinoid Research articles Carcinoid review articles Carcinoid PubMed articles Carcinoid PubMed Central articles Carcinoid 2023 articles Carcinoid 2024 articles Carcinoid Scopus articles Carcinoid impact factor journals Carcinoid Scopus journals Carcinoid PubMed journals Carcinoid medical journals Carcinoid free journals Carcinoid best journals Carcinoid top journals Carcinoid free medical journals Carcinoid famous journals Carcinoid Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Retroperitoneal articles Retroperitoneal Research articles Retroperitoneal review articles Retroperitoneal PubMed articles Retroperitoneal PubMed Central articles Retroperitoneal 2023 articles Retroperitoneal 2024 articles Retroperitoneal Scopus articles Retroperitoneal impact factor journals Retroperitoneal Scopus journals Retroperitoneal PubMed journals Retroperitoneal medical journals Retroperitoneal free journals Retroperitoneal best journals Retroperitoneal top journals Retroperitoneal free medical journals Retroperitoneal famous journals Retroperitoneal Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals Teratoma articles Teratoma Research articles Teratoma review articles Teratoma PubMed articles Teratoma PubMed Central articles Teratoma 2023 articles Teratoma 2024 articles Teratoma Scopus articles Teratoma impact factor journals Teratoma Scopus journals Teratoma PubMed journals Teratoma medical journals Teratoma free journals Teratoma best journals Teratoma top journals Teratoma free medical journals Teratoma famous journals Teratoma Google Scholar indexed journals Adenocarcinomatous articles Adenocarcinomatous Research articles Adenocarcinomatous review articles Adenocarcinomatous PubMed articles Adenocarcinomatous PubMed Central articles Adenocarcinomatous 2023 articles Adenocarcinomatous 2024 articles Adenocarcinomatous Scopus articles Adenocarcinomatous impact factor journals Adenocarcinomatous Scopus journals Adenocarcinomatous PubMed journals Adenocarcinomatous medical journals Adenocarcinomatous free journals Adenocarcinomatous best journals Adenocarcinomatous top journals Adenocarcinomatous free medical journals Adenocarcinomatous famous journals Adenocarcinomatous Google Scholar indexed journals
Article Details
1. Introduction
Teratomas are uncommon embryonic germ cell tumours (GCT) that have the potential to differentiate to any cell type. They are more frequent during childhood and most occur in gonads, with retroperitoneal teratomas accounting for only 4% of all teratomas [1]. They can be classified according to their maturity, morphology and location. Mature cystic teratomas are typically benign. Malignant transformation of a mature teratoma is rare and occurs in 1-2% of ovarian and 2-3% of testicular teratomas [2]. Few case reports have described benign retroperitoneal teratomas undergoing malignant transformation. These can present as non-germ cell, somatic cancers and the diagnosis are often only confirmed after histological examination of the resected lesion. There are no established treatment guidelines and therefore the management is challenging. We present a case of a premenopausal lady with a longstanding diagnosis of a right-sided adrenal incidentaloma which was later histologically confirmed to be a mature cystic teratoma of the retroperitoneum with intestinal-type adenocarcinoma and a focus of carcinoid. Written informed consent was obtained from the patient.
2. Case Presentation
A 48-year-old female manager presented to us in July 2017 with a 6-month history of non-specific right abdominal pain and tenderness exacerbated by exercise. She denied palpitations, night sweats, weight loss or gastrointestinal symptoms and her periods were regular. She was normotensive, a teetotaller, a non-smoker and not on any regular medications. There was no significant family history. At the age of 30, this lady was incidentally detected to have a 12 cm right adrenal mass at another institute. According to the available historic correspondence, she had had a full endocrine work-up, serial imaging and surgical review during the initial 3 years after its detection. It was concluded that the adrenal mass was non-functional and benign and an observational policy was followed. She was then lost to follow-up and had remained asymptomatic for 15 years.
When reviewed in our clinic, a ballotable mass in the right flank could easily be appreciated. Ultrasonography demonstrated a 14.4 x 7.9 cm complex mass in the right adrenal area with both cystic and solid components. Repeat endocrine investigations were within normal limits. A computed tomogram (CT) scan showed a 12.4 x 12.4 x 11.2 cm heterogeneous supra-renal mass with areas of fluid density, fat density and coarse calcifications (Figure 1a & 1b). She was seen in the joint surgical-endocrine clinic and booked for an open right adrenalectomy on 12th December, 2017, in view of the recent onset symptoms and concern about the size of the tumour.
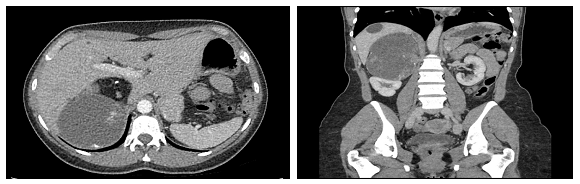
Figure 1 (a and b): CT scan showing a large, right-sided heterogeneous retroperitoneal mass with areas of fat, fluid and calcifications
The surgery was technically challenging as the large retroperitoneal tumour was found to be indented the inferior vena cava and had to be mobilized from both liver and kidney (Figure 2). The tumour was close to resection margins, but macroscopically completely resected, measuring 15 cm in maximum dimension and weighing 898.4 g. Histology was complex consisting of three main pathological entities - a mature cystic teratoma of the retroperitoneum encasing the right adrenal gland, a focus of trabecular carcinoid completely excised with no mitotic figures and no necrosis (Ki-67 proliferation index of 1%) and a moderately-differentiated intestinal-type adenocarcinoma arising from dysplastic epithelium within the teratoma (Figure 3b and 3d). Immunostaining showed strong positivity to caudal-type homebox transcription factor-2 (CDX-2) and patchy positivity for cytokeratin 7 and cytokeratin 20 (Figure 3e). Florid vascular and perineural invasion were noted along with lymph node involvement. The tumour was found to involve resection margins microscopically and based on its complex histology the case was referred to the local Oncology multidisciplinary team (MDT). On 28th January, 2018 she presented to the Emergency Unit with a 2-week history of headache and a new onset generalized tonic-clonic seizure. Magnetic resonance (MR) imaging demonstrated a discrete left frontal lesion with associated oedema consistent with a metastatic deposit (Figure 4). She was commenced on dexamethasone 8 mg BD and levetiracetam 500 mg BD and referred urgently to the Neurosurgical team with a plan to consider surgical resection and whole brain radiotherapy.
A staging CT scan of thorax, abdomen and pelvis on 2nd February, 2018 showed left supraclavicular, mediastinal, hilar and abdominal lymphadenopathy, pulmonary metastases and probable lymphangitis carcinomatosis (Figure 5). Cancer antigen 19-9 (CA 19-9) biomarker increased exponentially from its baseline value pre-surgery (Table 1). Left supraclavicular lymph node biopsy was performed and the histology showed features consistent with a metastatic moderately differentiated adenocarcinoma as demonstrated in the retroperitoneal teratoma.
Management plan made by the Oncology team included gastrointestinal-specific chemotherapy consisting of 5FU, oxaliplatin and capecitabine. Unfortunately, prior to any intervention she again presented to the hospital on 23rd March, 2018 with rapidly progressive dyspnoea secondary to a pleural effusion. Further active management was deemed inappropriate and end of life care pathway was followed. She sadly passed away a few days later.

Figure 2: Intraoperative view showing a large right-sided retroperitoneal mass intended by the IVC and displacing it anteriorly.
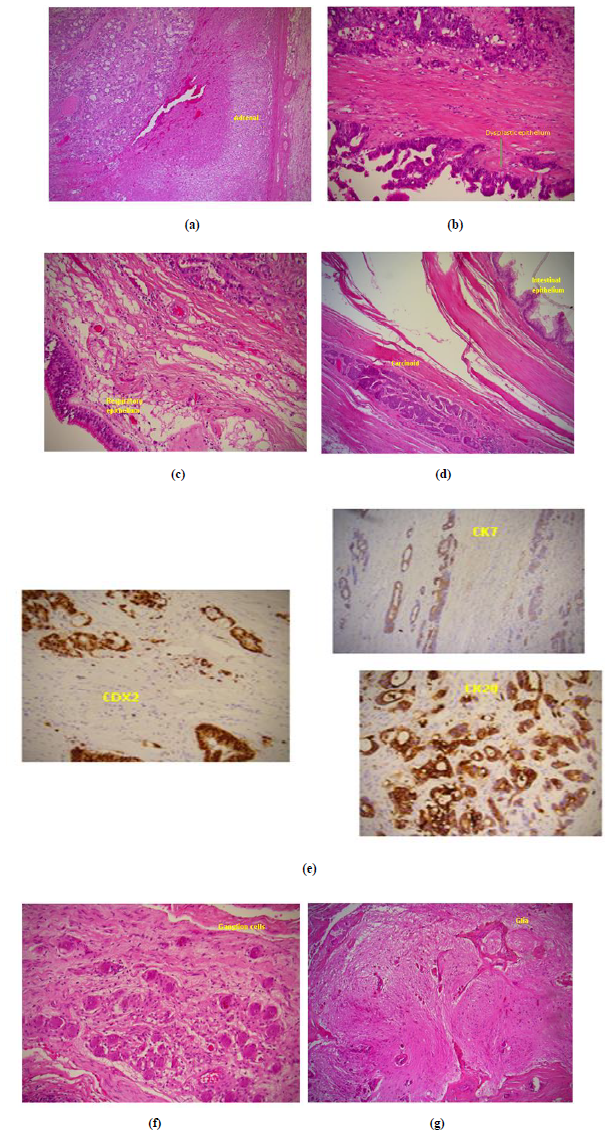
Figure 3: Histology slides; a. Normal adrenal; b. Dysplastic epithelium; c. Respiratory epithelium; d. Intestinal epithelium and carcinoid focus; e. Immunostaining for CDX2, CK7 and CK20; f. Ganglion cells; g. Glia.
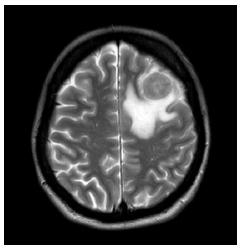
Figure 4: MRI head showing a solitary metastasis with surrounding oedema.
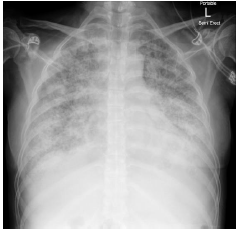
Figure 5: Chest x-ray showing lymphangitis carcinomatosis.
|
Date |
Tumour markers |
Result |
Reference range |
|
12/07/2017 |
CA 125 |
48.3 KU/l |
0.1 – 35.0 KU/l |
|
12/07/2017 |
CA 19-9 |
101 KU/l |
0 – 37 KU/l |
|
05/09/2017 |
CA 19-9 |
189 KU/l |
0 – 37 KU/l |
|
01/02/2018 |
AFP |
<1.7 KU/l |
<10 KU/l |
|
21/02/2018 |
CA 125 |
98.4 KU/l |
0.1 – 35 .0 KU/l |
|
21/02/2018 |
CA 19-9 |
9594 |
0 – 37 KU/l |
|
21/02/2018 |
CA 15-3 |
16 |
0.1-31.0 KU/l |
|
21/02/2018 |
24 hour 5HIAA |
18 umol/coll |
- |
CA125 - cancer antigen 125, CA 19-9 – cancer antigen 19-9, CA 125 – cancer antigen 125, AFP – alfa-fetoprotein, 5HIAA – 5-Hydroxyindoleacetic acid.
Table 1: Summary of tumour markers
3. Discussion
The term teratoma is derived from the Greek words ‘teras and ‘oma’ (monster and tumor) [3, 4]. Teratomas are uncommon congenital tumours that arise from pluripotential embryonic cells [5]. They contain derivatives from two or more germ cell layers (ectoderm, endoderm and mesoderm) [6] and therefore can contain different and anatomically peculiar somatic tissues such as hair, teeth, bone and even entire body organs. They belong to a class of tumours known as non-seminomatous germ cell tumours (GCT) and generally occur in the gonadal regions (ovaries and testis) [3]. Extragonadal sites include anterior mediastinal, retroperitoneal and sacro-coccygeal regions in order of frequency and as per developmental migration they occur as midline structures [7, 8]. Teratomas can be classified in several ways depending on their location, morphology and histology.
A primary retroperitoneal teratoma is rare and accounts for 1%-11% of all primary retroperitoneal tumours in adul [1, 7]. They are twice more common in females [6, 9] and have a bimodal incidence, presenting either within the first 6 months of life or during early adulthood [7]. Only a fifth present beyond the age of 30 and they have a predilection for the upper pole of the left kidney [8, 9]. Retroperitoneal masses are discovered quite late as they are usually asymptomatic until they become large enough to exert pressure over the surrounding structures. Patients have described non-specific abdominal discomfort, back pain, genitourinary symptoms and lower limb swelling, depending on the lesion’s specific location. The differential diagnosis is wide and includes ovarian tumours, renal cysts, adrenal tumours, retroperitoneal fibromas, retroperitoneal sarcomas and enlarged lymph nodes [10, 11].
In view of its close anatomical proximity to the adrenal gland, it is no surprise that a retroperitoneal lesion could be perceived to be of adrenal origin and be managed as per an adrenal incidentaloma pathway, as was the case with this patient. The adrenal gland is involved in only 4% of primary retroperitoneal teratomas [12]. A primary adrenal teratoma is exceptional, accounting for 0.13% of all adrenal lesions [13] and, as with retroperitoneal teratomas, is more common in premenopausal females and typically located on the left [14]. Diagnosis of a retroperitoneal lesion is usually made on imaging, namely ultrasound which can easily define its size and identify cystic and/or solid components and the presence of calcification. Plain x-rays can detect calcification in up to 61.5% of all teratomas [7] but this does not distinguish between a benign or malignant process as 12.5% of malignant teratomas also demonstrate calcification [15]. CT is superior in being able to identify and quantitatively assess various components such as soft-tissue density, fat and sebaceous content based on the Hounsfield unit [3]. CT is also essential in delineating resection margins preoperatively and assessing for metastatic disease. Our patient had both ultrasound and CT imaging while under surveillance and pre-operatively.
Benign characteristics of a teratoma include a cystic appearance, mature tissue and presence of sebum. It has been reported that overall, adult retroperitoneal teratomas have a 25.8% chance of malignancy compared to 6.8% in childhood [3]. However the ones that are mature and cystic are generally considered to be benign, even in adults [9, 16] and rarely do such teratomas undergo malignant transformation, as was seen in our patient. Immature teratomas, on the other hand, have an inherent malignant potential and can be aggressive [17]. Features of malignancy include solid tumours and the presence of immature embryonic tissue, such as fat, cartilage, fibrous and bony tissue [10]. This patient’s lesion demonstrated both benign (mature cystic appearance, presence of sebum and calcification) and malignant (solid components and adenocarcinomatous transformation) features.
In our patient the teratoma demonstrated malignant transformation (TMT). This is seen in only 1% of all teratomas [6] with the other forms of malignant teratomas being immature teratomas and teratomas associated with other malignant GCT elements [6]. TMT is defined pathologically when non-germ cell malignancies or malignant somatic cells emerge from within a previously benign teratoma. Most cases are detected between the age 30-70 years [18, 19]. Tumour size >9.9 cm and duration of disease are risk factors for TMT [20, 21], both of which were exemplified in the present case. While the predominant histological cell type is squamous cell carcinoma, seen in 75% of cases of ovarian teratoma [6, 22], retroperitoneal teratomas transforming into an adenocarcinoma have been reported in the literature. Cases of signet ring cell-, mucinous- and intestinal-type adenocarcinomas have all been described [23-26].
TMT with adenocarcinomatous transformation is associated with poorer prognosis [27]. They have the potential to metastasize and are considered resistant to chemotherapy and radiotherapy [28, 29]. Other markers of poor prognosis include cyst wall invasion, rupture, tumour dissemination, ascites and adhesions [27]. There are no established guidelines for the management of such rare cases of retroperitoneal teratomas with malignant transformation. Surgical resection is the mainstay of treatment and yields a good prognosis if complete [29]. However, patients often have metastatic disease at presentation and therefore have a much grimmer prognosis. While no standard adjuvant therapy is recommended, some centres have published good outcomes with the addition of targeted chemotherapy based on the transformed histology [28, 30].
The other unusual feature of the tumour in our patient was the presence of a carcinoid tumour arising from a mature cystic retroperitoneal teratoma, which has been reported in less than 5% of cases of TMT [27]. This is primarily a histological diagnosis as patients typically do not demonstrate features of carcinoid syndrome (flushing, bronchospasm, diarrhoea) as there is no systemic release of vasoactive peptides. Our patient did not report any such symptoms. While the significance of mitotic index and Ki 67 proliferation index are not validated in the context of an intra-teratoma carcinoid focus, by analogy with lung and gastrointestinal neuroendocrine tumours, it is likely that absence of such features is associated with less aggressive behaviour. This case highlights the vast potential of teratomas to proliferate into multiple other tissues. Treatment strategies for such cases have not been established, but complete surgical resection as above is first-line with a few case reports showing no recurrence 24-31 months of follow-up [31, 32]. The role of somatostatin analogues in these cases has not been established.
Tumour markers such as alfa-fetoprotein (AFP), carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 19-9 are occasionally elevated in the presence of retroperitoneal teratomas [16, 33]. Elevated AFP has been reported to fall following tumour resection and rise again with disease recurrence [15]. A retrospective analysis of 215 patients with mature cystic ovarian teratomas showed that CA 19-9 had the highest positivity rate, among other tumour markers and correlated with tumour size [34]. Similarly, in the present case CA 19-9 was 3-fold elevated on initial assessment and levels surged exponentially with metastatic disease. While the use of these biomarkers is not advocated in diagnosis, they can be useful in gauging disease progression and detecting post -treatment recurrence.
Our case was a challenging one, as this lady was a young, clinically well patient who was lost to follow-up with a stable retroperitoneal mass for over 17 years. Her lesion was mislabelled as an adrenal incidentaloma with no adverse imaging or biochemical characteristics and therefore an observational policy was not unreasonably initially agreed to a patient’s request. Histology however, demonstrated several adverse prognostic features including malignant transformation with lymphovascular invasion and nodal involvement with a poor clinical outcome. In retrospect, based on the criterion of size she should have been offered surgical resection at the time of initial assessment.
4. Conclusion
Retroperitoneal teratomas are rare in adults and because of their location they can be easily mistaken for an adrenal incidentaloma. 1 in 4 cases prove to be malignant and therefore we propose that any sizable lesion with atypical features for a myelolipoma should be considered for early surgical intervention. Prognosis for a mature cystic retroperitoneal teratoma is excellent if complete surgical excision is achieved. Less frequently, malignant transformation can occur which carries a worse prognosis. In such cases, targeted chemotherapy based on the transformed histology can be offered as adjuvant therapy.
References
- Mathur P, Lopez-Viego MA, Howell M. Giant primary retroperitoneal teratoma in an adult: A case report. Case Rep Med 3 (2010).
- Niu M, Liu A, Zhao Y, et al. Malignant transformation of a mature teratoma of the adrenal gland: A rare case report and literature review. Medicine (Baltimore) 96 (2017): e8333.
- Gupta R, Reddy Y, Gupta R, et al. Primary benign cystic retroperitoneal teratoma in an asymptomatic adult. BBJNTCT 1 (2013).
- Sakurai H, Asamura H, Suzuki K, et al. Management of primary malignant germ cell tumor of the mediastinum. Jpn J Clin Oncol 34 (2004): 386-392.
- Weinstein BJ, Lenkey JL, Williams S. Ultrasound and CT demonstration of a benign cystic teratoma arising from the retroperitoneum. Am J Roentgenol 133 (1979): 936-938.
- Thambi R, Johnson G, Leelamma JP. Adenocarcinoma: A surprise diagnosis in a middle-aged woman with retroperitoneal teratoma. Libyan J Med Sci 2 (2018): 111-113.
- Gschwend J, Burke TW, Woodward JE, et al. Retroperitoneal teratoma presenting as an abdominal-pelvic mass. Obstet Gynecol 70 (1987): 500-502.
- Engel RM, Elkins RC, Fletcher BD. Retroperitoneal teratoma. Review of the literature and presentation of an unusual case. Cancer 22 (1968): 1068-1073.
- Khan SA, Mahmood T, Sarwar MZ, et al. Retroperitoneal Teratoma in an adult presenting with painful abdominal mass: case history and literature review. BJMP 5 (2012): a509.
- Pantoja E, Llobet R, Gonzalez-Flores B. Retroperitoneal teratoma: a historical review. J Urol 115 (1976): 520-523.
- Pandya JS, Pai MV, Munchhala S. Retroperitoneal teratoma presenting as acute abdomen in an elderly person. Ind Jou Gastroentero 19 (2000): 89-90.
- Ratkal JM, Shaik NJ, Salia D, et al. Rare primary retroperitoneal teratoma masquerading as adrenal incidentaloma. Afr J Urol 21 (2015): 96-99.
- Shuqiang LI, Hanzhong LI, Zhigang ji, et al. Primary adrenal teratoma: Clinical characteristics and retroperitoneal laparoscopic resection in five adults. Oncol Lett 10 (2015): 2865-2870.
- Kuo EJ, Sisk AE, Yang Z, et al. Adrenal Teratoma: a Case Series and Review of the Literature. Endocr Pathol 28 (2017): 152-158.
- Bruneton JN, Diard F, Drouillard JP, et al. Primary retroperitoneal teratoma in adults: Presentation of two cases and review of the literature. Radiology 134 (1980): 613-616.
- Gatcombe, et. al. Primary Retroperitoneal Teratomas: A review of the literature. Journal of Surgical Oncology 86 (2004): 107-113.
- Huang X, Liu B, Xie L. Giant primary retroperitoneal teratoma in an adult female patient: A case report. Oncol Lett 6 (2013): 460-462.
- Ayhan A, Bukulmez O, Genc C, et al. Mature cystic teratomas of the ovary: Case series from one institution over 34 years. Eur J Obstet Gynecol Reprod Biol 88 (2000): 153-157.
- Singh P, Yordan EL, Wilbanks GD, et al. Malignancy associated with benign cystic teratomas (dermoid cysts) of the ovary. Singapore Med J 29 (1988): 30-34.
- Morinaga S, Nomori H, Kobayashi R, et al. Well-differentiated adenocarcinoma arising from mature cystic teratoma of the mediastinum (teratoma with malignant transformation). Report of a surgical case. Am J Clin Pathol 101 (1994): 531-534.
- Ulker V, Numanoglu C, Akbayir O, et al. Malignant transformation arising from mature cystic teratoma of the ovary: a report of six cases. J Obstet Gynaecol Res 38 (2012): 849-853.
- Petousis S, Kalogiannidis I, Margioula-Siarkou C, et al. Mature Ovarian Teratoma with Carcinoid Tumor in a 28-Year-Old Patient. Case Reports in Obstetrics and Gynecology (2013): ID 108582.
- Chu PY, Teng TH, Lee CC, et al. Adenocarcinomas arising from primary retroperitoneal teratoma in an adult female patient. Int J Urol 13 (2006): 1352-1354.
- Song ES, Choi SJ, Kim L, et al. Mucinous adenocarcinoma arising from one retroperitoneal mature cystic teratoma in a postmenopausal woman. J Obstet Gynaecol Res 31 (2005): 127-132.
- Terado Y, Kurata A, Ishida T, et al. Adenocarcinoma of small intestinal type in retroperitoneal mature teratoma. Pathol Int 60 (2010): 701-705.
- Cheung WL, Cao D. Colonic-type adenocarcinoma arising in a primary retroperitoneal mature cystic teratoma. Pathol Int 58 (2008): 792-796.
- Arora DS, Haldane S. Carcinosarcoma arising in a dermoid cyst of the ovary. J Clin Pathol 49 (1996): 519-521.
- Kim JH, Lee TS, Oh HK, et al. A case of mucinous adenocarcinoma arising from retroperitoneal teratoma treated with chemoradiation. J Gynecol Oncol 20 (2009): 126-128.
- Donadio AC, Motzer RJ, Bajorin DF, et al. Chemotherapy for teratoma with malignant transformation. J Clin Oncol 21 (2003): 4285-4291.
- Lin C, Du Y, Li Y, et al. Superior mediastinal mature cystic teratoma with gastrointestinal adenocarcinoma transformation: Report of a case. Oncotarget 7 (2016): 38392-38397.
- Shindo K, Ueda J, Toubo T, et al. Primary carcinoid tumor in a retroperitoneal mature teratoma: report of a case. Surg Today 43 (2013): 694-697.
- Yamasaki T, Yagihashi Y, Shirahase T, et al. Primary carcinoid tumor arising in a retroperitoneal mature teratoma in an adult. Int J Urol 11 (2004): 912-915.
- Lin MCH, Ng K, Hung CF, et al. Dyspnoea as a clinical manifestation in primary retroperitoneal teratoma. Chin J Radiol 26 (2001): 141-145.
- Ustunyurt E, Gungor T, Iskender C, et al. Tumor markers in mature cystic teratomas of the ovary. Arch Gynecol Obstet 279 (2009): 145-147.
