Accepting A Kidney with Polycystic Kidney Disease from A Cadaver Donor: A Case Report
Article Information
Maher Mohammed Aldemerdash*
King Fahad Specialist Hospital, Dammam, Saudi Arabia
*Corresponding Author: Maher Mohammed Aldemerdash, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Received: 10 August 2021; Accepted: 13 September 2021; Published: 01 October 2021
Citation: Maher Mohammed Aldemerdash. Accepting a Kidney with Polycystic Kidney Disease from a Cadaver Donor: A Case Report. Archives of Nephrology and Urology 4 (2021): 124-127.
View / Download Pdf Share at FacebookAbstract
Faced with the long waiting list for a kidney transplant, the use of donors with expanded criteria, like polycystic kidneys, is an option that aims to increase in a short time the supply of kidneys for transplant. Here we present of a patient with end stage renal failure and limited vascular access who received a deceased donor kidney from a 33-year-old who develop intracranial hemorrhage who likely had undiagnosed Polycystic Kidney Disease. The transplant went uneventful and showed promising results, and the recipient ended up with a good renal function. The option of using donors with polycystic kidneys is safe and gives good results.
Keywords
Polycystic kidney disease; Cadaver; Renal failure; ESRD; Transplant
Polycystic kidney disease articles; Cadaver articles; Renal failure articles; ESRD articles; Transplant articles
Polycystic kidney disease articles Polycystic kidney disease Research articles Polycystic kidney disease review articles Polycystic kidney disease PubMed articles Polycystic kidney disease PubMed Central articles Polycystic kidney disease 2023 articles Polycystic kidney disease 2024 articles Polycystic kidney disease Scopus articles Polycystic kidney disease impact factor journals Polycystic kidney disease Scopus journals Polycystic kidney disease PubMed journals Polycystic kidney disease medical journals Polycystic kidney disease free journals Polycystic kidney disease best journals Polycystic kidney disease top journals Polycystic kidney disease free medical journals Polycystic kidney disease famous journals Polycystic kidney disease Google Scholar indexed journals Cadaver articles Cadaver Research articles Cadaver review articles Cadaver PubMed articles Cadaver PubMed Central articles Cadaver 2023 articles Cadaver 2024 articles Cadaver Scopus articles Cadaver impact factor journals Cadaver Scopus journals Cadaver PubMed journals Cadaver medical journals Cadaver free journals Cadaver best journals Cadaver top journals Cadaver free medical journals Cadaver famous journals Cadaver Google Scholar indexed journals Renal failure articles Renal failure Research articles Renal failure review articles Renal failure PubMed articles Renal failure PubMed Central articles Renal failure 2023 articles Renal failure 2024 articles Renal failure Scopus articles Renal failure impact factor journals Renal failure Scopus journals Renal failure PubMed journals Renal failure medical journals Renal failure free journals Renal failure best journals Renal failure top journals Renal failure free medical journals Renal failure famous journals Renal failure Google Scholar indexed journals ESRD articles ESRD Research articles ESRD review articles ESRD PubMed articles ESRD PubMed Central articles ESRD 2023 articles ESRD 2024 articles ESRD Scopus articles ESRD impact factor journals ESRD Scopus journals ESRD PubMed journals ESRD medical journals ESRD free journals ESRD best journals ESRD top journals ESRD free medical journals ESRD famous journals ESRD Google Scholar indexed journals Transplant articles Transplant Research articles Transplant review articles Transplant PubMed articles Transplant PubMed Central articles Transplant 2023 articles Transplant 2024 articles Transplant Scopus articles Transplant impact factor journals Transplant Scopus journals Transplant PubMed journals Transplant medical journals Transplant free journals Transplant best journals Transplant top journals Transplant free medical journals Transplant famous journals Transplant Google Scholar indexed journals computed tomography articles computed tomography Research articles computed tomography review articles computed tomography PubMed articles computed tomography PubMed Central articles computed tomography 2023 articles computed tomography 2024 articles computed tomography Scopus articles computed tomography impact factor journals computed tomography Scopus journals computed tomography PubMed journals computed tomography medical journals computed tomography free journals computed tomography best journals computed tomography top journals computed tomography free medical journals computed tomography famous journals computed tomography Google Scholar indexed journals end stage renal disease articles end stage renal disease Research articles end stage renal disease review articles end stage renal disease PubMed articles end stage renal disease PubMed Central articles end stage renal disease 2023 articles end stage renal disease 2024 articles end stage renal disease Scopus articles end stage renal disease impact factor journals end stage renal disease Scopus journals end stage renal disease PubMed journals end stage renal disease medical journals end stage renal disease free journals end stage renal disease best journals end stage renal disease top journals end stage renal disease free medical journals end stage renal disease famous journals end stage renal disease Google Scholar indexed journals hemodialysis articles hemodialysis Research articles hemodialysis review articles hemodialysis PubMed articles hemodialysis PubMed Central articles hemodialysis 2023 articles hemodialysis 2024 articles hemodialysis Scopus articles hemodialysis impact factor journals hemodialysis Scopus journals hemodialysis PubMed journals hemodialysis medical journals hemodialysis free journals hemodialysis best journals hemodialysis top journals hemodialysis free medical journals hemodialysis famous journals hemodialysis Google Scholar indexed journals Autosomal dominant polycystic kidney disease articles Autosomal dominant polycystic kidney disease Research articles Autosomal dominant polycystic kidney disease review articles Autosomal dominant polycystic kidney disease PubMed articles Autosomal dominant polycystic kidney disease PubMed Central articles Autosomal dominant polycystic kidney disease 2023 articles Autosomal dominant polycystic kidney disease 2024 articles Autosomal dominant polycystic kidney disease Scopus articles Autosomal dominant polycystic kidney disease impact factor journals Autosomal dominant polycystic kidney disease Scopus journals Autosomal dominant polycystic kidney disease PubMed journals Autosomal dominant polycystic kidney disease medical journals Autosomal dominant polycystic kidney disease free journals Autosomal dominant polycystic kidney disease best journals Autosomal dominant polycystic kidney disease top journals Autosomal dominant polycystic kidney disease free medical journals Autosomal dominant polycystic kidney disease famous journals Autosomal dominant polycystic kidney disease Google Scholar indexed journals
Article Details
1. Introduction
Patients under the age of 40 years rarely develop end-stage renal disease (ESRD); however, approaching the age of 60 years, end-stage renal disease requiring dialysis increases in frequency. The treatment of choice in patients who have progressed to ESRD is dialysis or transplantation [1]. Kidney transplant as the treatment for ESRD helps return renal function to an adequate level and offers patients an opportunity to resume their professional and social life. It is a well-established fact that patients receiving a kidney from a deceased donor have an improved quality of life and a better chance at long-term survival than patients who are on a transplantation waiting list. The supply of the organs, however, does not fulfill their demand.
Polycystic kidney disease (PKD) is one of the major primary renal diseases that necessitate renal transplant. It is a genetic tubulointerstitial disease that causes progressive loss of renal function and the development of multiple cysts in renal parenchyma [2]. The literature is scattered with case reports of patients who have received kidneys from a deceased ADPKD donor showing encouraging outcomes [3-7].
Here we provide our experience of a patient with end stage renal failure who received a deceased donor kidney from a 33-year-old who develop intracranial hemorrhage and brain edema who likely had an undiagnosed ADPKD.
2. Case Presentation
2.1 The donor
A 33-year male with no known comorbidities presented to the hospital with loss of consciousness with GCS of 8/15, with no history of trauma. Emergency computed tomography (CT) scan showed intracranial hemorrhage with severe brain edema. He was admitted to the intensive care unit (ICU). His creatinine on admission was 103 mmol/L with no previous labs to compare it with. He had an episode of hypotension 83/51 mmHg that was supported with inotropes. He developed AKI afterward with a peak of creatinine 255 mmol/L and creatinine of 93 mmol/L at the time of Kidney retrieval. Urine analysis was negative for proteinuria, hematuria, leukocytes, or casts. Urine output was around 2L/24 hours. His IgG was positive for CMV and EBV. He was negative for HBV, HCV, HIV, HTLV, and Syphilis. His abdominal imaging (ultrasound and CT) showed multiple Liver cysts, two simple Renal cysts in the right and one on the left. Those findings and with the history could suggest that he could have had an undiagnosed ADPKD.
During his hospital stay, his GCS was deteriorating, and he was declared brain dead. After discussing his case with the Transplant committee, we accepted and retrieved his left Kidney.
2.2 The recipient
A 22-year-old female with end stage renal disease (ESRD) secondary to unknown primary. She has been of intermittent hemodialysis (IHD) with limited vascular access for five years. past history was not significant, and there was no family history of Renal disease. The donor: recipient Human Leucocyte Antigen (HLA) mismatch was 2:2:2 at HLA's A:B:DR. All her preoperative serologies were negative except for IgG CMV and EBV. She was counseled about the risk and benefits of this Kidney, especially with her limited vascular access. Her surgery was uneventful. The graft had one artery, one vein, and one ureter. The cold ischemic time was 8 hours and 8 minutes. The warm ischemic time was 52 minutes, and the anastomosis time was 32 minutes. She received Thymoglobulin and Methylprednisolone as induction agents, followed by our usual maintenance protocol Cellcept (1g PO BID), Tacrolimus (aiming for a Tacrolimus level 8-10), and prednisone taper (30 mg po daily).
She developed delayed graft function post-operatively and required dialysis once for Hyperkalemia. Her creatinine started improving, as shown in the figure 1.
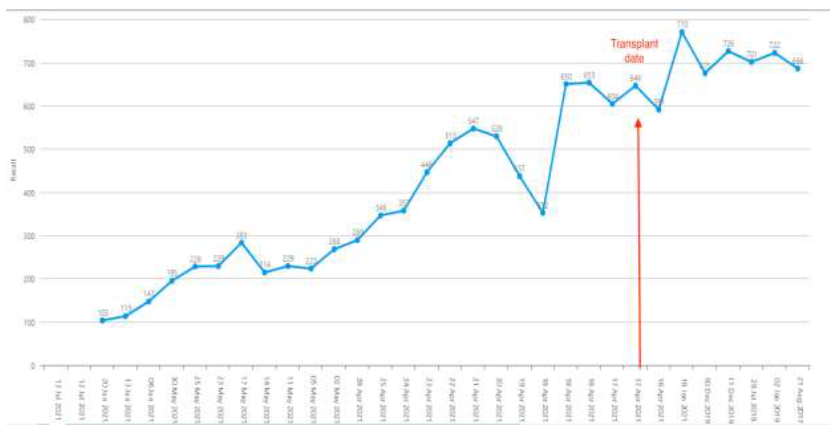
Figure 1: Showing improvement in creatinine.
3. Discussion
Autosomal dominant polycystic kidney disease (ADPKD) is a hereditary disease that causes cysts formation in the kidneys and gradual impairment of renal function. Accounting for 2-9 percentage of the population, it frequently ends in renal failure. ADPKD symptoms develop in adulthood with 85% of the carriers developing symptoms in the fourth decade of life [8]. Etiological causes of ESRD include ADPKD in 10-15 percent of the cases. However, the development of renal failure following the beginning of ADPKD symptoms generally takes 10 years. The probability of progression to renal failure in 50-year-old patients is 23%, but it increases to 48% in 70-year-old patients [9, 10]. In the case of the unavailability of donor kidneys, the transplantation of an ADPKD kidney is considered viable if the parenchyma and renal function are intact. Currently, the 16 cases reported in the literature have had excellent transplant outcomes, with immediate function in 81% of the cases. Good renal function has been observed in 8 cases with follow-up exceeding 3 years. A case of excellent renal function with a 15-year follow-up has also been reported [11].
Concerns about transplanting an ADPKD kidney mainly center around the risk of cyst growth that can progress to renal failure. However, Howards et al. [4] reported that the development of ESRD following transplantation of an ADPKD kidney with cyst size up to 34 mm can take 12.5 years. Donor age is a key factor determining the time the transplanted organ can survive. A kidney transplant from a 21-year-old deceased donor should allow a minimum of 10 years of kidney function. Infection, cyst rupture, and bleeding are other rare but potential risks, especially when a biopsy is required for renal transplant. With the administration of Calcineurin-based immunosuppressants, graft survival has improved considerably in the last four decades. Comparing mortality between patients on dialysis who were on the transplant waiting list and patients receiving transplants from deceased donors, transplant patients were found to have lower mortality after a 2-year follow-up. Bearing in mind the wide gap between the demand and supply of kidney donors, and the quality of life with a functional kidney, a patient may receive a deceased donor ADPKD kidney with an adequate renal function depending upon the graft survival period with immunosuppression and the approximate time it would take for the deceased donor kidney to fail [12].
This fact confirm the option of using donors with PKD is safe and give good results especially if the potential recipient has limited vascular access for dialysis.
References
- Parfrey PS, Bear JC, Morgan J, et al. The diagnosis and prognosis of autosomal dominant polycystic kidney disease. N Engl J Med 323 (1990): 1085-1090.
- Wilson PD. Polycystic kidney disease. N Engl J Med 350 (2004): 151-164.
- Siegal B. The polycystic kidney donor. Transplantation 54 (1992): 1131.
- Howard RJ, Reed AI, Van der Werf WJ, et al. Development of polycystic disease in a kidney 10 years after transplantation. Transplantation 68 (1999): 1620.
- Shamali A, Milsom-Mcquillan S, Gibbs P. Outcomes of renal transplant from donors with polycystic kidney disease. International Journal of Surgery 51 (2018): 229-232.
- Mancini G, Comparini L, Salvadori M. Transplant of a polycystic kidney because of organ shortage. Transplantation proceedings (1990).
- Shan Y, Lee P, Sy E, et al. Polycystic kidney patient as a cadaveric donor: is it appropriate? Nephrology, dialysis, transplantation 16 (2001): 410-411.
- Roozbeh J, Razmkon AR, Jalaeian H, et al. Outcome of kidney transplantation in patients with polycystic kidney disease: a single center study. Saudi J Kidney Dis Transpl 19 (2008): 72-75.
- Churchill DN, Bear JC, Morgan J, et al. Prognosis of adult onset polycystic kidney disease re-evaluated. Kidney Int 26 (1984): 190-193.
- Olsburgh JD, Godbole HC, O'Donnell PJ, et al. Transplantation of kidneys from deceased adult polycystic donors. Am J Transplant 6 (2006): 2809-2811.
- Eng MK, Zorn KC, Harland RC, et al. Fifteen-year follow-up of transplantation of a cadaveric polycystic kidney: a case report. Transplant Proc 40 (2008): 1747-1750.
- Wolfe RA, Ashby VB, Milford EL, et al. Comparison of Mortality in All Patients on Dialysis, Patients on Dialysis Awaiting Transplantation, and Recipients of a First Cadaveric Transplant 341 (1999): 1725-1730.
