Acceptability, Willingness to use and Preferred Distribution Models of Oral- Based HIV Self-Testing Kits among Key and Priority Populations Enrolled in HIV Pre-Exposure Prophylaxis Clinics in Central Uganda. A Mixed-Methods Cross-Sectional Study
Article Information
John Bosco Junior Matovu1§, Roy William Mayega2*, Sylvia Nalubega3*, Jayne Byakika-Tusiime4*
1School of Public Health, Busitema University, Mbale, Uganda
2Department of Epidemiology and Biostatistics, School of Public Health Makerere University, Kampala, Uganda
3Department of Nursing, School of Health Sciences, Soroti University, Soroti, Uganda
4Department of Public Health, School of Health Sciences, Soroti University, Soroti, Uganda
*These authors have contributed equally to the work.
*Corresponding author: John Bosco Junior Matovu, School of Public Health, Busitema University, Mbale, Uganda.
Received: 18 October 2022; Accepted: 27 October 2022; Published: 05 November 2022
Citation: John Bosco Junior Matovu, Roy William Mayega, Sylvia Nalubega, Jayne Byakika-Tusiime. Acceptability, Willingness to use and Preferred Distribution Models of Oral-Based HIV Self-Testing Kits among Key and Priority Populations Enrolled in HIV Pre-Exposure Prophylaxis Clinics in Central Uganda. A Mixed-Methods Cross-Sectional Study. Archives of Clinical and Biomedical Research 6 (2022): 933-943.
View / Download Pdf Share at FacebookAbstract
Background: Key Populations (KPs) and Priority Populations (PPs) taking Pre-Exposure Prophylaxis (PrEP) for HIV prevention require routine HIV testing every after three months hence can benefit from HIV self-testing (HIVST). We assessed the acceptability of oral-based HIVST among Key and priority Populations taking PrEP in central Uganda.
Materials and Methods: A mixed methods cross-sectional study was conducted on 367 KPs and PPs attending PrEP clinics in central Uganda in August 2018. Quantitative data analysis included inferential statistics to determine associations between social-demographic and economic characteristics, and study outcomes using multivariable logistic regression, quoting p-values less than 5% at 95% confidence interval. Thematic analysis was performed to explore factors that promote and inhibit HIVST.
Results: HIV self-testing acceptability; defined as the proportion of respondents who performed the test among those approached was 99.5% (365/367). Choice of HIVST was predicted by education level, (primary versus other: AOR 0.403; 95% CI 0.204-0.794; p<.009), willingness to pay for HIVST kits was predicted by clinic location (Urban vs Rural: AOR 0.041; 95% CI 0.018-0.97; p<.001) and KP category (FSW versus others: AOR 4.605; 95% CI, 1.497-14.172. Respondents who attained post-primary education preferred to pay less than 1.4 USD for an oral HIVST kit (AOR 2.064; 95% CI 1.006-4.237; p<.048). Oral fluid-based kit “Oraquick” was preferred over other HIV testing modalities because it was painless, convenient, easy to use and time saving.
Conclusion: Oral-based HIV self-testing is highly acceptable among key and priority populations taking Pre-Exposure Prophylaxis and can be adopted as an alternative to the conventional routi
Keywords
Acceptability; HIV self-testing; Key Populations; Oral-Based; Oraquick; Priority Populations; Pre-exposure Prophylaxis
Acceptability articles; HIV self-testing articles; Key Populations articles; Oral-Based articles; Oraquick articles; Priority Populations articles; Pre-exposure Prophylaxis articles
Article Details
1. Introduction
Globally, an estimated 84% of all people living with Human Immunodeficiency Virus (HIV) know their status [1]. As the world prepares to end AIDS by 2030, the remaining undiagnosed people living with HIV need to be identified, initiated and maintained on treatment to achieve viral suppression [2]. In Uganda, most of the new HIV infections occur in Key Populations (KPs) and Priority Populations(PPs) who include sex workers, fisher folks, long distance truck drivers, uniformed service personnel, men who have sex with men (MSM), and boda-boda taxi-men [3]. Pre-Exposure Prophylaxis (PrEP) was introduced as a biomedical intervention to reduce the risk of HIV acquisition among people with ongoing risk of HIV acquisition such as KPs and PPs. Commonly used PrEP medication is a formulation of a fixed dose combination drug consisting of Tenofovir (TDF) and Emtricitabine (FTC), taken daily as long as the risk of HV acquisition remains. However, injectable PrEP formulations such as long acting Cabotegravir have been developed and provide better adherence on PrEP hence better prevention outcomes. People taking PrEP are required to test for HIV every three months to ascertain their HIV negative status so as to continue with prevention services. Currently, there is only one existing testing method for routine follow up testing of KPs on PrEP: that is, blood-based test either at the clinic (facility) or at community outreach centers. HIV Self-Testing (HIVST) is an HIV testing approach where a person collects his or her own specimen (oral fluid or blood), performs an HIV test and interprets the result, often in a private setting, either alone or with someone he or she trusts [4]. Providing a variety of HIV testing options is a good strategy for increasing HIV testing uptake and would potentially improve HIV testing among KPs and PPs leading to early linkage to post-test services [5]. Studies conducted on HIV self-testing worldwide have shown high but varying levels of acceptability across age, gender and sub-populations [6-11] including people who take PrEP [12]. However, studies have documented barriers to acceptability of HIVST as unease of use, cost of the test kits, and lack of accessibility to professional support after self-testing [10, 13] For effective implementation and optimisation of the outcomes of HIVST, these barriers and concerns need to be adequately addressed. There is limited literature about studies conducted to determined acceptability of HIV self-testing using an oral based kit among KPs and PPs who are taking PrEP. We aimed to determine the proportion of Key and Priority Populations taking Pre-Exposure Prophylaxis for HIV in central Uganda who accept oral-based HIV Self-Testing, the preferred HIV testing method for routine testing while on PrEP, their willingness to pay for the kits and the amount they are willing to pay and to establish the preferred HIV Self-Testing kit distribution approaches/models. Our study builds on existing literature about HIV self-testing and contributes a new dimension of using HVST as a favorable HIV testing approach among KPs and PPs on PrEP during routine three monthly follow up testing.
2. Materials and Methods
2.1 Study Design and Setting
This cross-sectional study employed both quantitative and qualitative research methods and was conducted between May and August 2018 at two clinics in Uganda where PrEP was being offered: Most at Risk Population Initiative (MARPI) clinic in Kampala city and Kasensero HC II in Rakai district. The study targeted all people categorized as key populations [Men who have sex with Men (MSM), People who inject drugs (PIDs), Female sex workers (FSWs)] and priority populations [(Fisher folks, Adolescent girls and young women (AGYWs) and negative people in discordant sexual relationships)] who had been enrolled and active on PrEP at both PrEP clinics by December 2018. Two emancipated minors aged 17 years belonging to the adolescent girls and young women category were considered for the study and written informed consent was obtained from each of their guardians before enrolment [14, 15]. We excluded respondents who had ever performed HIV self-testing prior to the study and those who were unable to provide consent on their own either due to ill health, altered mental state or any other reason. We estimated the sample size using the Kish Leslie formula for cross-sectional studies for a single sample proportion for a categorical outcome.
N= Calculated sample size
P= assumed sample proportion that accepts HIVST estimated at 85% (P=0.85).
The estimated acceptability of 85% was based on assumptions that HIVST was new in the study population and there was no in-country data on acceptability of HIVST in the study population, hence we anticipated the below that of Nangendo et al. [6] and Ngure et al. [12], hence we expected a lower acceptance rate of HIVST among study participants compared to the general population
1-P = The probability of not accepting the HIVST
Z1-α/2 = Standard normal deviate at 95% confidence interval (z=1.96)
δ =acceptable margin of error acceptability of 5%.
D=Design effect of 1.5 was included in the sample size estimate because our respondents were sampled from two different clinics (Clusters) purposively selected, and further still, respondents were being reviewed at each of those clinics serving as clusters. An estimated dropout rate of 20% was considered because HIVST was a new intervention among respondents.
Due to logistical reasons and the dynamic nature of the study population, we employed a consecutive convenience sampling strategy. Potential participants were screened for eligibility as they came for their clinic appointments until the desired sample size was achieved for each clinic to make a total of 367 respondents. The primary outcome (dependent) variable for the study was acceptability to use HIV self-testing at this follow up visit. Acceptability was defined as the proportion of respondents who used the oral HIVST kit out of those reached with the HIVST. Secondary outcomes were preferred method of HIV testing during routine follow up monitoring, willingness to pay for the HIVST kit, amount to pay for an HIVST kit and the preferred model of distributing HIVST kits. Social, demographic, and economic data including age, gender, KP/PP category, education level, occupation, marital status and religion, and level of income were assessed
2.2 Data Collection and Management
Data collection took place between May and August 2018. Quantitative data was collected using an interviewer administered structured questionnaire in English language and questions were directly translated in the preferred local language during the interview session for respondents who did not understand English. In-depth individual interviews were used to collect qualitative data after collection of the quantitative data. Respondents were informed of the availability of HIVST and the standard HIV testing services at the clinic, followed by a demonstration of HIV self-testing procedure by research assistants using a demonstration video and leaflet inserts in the HIVST pack. The demonstration involved three steps: preparing for oral fluid sample collection, using the kit to test for HIV, and interpreting test results. Respondents were asked if they were willing to perform a self-test and those willing were asked to voluntarily consent after which, they were provided with an Oraquick HIVST kit to perform self-testing (accepting) and interpret the results. As a quality assurance measure, research assistants supervised the self-testing procedure. Respondents who tested HIV positive (five in number) on self-testing were subjected to a confirmatory test using the national HIV testing algorithm. Respondents who tested HIV positive on confirmatory testing (four in number) did not continue with the questionnaire.
2.3 Data Analysis
Quantitative data was analyzed using SPSS analytic software version 24.0 package. Univariate analysis was used to calculate the descriptive statistics for each of the independent variables. Categorical variables were summarized as proportions, while the continuous variable (age) was summarized using the median and standard deviation. Initially, each independent variable was assessed separately for its association with the outcome variables (HIV testing kit type preference, willingness to pay and amount one is willing to pay for an HIVST) using bivariate logistic regression, and we presented crude odds ratio (COR), 95% confidence interval (CI), and p-values. Independent variables found significant at a p-value less than 0.05 were added to the multivariable model. We determined HIVST kit distribution model preference by computing the proportion of respondents who would prefer any of the available testing kit distribution models. The amount one was willing pay was captured in Uganda shillings (UGX) and converted in USD equivalent during analysis. The qualitative study employed an in-depth interview technique to gather data from participants and followed the quantitative data collection. We interviewed 20 participants with effort to ensure variation between KP categories, gender and testing site. Purposive sampling was used to select the participants and the principle of data saturation (where no new insights emerge from the data) was used to guide participant enrolment into the study. Recorded information was transcribed verbatim and important statements were identified and extracted. The thematic analysis approach was employed for data analysis and results were presented in a narrative form alongside and to support the quantitative results.
2.4 Power Calculations
Based on post Clopper-Pearson confidence interval formula, with a sample size of 367, a width of 0.5 and a sample proportion, we were powered to detect the observed primary outcome with >90% power.
2.5 Ethics Approval and Consent to Participate
The study protocol was reviewed and approved by the Busitema University Faculty of Health Sciences Higher Degrees and Research Committee and the Mbale Regional Referral Hospital Research and Ethics Committee (Ref No. MRRH-REC-IN-COM 024/2018). All respondents provided written informed consent and were free to opt out of the study at any stage of the study.
3. Results
3.1 Participants
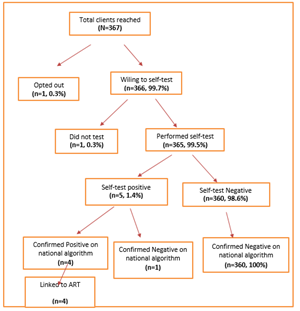
A total of three hundred sixty-seven (367) respondents were contacted, one respondent opted out and preferred not to be interviewed for personal reasons. Of the 366 respondents who were willing to perform HIV self-testing, 365 performed the test and five respondents tested HIV positive. The five HIV positive respondents were subjected to national HIV testing algorithm (Determine, Statpack, SD Bioline) and four were confirmed HIV positive. All positive participants were linked to Anti-Retroviral Therapy (ART) clinics for initiation on treatment. The fifth respondent who tested HIV negative on the national HIV testing algorithm was considered HIV negative (Figure 1). For the qualitative component, twenty interviews were conducted, eleven males and nine females with an age range of 19-40. Of the twenty participants, five female sex workers, three people who use and inject drugs, three MSM, six HIV negative people in sero-discordant sexual relationships, two young people and one fisherman. Twelve participants were from MARPI Mulago while eight were from Kasensero HC III clinics. Four main themes emerged from the qualitative study which were generally aligned to the study aim. These were: acceptability of HIVST, choice of an HIV testing approach, preferred kit distribution models and willingness to pay for the test.
3.2 Socio Demographic and Economic Characteristics of Participants
Three hundred sixty-six (366) individuals were included in the study. The median age was 27 (SD=7.5), the youngest participant was 17 years while the oldest at 54 years, 54.1% (n=198) were from urban settings, 49.2% (n=180) were males, 34.2% (n=125) were female sex workers and 48.4% (n=177) had attained up to primary education. About 34% (n=124) were married or cohabiting and more than half, 52.5% (n=192) were Catholics. Casual labor was the major source of income contributing to 62.6% (n=229) as detailed in table 1 below.
|
Site |
n(N=366) |
% |
|
MARPI Mulago (Urban) |
198 |
54.1 |
|
Kasensero (Rural) |
168 |
45.9 |
|
Age category |
34 |
9.3 |
|
17-19 |
96 |
26.2 |
|
20-24 |
103 |
28.1 |
|
25-29 |
56 |
15.3 |
|
30-34 |
42 |
11.5 |
|
35-39 |
21 |
5.7 |
|
40-44 |
14 |
3.8 |
|
45 and above |
||
|
Gender |
||
|
Male |
180 |
49.2 |
|
Female |
186 |
50.8 |
|
Education level |
||
|
Never went to school |
25 |
6.8 |
|
Primary |
177 |
48.4 |
|
Secondary |
141 |
38.5 |
|
Tertiary institutions (none-degree) |
13 |
3.6 |
|
University |
10 |
2.7 |
|
Marital status |
||
|
Single/Never Married |
117 |
32 |
|
Married/Cohabiting |
124 |
33.9 |
|
Divorced/Separated/widowed |
125 |
34.2 |
|
Religion |
||
|
Catholic |
190 |
51.9 |
|
Protestant |
70 |
19.1 |
|
Muslim |
72 |
19.7 |
|
Others |
||
|
Key/Priority population category |
||
|
FSW |
125 |
34.2 |
|
Fisher Folks |
79 |
21.6 |
|
MSM |
47 |
12.8 |
|
PWID |
45 |
12.3 |
|
Discordant Negative |
36 |
9.8 |
|
AGYW |
31 |
8.5 |
|
Transgender |
3 |
0.8 |
|
Source of income |
||
|
Casual labor |
229 |
62.6 |
|
Formally employed (Gov't/NGO/Private) |
24 |
6.6 |
|
Self Employed |
84 |
23 |
|
In school, not employed |
7 |
1.9 |
|
Farmer |
22 |
6 |
Table 1: Socio demographic and economic characteristics of the study participants.
3.3 Acceptability of HIV Self-Testing
Acceptability was computed as a proportion of clients who performed an HIV self-test out of those that were reached with HIV self-testing. Of the 367 participants who were reached, 365 performed HIV self-testing translating into an acceptability of 99.5%. One participant declined to take the kit and one other participant who took the kit did not perform the self-test. Participants felt HIVST was an approach that would reduce obstacles associated with current approaches and reported HIVST to be time saving, cost effective, private and accessible (‘you move with your lab’).
The other problem is having to line up, I may come but when I have no time for lining up and I go back without being tested. I will sit until the line is completed, yet here I will be alone and still go when I know whom I am (M05, MSM).
Respondents felt HIVST was particularly important for special groups who feel stigmatised when they visit health facilities. Particularly, FSWs and MSMs reported this concern and felt society has not accepted them and discriminates them, hence found HIVST more convenient. Not only does HIVST save time, but also enables to bridge the HIV testing provider-HIV tester time mismatch for special categories of people, such as sex workers, who work during night and rest during day.
Like for us (MSM), there are those who do not want to be identified. When they just want to be in hiding, but for us we bump on them. This method will be helpful when they come to know their status and take care accordingly, because they may say they have no time, and you offer them the test (M05, MSM).
Respondents viewed HIVST as an approach that would help them reduce the risk of acquiring HIV, through testing their sexual partners before engaging in sex. In addition to routine follow up testing while on PrEP, HIVST was reported to be useful in mobilizing peers for HIV testing thus increasing the number of people who will become aware of their HIV status.
It is good because it is handy, any time when you have someone, you can use it with a customer (sex customer), because many will fear to go to the clinic. So it is safe for you to move with your own test (M10, FSW).
I was excited as a person and I thought if I can have somewhere to find them I would not be worried, because like some of us who use drugs, you may be there high on drugs and you just pick up a woman, and by the time you come to your senses, you regret your actions, […]. But when you have that test, it becomes easy for you to test yourself and take caution to protect your-self (M01, PUWD).
Respondents expressed trust in HIVST compared to facility-based testing, citing that by performing a self-test, they would receive correct results and would not doubt a result from a test they performed themselves. One respondent cited an example of false HIV test results received at a facility and felt HIVST would be a solution to such a problem.
The other thing is that here I will be able to see the results by myself and know that, I am like this. This is how my status is, when I can personally see the results. Because you may be told that you are OK, because it happened to me two times, by the time I came here for testing, I first cheeked myself in two places, and they were telling me that I was not ok, so someone invited me to come to this place. When I arrived, they told me that I was HIV negative, and I took long to accept it (M03, Discordant). HIV self-testing was regarded as an approach that would eliminate mistrust between health workers and their clients since clients would take the driving sit in knowing their HIV status. Despite its high acceptability, psychological/emotional stress associated with an HIV positive test result was a concern. Participants felt that whereas HIV self-testing provides privacy, it also stood the challenge of lack of emotional support in case one turned HIV positive due to lack of post-test counselling irrespective of the HIV test result. Other respondents felt HIVST could give false results if one panics and ends up misinterpreting the test results.
Counselling for this approach is lacking. For example, if you have always known yourself to be HIV negative and you find yourself HIV positive, handling the situation may be difficult when you are alone, with no body to council you. That’s the only problem or side effect I see with this approach (M07, FSW).
The other issue is that some people have weak hearts. You may test yourself and find him reading a negative result as a positive because of panic (M06, MSM).
However, emotional concerns were expressed by six of the twenty respondents that participated in the qualitative interview. Nevertheless, there is need for exploring further, the emotional concerns following HIVST as this study did not have an in-depth evaluation of them, yet they have been reported in literature as significant concerns of the HIVST approach.
3.4 Preferred HIV Testing Method, Willingness to Pay for the Kit, Amount One was willing to Pay and Preferred Kits Distribution Model
3.4.1 Preferred method for HIV Testing during Routine follow up Monitoring while on PrEP: Majority of respondents (88.4%, n=319) preferred to use an oral fluid based HIVST for routine three monthly HIV testing while on PrEP compared to the conventional health care provider-dependent and facility-based HIV testing (8.6%, n=31). Only 3% (n=11) preferred a blood based self-test kit if introduced in the future. In table 2. The independent predictor of preference for Oral fluid HIVST was the education level where respondents who attained post-primary education were 0.0403 less likely to prefer the HIVST oral kit to other HIVST methods (AOR 0.403; 95% CI 0.204-0.794; p<.009). Other social demographic characteristics did not significantly predict test kit preference.
Table 2: Distribution of respondents by preferred HIV testing method (N=366).
AOR: Adjusted Odds Ratio; CI: Confidence Interval; COR: Crude Odds Ratio
Participants highlighted various advantages of the oral based HIVST over the other two HIV testing options as being: non-invasive, not painful, no blood loss, and easy to use.
I would prefer the oral based test, because for it will not be difficult like the others. The one of a finger prick may be difficult for me to use, because I do not want to be pricked. They prick you and you get damages on your fingers (M05, MSM/MSW)
From among the three, this one of oral fluid test is the best because, the other two are painful. You are removing one which pains and replacing it with another painful one. It is not good to feel the pain of the needle. But this one is very simple; I just rub it around the teeth. So, this one is so far the best of all the three (M08, PWUD).
Other participants expressed a fear of continued blood loss during HIV testing procedures that involved blood-based testing. People on PrEP were particularly concerned as they frequently underwent HIV testing, on a three-monthly basis. Some felt that the continued blood loss could cause them health complications, yet with the oral fluid-based test, no such fears could arise.
I have found this one (oral fluid based HVST approach) different from others because for me, I don’t want to lose my blood, because sometimes when there are checking you, they take off quite a lot of blood. So, with this method, I will not lose blood and yet I will receive correct results, and I am the one who has also tested myself, I have not wasted time going to hospital, I have done the test by myself, and I have received correct results, without losing blood or experiencing pain. So I find this quite unique from other methods (M02, Discordant).
Ease of use of the HIVST kit was reported to be a factor influencing the choice of the kit to other HIV testing kits.
And sometimes you may use it (the finger prick-based test) wrongly since you are not a health professional. So, it may not treat you well. But this method is so far the best (M01, PUWD).
These findings did not differ much from other studies conducted elsewhere [10,17,18] which revealed high acceptability of HIVST.
3.4.2 Willingness to Pay and Amount to Pay for HIV Self-Testing Kits: Majority of respondents (73.2%, n=264) were willing to pay for HIV self-testing kits, of which 85.6% (n=226), were willing to pay an amount not exceeding 5000/ Uganda shillings ($1.4). In table 3, the independent predictors of willingness to pay for the HIVST kits were site location and KP/PP category. Respondents belonging to a rural clinic were less willing to pay for HIVST kits compared to those at an urban PrEP clinic (AOR 0.041; 95% CI 0.018-0.97; p<.001). Belonging to a KP/PP category other than FSW was significantly associated with willingness to pay for the kits (AOR 4.605; 95% CI, 1.497-14.172; p<.008). In Table 4, the independent predictor of amount to pay for Oral fluid HIVST was the education level of respondents, where people who attained post-primary education were more likely to pay an amount less than 1.4 USD HIVST for an oral kit (AOR 2.064; 95% CI 1.006-4.237; p<.048).
Table 3: Willingness to pay for HIV self-testing kits.
AOR: Adjusted Odds Ratio; CI: Confidence Interval; COR: Crude Odds Ratio.
|
Variable |
Up to $ 1.4 |
Above $1.4 |
Unadjusted |
95% CI |
p value |
|
(N=226) |
N= (38) |
COR |
|||
|
(n, %) |
n (%) |
||||
|
Site location |
|||||
|
MARPI Mulago (Urban) |
87 (82.1) |
19 (17.9) |
Reference |
||
|
Kasensero (Rural) |
139 (88.0) |
19 (12.0) |
0.626 |
(0.314-1.248) |
0.183 |
|
Gender |
|||||
|
Male |
92 (82.9) |
19 (17.1) |
Reference |
||
|
Female |
134 (87.6) |
19 (12.4) |
0.687 |
(0.345-1.368) |
0.285 |
|
Age |
|||||
|
Below 29 |
140 (84.3) |
26 (15.7) |
Reference |
||
|
30 and above |
86 (87.8) |
12 (12.2) |
0.751 |
(0.360-1.567) |
0.446 |
|
Marital status |
|||||
|
Single/Never Married |
60 (80) |
15 (20.0) |
Reference |
||
|
Married/Cohabiting |
77 (85.6) |
13 (14.4) |
0.675 |
(0.299-1.527) |
0.346 |
|
Divorces/Separated/Widowed |
89 (89.9) |
10 (10.1) |
0.449 |
(0.189-1.067) |
0.07 |
|
Education |
|||||
|
Primary |
117 (90.0) |
13 (10.0) |
Reference |
||
|
Other |
109 (81.3) |
25 (18.7) |
2.064 |
(1.006-4.237) |
0.048 |
|
Religion |
|||||
|
Catholic |
123 (88.5) |
16 (11.5) |
Reference |
||
|
Other |
103 (82.4) |
22 (17.6) |
1.642 |
(0.819-3.291) |
0.162 |
|
KP/PP Category |
|||||
|
FSW |
90 (88.2) |
12 (11.8) |
Reference |
||
|
Other |
136 (84.0) |
26 (16.0) |
1.434 |
(0.688-2.987) |
0.336 |
|
Source of income |
|||||
|
Casula labor |
137 (87.3) |
20 (12.7) |
Reference |
||
|
Other |
89 (83.2) |
18 (16.8) |
1.385 |
(0.695-2.763) |
0.355 |
Table 4: Amount to pay for HIV self-testing kits.
AOR: Adjusted Odds Ratio; CI: Confidence Interval; COR: Crude Odds Ratio.
Whereas majority of respondents were willing to pay for the kits, the cost of the kits was reported as a potential hinderance to access and use of HIVST:
If this kit comes at a cost, it will be difficult for me to pay. Why…because I do not have a permanent job which I can use to pay. But if it comes free of charge, everyone will want to use it. Because many of us do not have permanent jobs, we only get temporally jobs which pay us little income. So if you want us to use the test, and for people to like it, it is good if you give it out freely (M06, MSM).
If the test came at a cost that is a dead deal…it’s a dead deal because not everyone has money. There are those who have, meaning it will be the rich to use them (M08, PWUD).
As for me I want it freely. At least if it came at around 2000 ($0.6), there I can afford, but still you see that even people fail to afford a pregnancy test, so when you are doing something, you also put into consideration that people fall under different categories (M10, FSW).
3.4.3 Preferred HIV Self-Testing Kit Distribution Approaches:
Of the 330 respondents who preferred to use HIVST as an approach for routine HIV testing while on PrEP, 121 (33.1%) preferred home delivery of testing kits by health workers, 108 (29.5%) preferred picking the kits from PrEP clinics, 74 (20.2%), preferred home delivery by peers while 27 (7.4%) preferred accessing the kits from private facilities.
We also have our peers who can distribute them to us. Even I am also a peer, so we can get condoms and go and distribute them to the communities. So even this approach can work. They train you and you come to know how to use it. Because for me I know but there is someone who does not know. So, that approach would work, especially for us (MSMs), who don’t want to go to hospital, who can even spend a year, or six months, such people would benefit a lot more (M05, MSM).
For me I have no problem because I have many health facilities around me but there are some people living in the villages when they need to travel for about 20 miles to access it. So I request that if it is possible, the government should provide the tests free of charge and they should be available everywhere, not only in large health facilities, not only in the cities, but also in villages, so that everyone can access it easily (M02, Discordant).
To some respondents, delivering the kits to private facilities would compromise the quality of the kits
I don’t want to find it from any other place, because they are many people who duplicate. Like this test, you may find its duplicates by tomorrow. So if the government decides to bring them, we should access them from the main hospital, Mulago, from a qualified doctor (M08, PWUD).
The above findings suggest that in determining the models of HIVST kit distribution, accessibility by the users, privacy, and cost implications should be considered.
4. Discussion
Our findings reveal that HIVST is highly acceptable among people taking PrEP irrespective of their social demographic and economic characteristics. These findings are comparable to other studies; for instance, acceptability of HIVST was 100% among pregnant women in India [16] and 98% among KPs on PrEP who were in sero discordant relationships in Kenya, [12]. Our study, having catered for a variety of KPs and PPs including MSM, sero discordant HIV negative people, FSW, PWUIDS, fisher folks, adolescent young girls and women provides grounded evidence on the acceptability of HIV self-testing among people taking PrEP. Acceptability results in the quantitative study are further justified by the qualitative findings in which respondents singled out key reasons to justify self-testing as: the procedure being time saving, cost effective (eliminates transport costs), private, and accessible. These findings are similar to those from previous research [17]. Compared to other studies elsewhere, KPs and PPs are willing to pay for HIVST but the cost of the kits may restrict their use as revealed by Ng OT and others. In their study to determine accuracy and user acceptability of HIV self-testing using Oraquick HIVST kit, 87.4% of participants were willing to pay for the kit, but only 28% could afford the kit at a market price of five USD [18]. Similarly, Maheswaran and others [19], in their study entitled “Cost and quality of life analysis of HIV self-testing and facility-based HIV testing and counselling in Blantyre” recommended that HIVST would be affordable if the kits were subsidized to a cost comparable to that of routine HIV facility based testing. Our findings further suggest that HIVST test kits should be free of charge or at a very minimal cost that KPs and PPs can afford. Key and priority populations taking PrEP prefer use of multiple modes to access HIVST kits. The most preferred models were home delivery of kits by health workers, picking kits from a from health facility, and home delivery of kits by peers. These findings relate with those from other studies which where home based delivery [20], facility based distribution, and peer facilitated delivery [5] of testing kits were preferred. Our study had several limitations: We employed a non-probability consecutive convenience sampling method to enroll respondents (due to time and logistical constraints plus the dynamic nature of the study population) hence not all respondents had equal chance of being selected. This could have led to a selection bias. Providing HIV self-testing kits to respondents and requesting them to test on the same day could have influenced their decision to accept self-testing without adequately reflecting on their choice. A better method would have been to let respondents take kits home and decide to or not to perform self-testing. The Oral fluid HIV testing kits used in this study could miss early HIV infections especially in populations with high HIV incidence such as KPs and PPs where acute infection is more common hence it is possible that some early infections could not be detected. However, by using the oral fluid HIV self-testing kit, we identified and confirmed four HIV positive respondents who were on PrEP.
5. Conclusions
HIV self-testing is highly acceptable and is the most preferred HIV testing approach for routine three monthly follow up testing among KPs and PPs on PrEP in central Uganda. The most preferred models of HIVST kit distribution are self-pick from facility, heath worker distribution and peer distribution. Oral fluid-based HIV self-testing kits should be available at no cost or subsidised to not more than 5,000 Uganda shillings (USD 1.4).
6. Recommendations
We recommend that: HIVST be adopted as a testing approach for all people who may require regular rapid HIV testing due to ongoing risk of exposure on opt-out basis; Adequate pre and post “self-testing” counselling information should be provided to all people who intend to perform self-testing in order to eliminate possible psychological stress arising from performing the procedure. There is need to study linkage to care after HIV self-testing as it was a concern during the qualitative assessment but was not addressed by our study. A multi-model approach to distributing HIV self-testing kits is necessary since there is no single model that well applies to all categories of KPs and PPs on PrEP.
Source of Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors’ Contributions
John Bosco Matovu Junior, Jayne Tusiime Byakika, Roy William Mayega and Sylivia Nalubega: All participated equally in conception of the research project, study design, literature review, data extraction, data analysis, interpretation, and drafting the manuscript. Manuscript review, and edition and validation.
Ethics Approval and Consent to Participate
The Busitema University Faculty of Health Sciences Higher Degrees and Research Committee approved the study as well as the Mbale Regional Referral Hospital Research and Ethics Committee (Ref No. MRRH-REC-IN-COM 024/2018). All respondents provided a written informed consent except two emancipated minors aged 17 years belonging to the adolescent girls and young women category for whom written informed consent was obtained from each of their guardians before enrolment. Clients were free to opt out of the study at any stage they felt like, and one participant did. In order to maintain confidentiality, qualitative data was kept in the audio recorder, and was only accessed by the research team, while all paperwork generated during the interviews was stored in a ziplock opaque bag. No client name was appended on the questionnaire. All those who tested HIV positive on HIVST (5 clients) were linked for further confirmatory testing according to the national HIV testing algorithm and out of the 5 respondents, 4 were confirmed positive and were linked to anti-retroviral therapy (ART) clinic for initiation.
Availability of Data and Materials
The datasets used and/or analysed plus data collection instruments used during the study are available via this link https://doi.org/10.7910/DVN/XLBZXD
Acknowledgement
Lecturers of the Faculty of Health Sciences, Busitema University, the leadership and management of MARPI Mulago and Rakai Health Sciences program, the research assistants and the Program Manager and all staff of the HIV Testing Services unit, Ministry of Health, STD/AIDS control program, Uganda.
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Global HIV & AIDS statistics — Fact sheet (2022).
- Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. Geneva: World Health Organization (2017).
- Technical Guidance on Pre-Exposure Prophylaxis (PrEP) for Persons at High Risk of HIV in Uganda. In: Health, editor. Uganda: Ministry of Health (2016).
- A short technical update on self-testing for HIV. United Nations Program on HIV/AIDS (2014).
- Geng EH, Ortblad K, Kibuuka Musoke D, et al. Direct provision versus facility collection of HIV self-tests among female sex workers in Uganda: A cluster-randomized controlled health systems trial. PLoS medicine 14 (2017): e1002458.
- Nangendo J, Obuku EA, Kawooya I, et al. Diagnostic accuracy and acceptability of rapid HIV oral testing among adults attending an urban public health facility in Kampala, Uganda. PLoS One 12 (2017): e0182050.
- Mugo PM, Micheni M, Shangala J, et al. Uptake and Acceptability of Oral HIV Self-Testing among Community Pharmacy Clients in Kenya: A Feasibility Study. PLoS One 12 (2017): e0170868.
- Kurth AE, Cleland CM, Chhun N, et al. Accuracy and Acceptability of Oral Fluid HIV Self-Testing in a General Adult Population in Kenya. AIDS Behav 20 (2016): 870-879.
- Katz DA, Golden MR, Hughes JP, et al. Acceptability and Ease of Use of Home Self-Testing for HIV among Men Who Have Sex with Men2012; University of Washington.
- Pal K, Ngin C, Tuot S, et al. Acceptability study on HIV self-testing among transgender women, men who have sex with men, and female entertainment workers in Cambodia: A qualitative analysis. PLOS One 11 (2016).
- Figueroa C, Johnson C, Verster A, et al. Attitudes and Acceptability on HIV Self-testing Among Key Populations: A Literature Review. AIDS and Behavior 19 (2015): 1949-1965.
- Ngure K, Heffron R, Mugo N, et al. Feasibility and acceptability of HIV self-testing among pre-exposure prophylaxis users in Kenya. J Int AIDS Soc 20 (2017): 21234.
- Walensky RP, Bassett IV. HIV self-testing and the missing linkage. PLoS Med 8 (2011): e1001101.
- National Guidelines for Research involving Humans as research Participants. National Guidelines for Research involving Humans as research Participants. Kampala: UNCST website (2014): 38.
- John Santelli SH, McGovern T. Inclusion with Protection: Obtaining informed consent. UNICEF Innocenti Research Broef 13 (2017).
- Sarkar A, Mburu G, Shivkumar PV, et al. Feasibility of supervised self-testing using an oral fluid-based HIV rapid testing method: a cross-sectional, mixed method study among pregnant women in rural India. Journal of the International AIDS Society 19 (2016): 20993.
- Weiser SD, Pant Pai N, Sharma J, et al. Supervised and Unsupervised Self-Testing for HIV in High- and Low-Risk Populations: A Systematic Review. PLoS Medicine 10 (2013): e1001414.
- Ng OT, Chow AL, Lee VJ, et al. Accuracy and user-acceptability of HIV self-testing using an oral fluid-based HIV rapid test. PLoS One 7 (2012): e45168.
- Maheswaran H, Petrou S, MacPherson P, et al. Cost and quality of life analysis of HIV self-testing and facility-based HIV testing and counselling in Blantyre, Malawi. BMC Medicine 14 (2016): 34.
- Gaydos CA, Hsieh YH, Harvey L, et al. Will patients "opt in" to perform their own rapid HIV test in the emergency department? Ann Emerg Med 58 (2011): S74-78.