A Subcutaneous Abscess Caused by Candida Krusei Infection: A rare Manifestation
Article Information
Adrita Ashraf1, Mark Bannon1, Matthew Nunley1, Prashant Kaushik2, Creticus Marak3*
1Department of Internal Medicine, House Staff, Northeastern Health System, Tahlequah, UK.
2Department of Medicine, Rheumatology, Northeastern Health System, Tahlequah, UK.
3Department of Medicine, Pulmonary and Critical Care, Northeastern Health System, Tahlequah, UK.
*Corresponding Author: Creticus Marak, Department of Medicine, Pulmonary and Critical Care, Northeastern Health System, Tahlequah, UK
Received: 15 July 2022; Accepted: 29 July 2022; Published: 28 September 2022
Citation: Adrita Ashraf, Mark Bannon, Matthew Nunley, Prashant Kaushik, Creticus Marak. A Subcutaneous Abscess Caused by Candida Krusei Infection: A Rare Manifestation. Archives of Internal Medicine Research 5 (2022): 455-457.
View / Download Pdf Share at FacebookAbstract
Candida is considered a normal microbiota of the gastrointestinal and genitourinary systems with a tendency for an invasive disease if the predisposing conditions exist. Mucocutaneous manifestations of Candida infection include the commonly encountered oropharyngeal thrush, vulvovaginitis, balanitis, intertrigo, paronychia, diaper dermatitis, and the rare chronic mucocutaneous candidiasis. Subcutaneous abscess due to Candida (albicans and non-albicans) is rare, with the literature available only in case reports. We report the first case of a subcutaneous perineal abscess due to C. krusie in a patient with poorly controlled diabetes without immune compromised conditions or a hematologic malignancy.
Keywords
Candida krusei, non-albicans Candida, perineal abscess, immune compromised host, fungal infection
Article Details
Case report
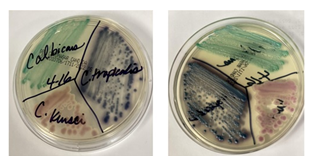
A 48-year-old female with insulin-dependent type 2 diabetes mellitus, hypertension, and hypercholesterolemia was brought to our facility for evaluation of acute encephalopathy. She complained of pain in the perineum of 2 weeks duration. Examination revealed a slightly confused obese female, and the local examination of her perineal region revealed vulvovaginal candidiasis and bilateral perirectal subcutaneous abscesses [Figures 1, 2, 3]. Her initial blood test revealed a sodium level of 144 mEq/L, potassium of 2.6 mEq/L, serum bicarbonate of 7 mEq/L, anion gap of 33, blood glucose of 570 mg/dL, pH 7.14, creatinine of 1.2 mg/dL, beta-hydroxybutyrate of 3.8 mmol/L, white blood cell count of 28.3 K, and A1c 12.9; urinalysis was negative for urinary tract infection. She was diagnosed with diabetic ketoacidosis (DKA), perineal abscesses, and candida vulvovaginitis and admitted to MICU for aggressive management and close monitoring. She was started on the hospital DKA protocol, oral fluconazole, IV vancomycin, and IV Piperacillin tazobactam (Zosyn). Incision and drainage of the bilateral perirectal abscesses was performed without complications. Multiple wound cultures, including anaerobic, grew only Candida krusei [Figures 4, 5], confirming C. krusei subcutaneous abscess. She completed 7 days of empiric therapy with IV vancomycin and IV Zosyn; Fluconazole was discontinued and switched to IV Micafungin. She completed 14 days of IV Micafungin with a good response. Post-discharge outpatient follow-up revealed adequate healing of the perineal wounds.
Introduction
Candida krusei, a non-albicans Candida (NAC) species, is an increasingly encountered fungal pathogen in patients with hematologic malignancies and transplant recipients [1, 2, 3]. Previously reported sites of infection include the bone, joint, vertebra, lung, urine, intraabdominal cavity, pleural space, and blood [4,5,6,7,8,9,10,11,12,13,14,15]. Risk factors include the chronic use of immunosuppressants, hematologic malignancies, chronic hemodialysis, enteric surgery or peritonitis, and previous candidemia [6, 7, 9, 11, 12, 13, 15].
Discussion
Candida albicans is the leading cause of candidiasis. Candida krusei, a NAC species, is a diploid, dimorphic ascomycetous yeast that inhabits mucosa in healthy individuals. It can cause life-threatening infections in patients with immunocompromised conditions or hematologic malignancies [1, 2]. Infections caused by NAC species have been steadily increasing in recent years.
Candidiasis is one of the most common fungal infections in humans with associated high mortality in patients with deep-seated organ infections and fungemia. Infections commonly occur in patients with hematologic malignancies, organ transplant recipients, and those on prolonged azole prophylaxis. Candida krusei, even though isolated less frequently than other Candida species, is typically a multidrug-resistant (MDR) pathogen with higher attributable and crude mortality than C. albicans [1, 2]. The infections caused by this organism are of particular relevance in clinical practice because of its intrinsic resistance to fluconazole and decreased susceptibility to amphotericin B and flucytosine [1, 2, 3].
Mucocutaneous infection by C. krusei is exceedingly rare; vulvovaginitis is probably the most familiar manifestation but is still much rarer than vulvovaginitis caused by the other Candida species [21]. Reports on C. krusei presenting with skin manifestations are scarce; abscess in an intravenous heroin drug abuser and a folliculocentric rash in a patient with AML have previously been reported [22, 24]. Subcutaneous abscess due to other Candida species, even though rare, is probably more common than C. krusei and has been reported with C. albicans and C. tropicalis [17, 18, 19, 29]. Invasive infections due to C. krusei frequently occur in patients with predisposing conditions; cutaneous manifestations are rare. To the best of our knowledge, a subcutaneous abscess with diabetes as the only risk factor has never been reported.
References
- Jamiu AT, Albertyn J, Sebolai OM, Pohl CH. Update on Candida krusei, a potential multidrug-resistant pathogen. Med Mycol. 2021 Jan 4;59(1):14-30. doi: 10.1093/mmy/myaa031. PMID: 32400853.
- Gómez-Gaviria M, Mora-Montes HM. Current Aspects in the Biology, Pathogeny, and Treatment of Candida krusei, a Neglected Fungal Pathogen. Infect Drug Resist. 2020 Jun 10;13:1673-1689. doi: 10.2147/IDR.S247944. PMID: 32606818; PMCID: PMC7293913.
- Pfaller, M. A., Diekema, D. J., Gibbs, D. L., Newell, V. A., Nagy, E., Dobiasova, S., Rinaldi, M., Barton, R., Veselov, A., & Global Antifungal Surveillance Group (2008). Candida krusei, a multidrug-resistant opportunistic fungal pathogen: geographic and temporal trends from the ARTEMIS DISK Antifungal Surveillance Program, 2001 to 2005. J Clin Microbiol. 2008;46(2):515-521. doi:10.1128/JCM.01915-07
- Kaldau NC, Brorson S, Jensen PE, Schultz C, Arpi M. Bilateral polymicrobial osteomyelitis with Candida tropicalis and Candida krusei: a case report and an updated literature review. Int J Infect Dis. 2012 Jan;16(1):e16-22. doi: 10.1016/j.ijid.2011.10.001. Epub 2011 Nov 29. PMID: 22129759.
- Pemán J, Jarque I, Bosch M, Cantón E, Salavert M, de Llanos R, Molina A. Spondylodiscitis caused by Candida krusei: case report and susceptibility patterns. J Clin Microbiol. 2006 May;44(5):1912-4. doi: 10.1128/JCM.44.5.1912-1914.2006. PMID: 16672439; PMCID: PMC1479197.
- Overgaauw AJC, de Leeuw DC, Stoof SP, van Dijk K, Bot JCJ, Hendriks EJ. Case report: Candida krusei spondylitis in an immunocompromised patient. BMC Infect Dis. 2020;20(1):739. Published 2020 Oct 8. doi:10.1186/s12879-020-05451-3
- Multani A, Subramanian AK, Liu AY. Successful eradication of chronic symptomatic Candida krusei urinary tract infection with increased dose micafungin in a liver and kidney transplant recipient: Case report and review of the literature. Transpl Infect Dis. 2019 Aug;21(4):e13118. doi: 10.1111/tid.13118. Epub 2019 Jun 3. PMID: 31111613.
- Lu H, Marengo MF, Mihu CN, Garcia-Manero G, Suarez-Almazor ME. Rare case of septic arthritis caused by Candida krusei: case report and literature review. J Rheumatol. 2012 Jun;39(6):1308-9. doi: 10.3899/jrheum.111348. PMID: 22661427.
- Imtiaz T, Thomson F, Innes A, du Toit FC, Bal AM. Candida krusei bronchopneumonia with nodular infiltrates in a patient with chronic renal failure on haemodialysis--case report and review of literature. Mycoses. 2011 Sep;54(5):e611-4. doi: 10.1111/j.1439-0507.2010.01925.x. Epub 2010 Jul 18. PMID: 20809925.
- Jud P, Valentin T, Regauer S, Gary T, Hackl G, Rief P, Brodmann M, Hafner F. Invasive Candida krusei infection and Candida vasculitis of a leg ulcer in an immunocompetent patient: A case report. Int J Infect Dis. 2017 Feb;55:96-98. doi: 10.1016/j.ijid.2017.01.010. Epub 2017 Jan 16. PMID: 28104503.
- Krcmery V Jr, Spanik S, Kunova A, Trupl J, Grausova S, Krupova I, Mateicka F, Pichnova E, Grey E, Sabo A. Nosocomial Candida krusei fungemia in cancer patients: report of 10 cases and review. J Chemother. 1999 Apr;11(2):131-6. doi: 10.1179/joc.1999.11.2.131. PMID: 10326744.
- Mori T, Inamori K, Matsumura M, Oguri T, Oshimi K. A case of fungemia due to Candida krusei. Nihon Ishinkin Gakkai Zasshi. 1999;40(1):15-20. doi: 10.3314/jjmm.40.15. PMID: 9929577.
- Cascio A, Bartolotta M, Venneri A, Musolino C, Iaria C, Delfino D, Navarra G. A case of Candida krusei peritonitis secondary to duodenal perforation due to Candida duodenitis. Mycopathologia. 2011 Jan;171(1):51-5. doi: 10.1007/s11046-010-9344-z. Epub 2010 Jul 15. PMID: 20632210.
- Tan M, Wang J, Hu P, Wang B, Xu W, Chen J. Severe pneumonia due to infection with Candida krusei in a case of suspected Middle East respiratory syndrome: A case report and literature review. Exp Ther Med. 2016 Dec;12(6):4085-4088. doi: 10.3892/etm.2016.3892. Epub 2016 Nov 11. PMID: 28101187; PMCID: PMC5228306.
- Imtiaz T, Thomson F, Innes A, du Toit FC, Bal AM. Candida krusei bronchopneumonia with nodular infiltrates in a patient with chronic renal failure on haemodialysis--case report and review of literature. Mycoses. 2011 Sep;54(5):e611-4. doi: 10.1111/j.1439-0507.2010.01925.x. Epub 2010 Jul 18. PMID: 20809925.
- Gordon RA, Simmons BP, Appelbaum PC, Aber RC. Intra-abdominal abscess and fungemia caused by candida krusei. Arch Intern Med. 1980 Sep;140(9):1239-40. PMID: 7406623.
- Wai PH, Ewing CA, Johnson LB, Lu AD, Attinger C, Kuo PC. Candida fasciitis following renal transplantation. Transplantation. 2001 Aug 15;72(3):477-9. doi: 10.1097/00007890-200108150-00019. PMID: 11502978.
- Benson PM, Roth RR, Hicks CB. Nodular subcutaneous abscesses caused by Candida tropicalis. J Am Acad Dermatol. 1987 Mar;16(3 Pt 1):623-4. doi: 10.1016/s0190-9622(87)80103-2. PMID: 3469231.
- Tuon FF, Nicodemo AC. Candida albicans skin abscess. Rev Inst Med Trop Sao Paulo. 2006 Sep-Oct;48(5):301-2. doi: 10.1590/s0036-46652006000500012. PMID: 17086322.
- Marcelo Corti, Maria F Villafa, Fernando Messina and Ricardo Negroni. Subcutaneous Abscess as a Single Manifestation of Candidiasis. Medical Mycology, December 05, 2015.
- Singh S, Sobel JD, Bhargava P, Boikov D, Vazquez JA. Vaginitis due to Candida krusei: epidemiology, clinical aspects, and therapy. Clin Infect Dis. 2002 Nov 1;35(9):1066-70. doi: 10.1086/343826. Epub 2002 Oct 10. PMID: 12384840.
- Jiang, Kecheng MD; Jones, Philbert MD; Shekar, Raja MD. Severe Soft Tissue Abscess Caused by Candida krusei. Infectious Diseases in Clinical Practice: May 2006 - Volume 14 - Issue 3 - p 166-167
- Gordon RA, Simmons BP, Appelbaum PC, Aber RC. Intra-abdominal abscess and fungemia caused by candida krusei. Arch Intern Med. 1980 Sep;140(9):1239-40. PMID: 7406623.
- Qi J, Jourabchi N, Balagula Y, Sheu M, Fischer MK. Folliculocentric cutaneous presentation of disseminated Candida krusei infection in a patient with acute myeloid leukemia. Dermatol Online J. 2015 Nov 18;21(11):13030/qt52j7w4g1. PMID: 26632935.