A Splendid Pelvic Tumor, Indeed
Article Information
Zilberman DE1, Waldman D2*, Raviv-Zilka L3*, Fridman E4, Ben-Shlush A3*, Mor Y1*
1Departments of Urology, The Chaim Sheba Medical Center and Edmond and Lily Safra Children's Hospital, Tel-Hashomer, Ramat-Gan, Affiliated to Sackler School of Medicine, Tel-Aviv University, Israel
2Pathology, The Chaim Sheba Medical Center and Edmond and Lily Safra Children's Hospital, Tel-Hashomer, Ramat-Gan, Affiliated to Sackler School of Medicine, Tel-Aviv University, Israel
3Pediatric Hemato-Oncology, The Chaim Sheba Medical Center and Edmond and Lily Safra Children's Hospital, Tel-Hashomer, Ramat-Gan, Affiliated to Sackler School of Medicine, Tel-Aviv University, Israel
4Unit of Pediatric Imaging, The Chaim Sheba Medical Center and Edmond and Lily Safra Children's Hospital, Tel-Hashomer, Ramat-Gan, Affiliated to Sackler School of Medicine, Tel-Aviv University, Israel
*Corresponding Author: Prof. Yoram Mor, Departments of Urology, The Chaim Sheba Medical Center and Edmond and Lily Safra Children's Hospital, Tel-Hashomer, Ramat-Gan, Affiliated to Sackler School of Medicine, Tel-Aviv University, Israel
Received: 27 May 2020; Accepted: 18 June 2020; Published: 02 July 2020
Citation: Zilberman DE, Waldman D, Raviv-Zilka L, Fridman E, Ben-Shlush A, Mor Y. A Splendid Pelvic Tumor, Indeed. Archives of Nephrology and Urology 3 (2020): 046-048.
View / Download Pdf Share at FacebookAbstract
Accessory spleen is not a common finding, usually located nearby the normal anatomic location of the spleen, oftentimes in the splenic hilum, the great omentum and the pancreas. Pelvic accessory spleen is a very rare finding, mostly asymptomatic and incidentally radiologically detected. Herein, we present an 18 years old male who underwent an investigation for daytime urinary frequency and suspicious small right pelvic mass was demonstrated by both ultrasound and MRI scans. In view of being a potentially malignant tumor, a robotic-assisted removal was uneventfully performed and the final pathology was surprisingly compatible with an accessory spleen.
Keywords
Accessory spleen; Pelvis; Pelvic accessory spleen
Accessory spleen articles, Pelvis articles, Pelvic accessory spleen articles
Accessory spleen articles Accessory spleen Research articles Accessory spleen review articles Accessory spleen PubMed articles Accessory spleen PubMed Central articles Accessory spleen 2023 articles Accessory spleen 2024 articles Accessory spleen Scopus articles Accessory spleen impact factor journals Accessory spleen Scopus journals Accessory spleen PubMed journals Accessory spleen medical journals Accessory spleen free journals Accessory spleen best journals Accessory spleen top journals Accessory spleen free medical journals Accessory spleen famous journals Accessory spleen Google Scholar indexed journals Pelvis articles Pelvis Research articles Pelvis review articles Pelvis PubMed articles Pelvis PubMed Central articles Pelvis 2023 articles Pelvis 2024 articles Pelvis Scopus articles Pelvis impact factor journals Pelvis Scopus journals Pelvis PubMed journals Pelvis medical journals Pelvis free journals Pelvis best journals Pelvis top journals Pelvis free medical journals Pelvis famous journals Pelvis Google Scholar indexed journals Pelvic accessory spleen articles Pelvic accessory spleen Research articles Pelvic accessory spleen review articles Pelvic accessory spleen PubMed articles Pelvic accessory spleen PubMed Central articles Pelvic accessory spleen 2023 articles Pelvic accessory spleen 2024 articles Pelvic accessory spleen Scopus articles Pelvic accessory spleen impact factor journals Pelvic accessory spleen Scopus journals Pelvic accessory spleen PubMed journals Pelvic accessory spleen medical journals Pelvic accessory spleen free journals Pelvic accessory spleen best journals Pelvic accessory spleen top journals Pelvic accessory spleen free medical journals Pelvic accessory spleen famous journals Pelvic accessory spleen Google Scholar indexed journals Bladder articles Bladder Research articles Bladder review articles Bladder PubMed articles Bladder PubMed Central articles Bladder 2023 articles Bladder 2024 articles Bladder Scopus articles Bladder impact factor journals Bladder Scopus journals Bladder PubMed journals Bladder medical journals Bladder free journals Bladder best journals Bladder top journals Bladder free medical journals Bladder famous journals Bladder Google Scholar indexed journals tumor articles tumor Research articles tumor review articles tumor PubMed articles tumor PubMed Central articles tumor 2023 articles tumor 2024 articles tumor Scopus articles tumor impact factor journals tumor Scopus journals tumor PubMed journals tumor medical journals tumor free journals tumor best journals tumor top journals tumor free medical journals tumor famous journals tumor Google Scholar indexed journals Computerized Tomography articles Computerized Tomography Research articles Computerized Tomography review articles Computerized Tomography PubMed articles Computerized Tomography PubMed Central articles Computerized Tomography 2023 articles Computerized Tomography 2024 articles Computerized Tomography Scopus articles Computerized Tomography impact factor journals Computerized Tomography Scopus journals Computerized Tomography PubMed journals Computerized Tomography medical journals Computerized Tomography free journals Computerized Tomography best journals Computerized Tomography top journals Computerized Tomography free medical journals Computerized Tomography famous journals Computerized Tomography Google Scholar indexed journals MRI Scan articles MRI Scan Research articles MRI Scan review articles MRI Scan PubMed articles MRI Scan PubMed Central articles MRI Scan 2023 articles MRI Scan 2024 articles MRI Scan Scopus articles MRI Scan impact factor journals MRI Scan Scopus journals MRI Scan PubMed journals MRI Scan medical journals MRI Scan free journals MRI Scan best journals MRI Scan top journals MRI Scan free medical journals MRI Scan famous journals MRI Scan Google Scholar indexed journals
Article Details
1. Case Report
An 18 years old generally healthy male presented with daytime urinary frequency. Physical examination and urinalysis were unremarkable. Abdominal ultrasound (US) demonstrated a solid lesion, 3 cm in diameter, adjacent to the Rt. Bladder wall. Magnetic resonance imaging (MRI) (Figure 1) demonstrated a similar finding, namely, a solid homogenous enhancing mass on T1 weighted images after injection of Gadolinium (26 × 18 mm), pressuring the upper-lateral aspect of the urinary bladder. In view of a potentially malignant tumor, a robotic-assisted removal of the tumor was uneventfully performed. The final pathology was compatible with an accessory spleen showing reactive lymphoid follicular hyperplasia (Figure 2). A repeat US, obtained 6 months postoperatively showed disappearance of the finding, and the patient remained well at 6-months follow-up visit.
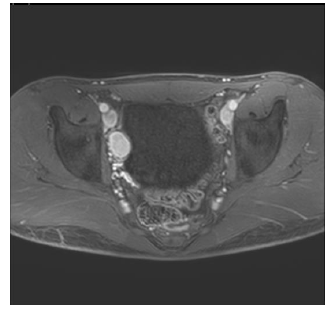
Figure 1: Abdominal MRI showing a solid homogenous enhancing mass (26 × 18 mm), on T1 weighted images after injection of Gadolinium, pressuring the upper-lateral aspect of the urinary bladder.
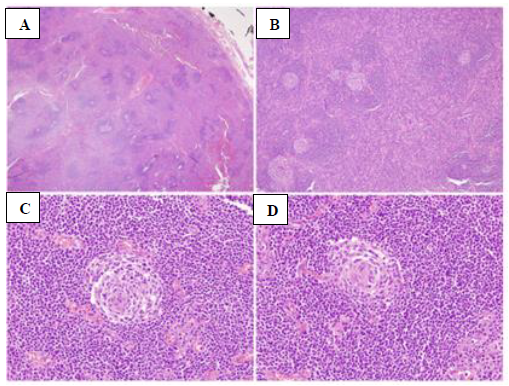
Figures 2: A - H&E x 2 Normal splenic tissue surrounded by splenic capsule; B - H&E x 4 – Splenic tissue with reactive lymphoid follicles; C, D - H&E x 40 - Central arteriole in a reactive lymphoid follicle.
2. Discussion
Ectopic splenic tissue can be encountered either due to auto-transplantation of cells following abdominal trauma or splenectomy (splenosis), or as a congenital malformation (accessory spleen) [1]. Accessory spleens were reported in 6.7% of autopsies, mainly in the splenic hilum, the great omentum and the pancreas [2]. However, pelvic accessory spleen is a very rare finding, mostly asymptomatic and incidentally radiologically detected, though it may cause acute abdominal pain, abdominal discomfort, or dysmenorrhea [3-4]. It can be well visualized by either Computerized Tomography (CT) scans, MRI which often shows a vascular pedicle originating from the great omentum or from the splenic hilum, as well as scintigraphy with Tc-99m-labeled colloids which localize in the reticuloendothelial cells of the liver and spleen [5]. Yet, as it mimics a primary tumor or a metastatic lymph node, it is usually removed to avoid concern.
Conflicts of Interest
The authors declare that they have no competing interests.
Financial Disclosure
The authors have no proprietary or commercial interests.
References
- Taskin MI, Baser BG, Adali E, et al. Accessory spleen in the pelvis: A case report. Int. J. Surg Case Rep 12 (2015): 23-25.
- Tendler R., Farah RK, Kais M, et al. Symptomatic pelvic accessory spleen in a female adolescent: Case report. J. Clin. Ultrasound 45 (2007): 600-602.
- Ota H, Ojima Y, Sumitani D, et al. Dynamic computed tomography findings of an accessory spleen in the pelvis: a case report. Surg. Case Rep 2 (2016): 2016.
- Zhou JS, Chen X, Zhu T, et al. Pelvic accessory spleen caused dysmenorrhea. Taiwan J. Obstet. Gynecol 54 (2015): 445-446.
- Iorio F, Frantellizzi V, Drudi FM, et al. Locally vascularized pelvic accessory spleen. J. Ultrasound 19 (2016): 141-144.
