A Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol for Labour Analgesia
Article Information
Neha Garg*, Vanitha VG
Department of Obstetrics and Gynaecology, JJM Medical College, Davangere, Karnataka, India
*Corresponding Author: Neha Garg, Department of Obstetrics and Gynaecology, JJM Medical College, Davangere,Karnataka, India - 577 004
Received: 23 April 2019; Accepted: 07 May 2019; Published: 10 May 2019
Citation:
Neha Garg, Vanitha VG. A Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol for Labour Analgesia. Obstetrics and Gynecology Research 2 (2019): 003-013.
View / Download Pdf Share at FacebookAbstract
Background: Labour pain described as ‘the most horrible’ affects both physiological and psychological aspects of labour. Thus, the provision of labour analgesia is of paramount importance to better both maternal and neonatal outcomes. In our country, majority of obstetric services are in the hands of trained nurses and non-specialized doctors and thus awareness and acceptance of pain-relieving for women in labour virtually does not exist. Therefore, drugs like paracetamol and tramadol with advantage of easy availability, being inexpensive with no special technique of administration are a boon for labour analgesia.
Objective: To compare the role of intravenous paracetamol versus intravenous tramadol as an intrapartum labour
analgesic.
Materials and methods: A total of 273 primigravidae with term gestation with singleton pregnancy with vertex presentation in active phase of labour with cervical dilatation ≥ 4cm with spontaneous onset of labour were taken who satisfied the inclusion and exclusion criteria of the study. Group P (141 women) and Group T (132 women) received 100 ml intravenous infusion containing 1 gram of paracetamol single dose and 100 mg of tramadol hydrochloride diluted in 100 ml normal saline over 15 minutes respectively. Visual Analogue scale (VAS) was used to assess pain intensity, before administering drug, after 1 and 3 hours of drug administration. The primary outcomes measured were difference in VAS score in both groups. The secondary outcomes analysed were mode of delivery, duration of labour, drug-delivery interval, maternal side effects and neonatal outcomes in terms of birth weight, APGAR scores and NICU admissions.
Results: The mean VAS score decreased significantly to a greater extent in group P than group T and showed a significant statistical difference among both the groups (p < 0.001). In both
Keywords
Labour analgesia; Intravenous; Paracetamol; Tramadol; VAS; APGAR
Labour analgesia articles Labour analgesia Research articles Labour analgesia review articles Labour analgesia PubMed articles Labour analgesia PubMed Central articles Labour analgesia 2023 articles Labour analgesia 2024 articles Labour analgesia Scopus articles Labour analgesia impact factor journals Labour analgesia Scopus journals Labour analgesia PubMed journals Labour analgesia medical journals Labour analgesia free journals Labour analgesia best journals Labour analgesia top journals Labour analgesia free medical journals Labour analgesia famous journals Labour analgesia Google Scholar indexed journals Intravenous articles Intravenous Research articles Intravenous review articles Intravenous PubMed articles Intravenous PubMed Central articles Intravenous 2023 articles Intravenous 2024 articles Intravenous Scopus articles Intravenous impact factor journals Intravenous Scopus journals Intravenous PubMed journals Intravenous medical journals Intravenous free journals Intravenous best journals Intravenous top journals Intravenous free medical journals Intravenous famous journals Intravenous Google Scholar indexed journals Paracetamol articles Paracetamol Research articles Paracetamol review articles Paracetamol PubMed articles Paracetamol PubMed Central articles Paracetamol 2023 articles Paracetamol 2024 articles Paracetamol Scopus articles Paracetamol impact factor journals Paracetamol Scopus journals Paracetamol PubMed journals Paracetamol medical journals Paracetamol free journals Paracetamol best journals Paracetamol top journals Paracetamol free medical journals Paracetamol famous journals Paracetamol Google Scholar indexed journals Tramadol articles Tramadol Research articles Tramadol review articles Tramadol PubMed articles Tramadol PubMed Central articles Tramadol 2023 articles Tramadol 2024 articles Tramadol Scopus articles Tramadol impact factor journals Tramadol Scopus journals Tramadol PubMed journals Tramadol medical journals Tramadol free journals Tramadol best journals Tramadol top journals Tramadol free medical journals Tramadol famous journals Tramadol Google Scholar indexed journals VAS articles VAS Research articles VAS review articles VAS PubMed articles VAS PubMed Central articles VAS 2023 articles VAS 2024 articles VAS Scopus articles VAS impact factor journals VAS Scopus journals VAS PubMed journals VAS medical journals VAS free journals VAS best journals VAS top journals VAS free medical journals VAS famous journals VAS Google Scholar indexed journals APGAR articles APGAR Research articles APGAR review articles APGAR PubMed articles APGAR PubMed Central articles APGAR 2023 articles APGAR 2024 articles APGAR Scopus articles APGAR impact factor journals APGAR Scopus journals APGAR PubMed journals APGAR medical journals APGAR free journals APGAR best journals APGAR top journals APGAR free medical journals APGAR famous journals APGAR Google Scholar indexed journals Labour pain articles Labour pain Research articles Labour pain review articles Labour pain PubMed articles Labour pain PubMed Central articles Labour pain 2023 articles Labour pain 2024 articles Labour pain Scopus articles Labour pain impact factor journals Labour pain Scopus journals Labour pain PubMed journals Labour pain medical journals Labour pain free journals Labour pain best journals Labour pain top journals Labour pain free medical journals Labour pain famous journals Labour pain Google Scholar indexed journals women articles women Research articles women review articles women PubMed articles women PubMed Central articles women 2023 articles women 2024 articles women Scopus articles women impact factor journals women Scopus journals women PubMed journals women medical journals women free journals women best journals women top journals women free medical journals women famous journals women Google Scholar indexed journals child birth articles child birth Research articles child birth review articles child birth PubMed articles child birth PubMed Central articles child birth 2023 articles child birth 2024 articles child birth Scopus articles child birth impact factor journals child birth Scopus journals child birth PubMed journals child birth medical journals child birth free journals child birth best journals child birth top journals child birth free medical journals child birth famous journals child birth Google Scholar indexed journals gestation articles gestation Research articles gestation review articles gestation PubMed articles gestation PubMed Central articles gestation 2023 articles gestation 2024 articles gestation Scopus articles gestation impact factor journals gestation Scopus journals gestation PubMed journals gestation medical journals gestation free journals gestation best journals gestation top journals gestation free medical journals gestation famous journals gestation Google Scholar indexed journals
Article Details
1. Introduction
Labour is the series of events that take place in the genital organs in an effort to expel the viable products of conception (fetus, placenta, and membranes) out of the womb through the vagina into the outside world. It is characterized by regular painful uterine contractions which increase in frequency and intensity. Labour pain has been described as the most agonizing, more than what human nature would be able to bear under any circumstance and ranked high on the pain rating scale when compared to other painful life experiences [1]. The experience of labour is subjective and complex. It is a highly individual response to variable stimuli that are uniquely received and interpreted. These stimuli are modified by emotional, motivational, cognitive, social, and cultural circumstances.
From time immemorial there has been this false belief that ‘pain is the mother’s safety and its absence her destruction; that it was the will of god and in someway beneficial to the sufferer and labour progress was related to degree of pain. From those days to the use of ether and chloroform to pregnant women to the present-day practice of evidence based comprehensive program of labour pain management; the field of obstetric analgesia and anaesthesia have trod a long journey. Currently myriad of options are available for pain relief such as acupuncture, transcutaneous electrical nerve stimulation (TENS), hypnosis, psychoprophylaxis, usage of massaging, heating pads and water immersion, inhalational agents like Entonox, parenteral opioids like pethidine, fentanyl, remifentanil and morphine. Modern neuraxial labour analgesia reflects a shift from just pain relief to an overall quality of analgesia, is now the gold standard and frequently being practiced in the developed countries [2].
Labour pain causes apprehension, stress, anxiety and adversely affects both the course of labour and fetal outcome. The associated sympathetic stimulation leads to maternal hyperventilation, increased oxygen consumption, respiratory alkalosis, excessive release of catecholamines and cortisol, uterine vasoconstriction, decrease in placental blood flow and resultant reduced oxygen transfer to fetus and fetal metabolic acidosis. Thus, pain relief during labour will improve maternal and perinatal outcome.
In our country majority of obstetric services are in the hands of trained nurses and non-specialized doctors and thus awareness and acceptance of pain-relieving for women in labour virtually does not exist. Antenatal education regarding labour, labour pain, birth experience expectations, analgesia options and concerns goes a long way in building a healthy patient- doctor relationship and these women being aware of such facilities and opting for the same. Also, most modern obstetric analgesic practices require costly equipment, continuous monitoring facilities, and expert anaesthesiologists which is scarcely available if at all in a developing country like India. Therefore, drugs like paracetamol and tramadol with advantage
of easy availability, being inexpensive with no special technique of administration are a boon for labour analgesia.
2. Objective
To compare the role of intravenous paracetamol vs intravenous tramadol as an intrapartum labour analgesic.
Primary objective – To measure the difference in VAS score in both groups before administration of drug, 1 hour and 3 hours after administration of respective drugs.
Secondary objective – To analyze the mode of delivery, duration of labour, drug-delivery interval, maternal side effects and neonatal outcomes in terms of birth weight, APGAR scores and NICU admissions
3. Materials and Methods
Health care setup – Tertiary care hospital
Setting – JJM Medical College, Davangere, Karnataka.
Duration of the study – Oct 2017 to Sep 2018 (12 months) Type of the study – Randomized controlled trial
Sample size – 273
Level of evidence – Level II
Selection of cases – 273 primigravidae were taken who satisfied the inclusion and exclusion criteria of the study.
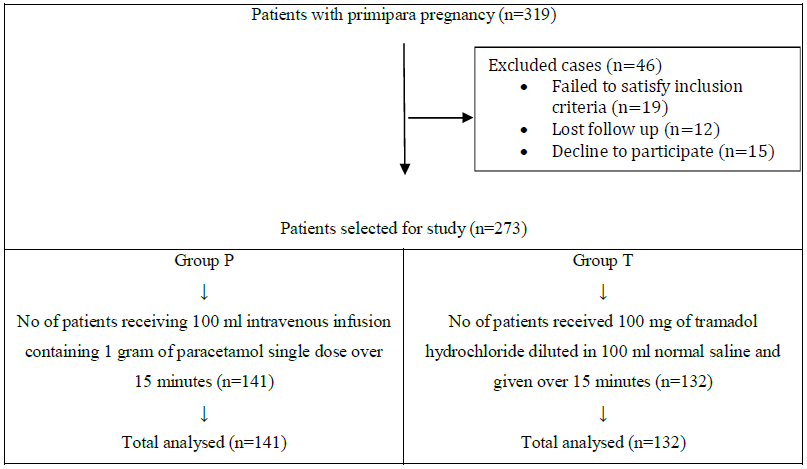
Figure 1: Patient’s selection
Inclusion criteria
- Primigravidae in active phase of labour; cervical dilatation ≥ 4cm, cervical effacement ≥60% with good uterine contractions (3-4 contractions in 10 minutes, each lasting for 45 seconds)
- Term gestation; period of gestation ≥ 37 weeks
- Spontaneous onset of labour.
- Singleton pregnancy with vertex presentation
Exclusion criteria
- Women with clinical evidence of cephalopelvic disproportion
- Malpresentation
- Multiple pregnancy
- Previously scarred uterus (post myomectomy, post cesarean)
- Preterm labour
- Induced labour
- Antepartum haemorrhage
- Pregnancy induced hypertension
- History of drug allergy
- History of medical disorders
- Fetal distress
- Intrauterine foetal death
- Patients who refused participation as per our protocol
After getting informed written consent from the patients enrolled in our study, they were subjected for thorough examination for fulfilment of all the inclusion criteria. The randomization was done by coin-tossing method into two groups as Paracetamol group (Group P): 141 women received 100 ml intravenous infusion containing 1 gram of paracetamol single dose over 15 minutes and Tramadol group (Group T): 132 women received 100 mg of tramadol hydrochloride diluted in 100 ml normal saline and given over 15 minutes.
Visual Analogue scale (VAS) was used to assess pain intensity. VAS score was further divided as 0: no pain, 0.1 - 3.9: mild pain, 4 - 6.9 : moderate pain and 7 – 10 : severe pain. The pain intensity before administering drug was recorded. The follow up was done with the subjective measurement of pain relief after 1 and 3 hours of drug administration. Labour was monitored using a WHO modified partogram. The primary outcome measured were the difference in VAS score in both groups before administration of drug, 1 hour and 3 hours after administration of respective drugs. The secondary outcomes analysed were mode of delivery, duration of labour, drug-delivery interval, maternal side effects (mothers were monitored for 24 hours after delivery for any side-effects) and neonatal outcomes in terms of birth weight, APGAR scores and NICU admissions.
3. Results
A total of 273 cases were enrolled in the study who were divided into two groups as group P & group T and considered for statistical analysis. The descriptive statistics were reported as mean (SD) for continuous variables, frequencies (percentage) for categorical variables. Data were statistically evaluated with IBM SPSS Statistics for Windows, Version 20.0, IBM Corp, Chicago, IL.
A) Demographic statistics
The age group in the present study ranged from 18 – 35 years in both the groups with the mean in group P being 24.71 ± 3.62 years and 23.18 ± 2.37 years in group T. The difference was statistically insignificant (p= 0.139) (as shown in Table 1).
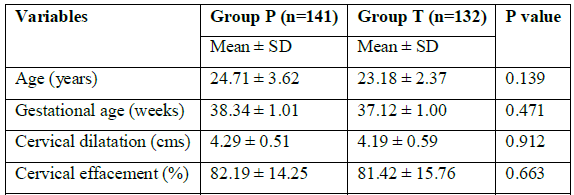
Table 1: Demographic statistics
The mean gestational age in group P was 38.34 ± 1.01 weeks and in group T was 37.12 ± 1.00 weeks. The difference was not statistically significant between the two groups (p= 0.471). (Table 1)
The mean cervical dilatation and effacement at enrolment in group P were 4.29 ± 0.51cm, and 82.19 ± 14.25% respectively and in group T were 4.19 ± 0.59cm, and 81.42 ± 15.76% respectively; with no statistically significant difference (p= 0.912, p=0.663) (Table 1)
B) Mean VAS score at different intervals
In group P, the mean VAS score decreased significantly from 9.1 before drug administration to 6.7 after 1 hour of drug administration and 3.2 after 3 hours. On the other hand, with group T, the mean VAS score decreased from 9.2 before drug administration to 7.2 after 1 hour of drug administration and to 4.7 after 3 hours. Thus, with Paracetamol pain reduced to a greater extent than with tramadol. The difference was statistically significant (as shown in Table 2).
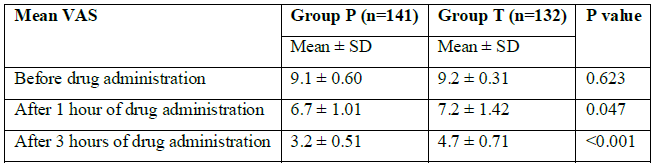
Table 2: Mean VAS score at different intervals
Pain intensity by VAS Before drug administration
In group P, 56% of women had severe pain, 35.5% had moderate pain, 8.5% had mild pain and none had no pain. In group T, 63.6% had severe pain, 36.4% had moderate pain, and none had mild or no pain. The difference in VAS score in both groups was not statistically significant (p=0.6912) (as shown in Table 3).
After 1 hour of drug administration
In group P, 32.6% had severe pain, 49% had moderate pain, 18.4% had mild pain and none had no pain. In group T, 56.8% had severe pain, 33.3% had moderate pain, 9.9% had mild pain and none had no pain. The difference was statistically significant (p=0.0031) (as shown in Table 3).
After 3 hours of drug administration
In group P, 24.1% had severe pain, 51.8% had moderate pain, 19.1% had mild pain and 5% had no pain at all. In group T, 48.5% had severe pain, 38.6% had moderate pain, 12.1% had mild pain and 0.8% had no pain at all. The difference in the VAS score was statistically significant (p<0.0001) (as shown in Table 3).
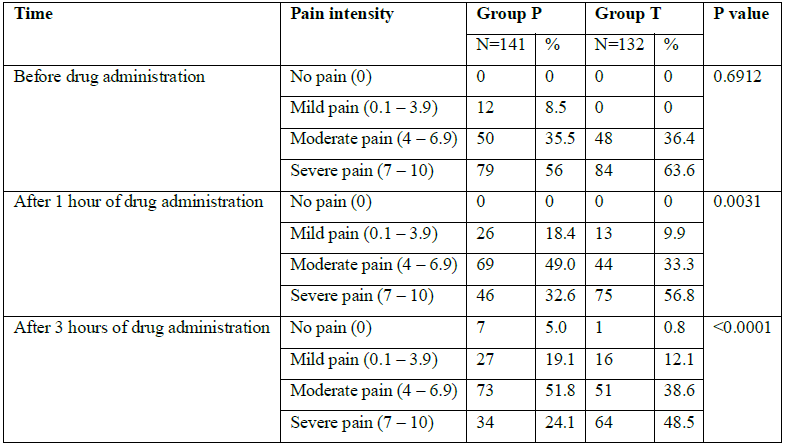
Table 3: Pain intensity by VAS
D) Mode of Delivery
In group P, 77.31 % women had spontaneous vaginal delivery, 16.80 % had instrumental delivery and 5.88 % underwent caesarean section. In group T, 73.71 % had spontaneous vaginal delivery, 13.39 % had instrumental delivery and 12.89 % had delivery by caesarean section. The difference in mode of delivery between both the groups was not statistically significant.
E) Mean duration of labour
The mean duration of active phase of first stage of labour with group P was 228 ± 53.41 mins and with group T was 293 ± 58.13 mins. The difference in mean duration of active phase of first stage of labour was statistically significant (p<0.0001). The mean duration of second stage of labour with group P was 36 ± 12.01 mins and in group T was 49 ± 11.41 minutes. The difference was statistically significant (p=0.0041). The mean duration of third stage of labour in group P was 8 ± 1.41 mins and with group T was 7 ± 2.19 mins. The difference in mean duration of third stage of labour was not statistically significant (p=1.9213). From enrolment in study to delivery; the total duration of labour in group P was 270 ± 58.43 minutes and in group T was 349 ± 64.73 mins. The difference between the two groups was statistically significant (p<0.0001) (as shown in Table 4).
The drug-delivery interval in group P was 262 ± 56.41 minutes and in group T was 342 ± 63.14 minutes. The difference between the two groups was statistically significant (p<0.0001) (as shown in Table 4).
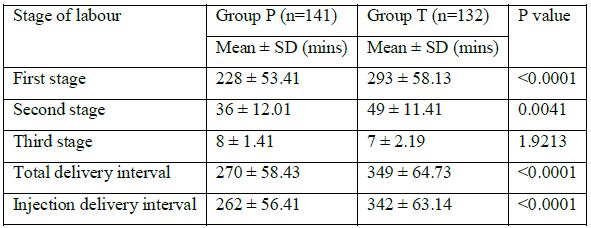
Table 4: Mean duration of labour
F) Birth weight
The majority of the babies born had birth weight between 2.5 kg to 3.5 kg; 73.21% in group P and 69.36% in group T. The mean birth weight in group P was 2.61 ± 0.29 kg and in group T was 2.69 ± 0.33 kg and the difference between them was not statistically significant (p= 0.825).
G) Mean APGAR score
Apgar score readings at 1 minute were 7, 8, 9 in 93.12 % of babies in group P and 86.52 % of babies in group T. At 5 minutes Apgar score readings of 7, 8, 9 were seen in 95.31 % in group P and in 91.73 % in group T. The mean Apgar scores at 1 min and 5 mins in paracetamol group were 7.62 ± 0.79 and 8.91 ± 0.86 respectively. Whereas in tramadol group neonates had Apgar scores at 1 min and 5 minutes of 7.64 ± 0.81 and 8.69 ± 0.69 respectively. The difference was statistically insignificant (p=0.8734, 0.3124) (as shown in Table 5). There was 7 NICU admission of a neonate in group T.
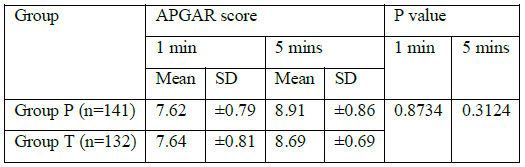
Table 5: Mean APGAR score
H) Maternal complications
In group P, 3.5% of cases had post-partum haemorrhage (PPH), 9.2% had vomiting, 7.1% had nausea as side-effects. In group T, 3.8% had PPH, 17.4% had vomiting and 4.6% had nausea. Vomiting was the most common side effect seen in group T followed by nausea seen in group P (as showed in Graph 1).
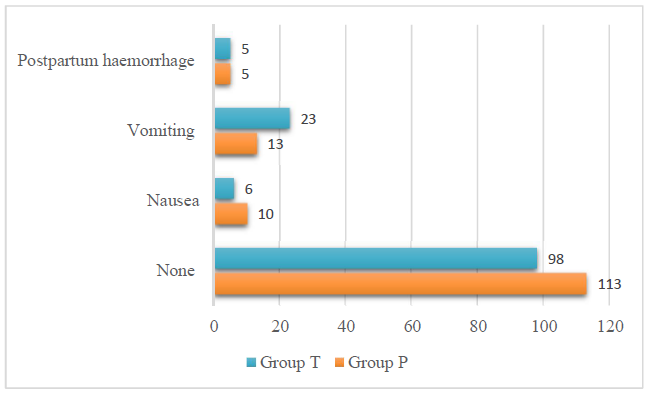
Graph 1: Maternal complications
5. Discussion
Paracetamol (acetaminophen) is now the most commonly used drug worldwide, available over the counter, used in almost all age groups as first line treatment for pain and pyrexia and forms step one of WHO analgesic ladder [3]. The exact mechanism of action is not fully elucidated. A number of central mechanisms including effects on prostaglandin production, and on serotonergic, opioid, nitric oxide, and cannabinoid pathways and a combination of interrelated pathways are involved [3]. It is centrally acting inhibitor of COX and/ or serotonergic system thus inhibiting prostaglandin synthesis. Various studies have shown the effectiveness and safety of intravenous paracetamol as an analgesic agent in varied spectrum of clinical conditions such as musculoskeletal pain, tension type headaches, migraines and across variety of surgical procedures [4-6]. It is inexpensive, easy to administer, requires no special monitoring, have useful opioid-sparing effects with minimal side-effects.
Tramadol hydrochloride (synthetic analogue of codeine) has a unique pharmacological profile. It combines the mechanism of action of opioids and tricyclic antidepressants. It is a weak µ-opioid receptor agonist and inhibits transmission of pain impulses and alters pain perception. Also, it reduces the reuptake of norepinephrine and serotonin in the descending spinal inhibitory system and thereby enhancing the effectiveness of the inhibitory pathway. It causes less maternal and foetal respiratory and cardiovascular depression common to other opioids [7,8]. It is shown to be effective, well tolerated and forms Step 2 in WHO ladder in treating several painful conditions where treatment with strong opioids is not required [9]. Its use as an obstetric analgesic has been widely studied in both intramuscular (7) and intravenous preparations [8,10]. Along with the ease of its administration it is considered as a good alternative to epidural analgesia in rural Indian setup with less resources [10].
Our study is one of a kind to compare intravenous paracetamol with intravenous tramadol for labour analgesia. It was found that in Paracetamol group, there was significant decrease in pain intensity after 1 and 3 hours of drug administration than with Tramadol. There was no difference in pain intensity before drug administration. After 1 hour of drug administration VAS score reached lower values in both groups; which after 3 hours significantly declined further in paracetamol group to a greater extent than in tramadol group. 5% in paracetamol group reported to have no pain at all as compared to 0.8% in tramadol group after 3 hours of drug administration This can be explained by the fact that onset of analgesia after IV paracetamol occurs within 5 min, peaking at 40-60 min, and lasting 4-6 hours [11] while for tramadol, onset is within 10 min, and action lasts for 2-3 hours. Our results were similar to various other studies which compared the efficacy of intravenous paracetamol with intramuscular tramadol as a labour analgesic. In 2015, Hema Mohan et al. [12] and Meenakshi Lallar et al. [13] demonstrated that intravenous paracetamol is a more effective labour analgesic than intramuscular tramadol. Kaur Makkar J et al. [14] concluded intravenous paracetamol provides comparable analgesia as intramuscular tramadol during active labour. In 2016, Bishnu Prasad Das et al. [15] also showed the effectiveness of intravenous paracetamol as a better labour analgesic. Also, tramadol in comparison with standard obstetric analgesic pethidine [16] seems to cause a shorter duration of labour and lower incidence of maternal side-effects. However, its analgesic efficacy was not as effective as pethidine in second stage of labour whereas in first stage both provided moderate analgesia. On the other hand, Paracetamol when compared to pethidine was found to be better intrapartum labour analgesic. [17,18]. Thus, on the whole concluding that paracetamol has better efficacy than tramadol.
Total duration of labour in paracetamol group was found to be significantly shorter than in tramadol group which further can have multiple potential benefits. This was consistent with various studies done previously [12-15]. Neonatal and maternal outcome was found to be more favourable with paracetamol. Seven NICU admissions were seen in tramadol group. The mean Apgar scores at 1 and 5 minutes were found to be comparable between both groups implying that both paracetamol and tramadol are safe with respect to no neonatal adverse effects. This is in contrast to a previous study by Kaur Makkar J et al. [14] which showed adverse neonatal effects with the use of these drugs but paracetamol being more
safe. Fetal bradycardia was seen in 5 patients in tramadol group (17.2%) as compared to 2 patients in paracetamol group (6.6%). Participants in the tramadol group had more incidence of maternal side-effects which is consistent with other studies [12-15]. Thus, hands down the battle of being the better labour analgesic was won by intravenous Paracetamol.
6. Conclusion
In the rural Indian setup with low health-care resources, intravenous paracetamol with better analgesic efficacy, shorter duration of labour and fewer maternal side-effects is a better labour analgesic than tramadol.
Funding sources
Nil
Conflict of interest
Nil
Acknowledgement
Nil
References
- Melzack R. The myth of painless childbirth. Pain 19 (1984): 321-337.
- Pandya ST. Labour analgesia: recent advances. Indian J Anaesth 54 (2010): 400-408.
- Chhaya V Sharma, Vivek Mehta. Paracetamol: mechanisms and updates. Continuing Education in Anaesthesia Critical Care and Pain 14 (2014): 153-158.
- Sinatra RS, Jahr JS, Reynolds LW et al. Efficacy and safety of single and repeated administration administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopaedic surgery. Anesthesiology 102 (2005): 822–831.
- Togrul T, Yildrim ZB, Cengiz M, et al. Comparison of intravenous paracetamol and tramadol for postoperative analgesia in patients with septo-rhinoplasty. Anest Derg 19 (2011): 213–216.
- Arslan M, Celep B, Çiçek R, et al. Comparing the efficacy of preemptive intravenous paracetamol on the reducing effect of opioid usage in cholecystectomy. J Res Med Sci 18 (2013): 172–177.
- Sudha Patil, S.C. Somashekara, G.K. Veerabhadra Goud, S. Bhanurekha, L. Jayanthi Reddy, S. Deepalaxmi. Tramadol analgesia in labour. Int J Pharm Biomed Res 3 (2012): 49-51.
- Kumari K, Swaroop N, Sharma P, Seth S, Kanti V, Kumar D. Intravenous infusion of tramadol- a safe labour analgesia. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 4 (2015): 1044-1047.
- Dayer P, Desmeules J, Collart L. Pharmacology of tramadol. Drugs 53 (1997): 18-24.
- Saleh HS, Abdelsalam WA, Helal KF, Abdelhamid Attiya AM. Tramadol injection versus epidural analgesia in controlling labour pain. JFIV Reprod Med Genet 5 (2015): 274.
- Moller PL, Sindet-Pedersen S, Petersen CT, Juhl GI, Dillenschneider A, Skoglund LA. Onset of acetaminophen analgesia: comparison of oral and intravenous routes after third molar surgery. Br J Anaesth 94 (2005): 642-648.
- Hema Mohan, Rekha Ramappa, Sandesh M., Akash B.K. Intravenous paracetamol infusion versus intramuscular tramadol as an intrapartum labor analgesic. Int J Reprod Contracept Obstet Gynecol 4 (2015): 1726-1729.
- Meenakshi Lallar, Haq ul Anam, Rajesh Nandal, Sunder Pal Singh, Surabhi Katyal. Intravenous paracetamol infusion versus intramuscular tramadol as an intrapartum labor analgesic. The journal of obstetrics and gynecology of India 65 (2015): 17-22.
- Jeetinder Kaur Makkar, Kajal Jain, Nidhi Bhatia, Vanita Jain, Sanwar Mal Mithrawal. Comparison of analgesic efficacy of paracetamol and tramadol for pain relief in active labor. Journal of clinical Anaesthesia 27 (2015): 159-163.
- Bishnu Prasad Das, Javed Ali, Ankita Baruah. Comparative study between intravenous paracetamol and intramuscular tramadol as labour analgesic. Int J Sci Res 5 (2016): 1675-1679.
- Khooshideh M., Shahriari A. A comparison of tramadol and pethidine analgesia on the duration of labour: a randomized clinical trial. Australian and New Zealand Journal of Obstetrics and Gynecology 49 (2009): 59-63.
- Abdollahi MH, Mojibian M, Pishgahi A, Mallah F, Dareshiri S, Mohammadi S, Naghavi-Behzad M. Intravenous paracetamol versus intramuscular pethidine in relief of labour pain in primigravid women. Niger Med J 55 (2014): 54-57.
- Elbohoty AE, Abd-Elrazek H, Abd-El-Gawad M, et al. Intravenous infusion of paracetamol versus intravenous pethidine as an intrapartum analgesic in the first stage of labor. Int J Gynaecol Obstet 118 (2012): 7–10.
