A Predictor for Decreased Left Ventricular Ejection Fraction in Patients Present to the Emergency Room with Non St Segment Elevation Myocardial Infarction
Article Information
Ramzi A. Almohammadi1*
1Division of Cardiology, Department of Medicine, King Abdulaziz University, P.O. Box 80205, Jeddah 21589, Saudi Arabia
*Corresponding author: : Ramzi A. Almohammadi, MD, Division of Cardiology, Department of Medicine, King Abdulaziz University, P.O. Box 80205, Jeddah 21589, Saudi Arabia
Received: 26 February 2024; Accepted: 04 March 2024; Published: 19 March 2024
Citation: Ramzi A. Almohammadi. A Predictor for Decreased Left Ventricular Ejection Fraction in Patients Present to the Emergency Room with Non St Segment Elevation Myocardial Infarction. Cardiology and Cardiovascular Medicine. 8 (2024): 89-95.
View / Download Pdf Share at FacebookAbstract
Background: Potassium (K) is a vital electrolyte in medical settings, essential for the maintenance of regular cardiac function. Deviant potassium levels from its normal range may impact the electrical activity of the heart, possibly resulting in arrhythmias and other issues related to the heart.
Objective: This study aims to assess the initial potassium level upon arrival of patient with NSTEMI as a predicator for low LVEF.
Method: A study analyzed 346 patients with Non-ST Elevation Myocardial Infarction - Acute Coronary Syndrome (NSTEMI-ACS) at King Abdulaziz University Hospital. The study analyzed several parameters such as duration of chest pain, diabetes, age, initial potassium and magnesium levels, LVEF by echocardiography, electrical instability, and treatment plan.
Results: Results revealed the first potassium level seems to be a good indicator of low LVEF in people who have had a NSTEMI. Based on our research, lower potassium levels are linked to a higher risk of cardiovascular problems, and this risk rises as potassium levels drop. .
Keywords
Initial K-level; LVEF; NSTEMI; electrolytes; TIMI scores; Grace Score
Article Details
1. Introduction
Non-ST Segment Elevation Myocardial Infarction (NSTEMI) is a myocardial infarction that happens when there is an incomplete obstruction or constriction of one or more coronary arteries, resulting in decreased blood supply to the cardiac muscle [1, 2]. In contrast to STEMI (ST Segment Elevation Myocardial Infarction), NSTEMI usually does not exhibit substantial ST-segment elevation on an electrocardiogram (ECG) [3, 4]. The diagnosis of NSTEMI entails a comprehensive assessment of the patient's symptoms, examination of ECG results, and analysis of blood samples to identify cardiac biomarkers like troponin [5, 6]. These biomarkers are released into the bloodstream as a response to heart muscle injury. Potassium (K) is a vital electrolyte in medical settings, essential for the maintenance of regular cardiac function [7, 8]. Deviant potassium levels may impact the electrical activity of the heart, possibly resulting in arrhythmias and other issues related to the heart [9] Left ventricular ejection fraction (LVEF) quantifies the efficiency of the left ventricle in propelling blood throughout each cardiac cycle [10]. A diminished LVEF suggests inadequate cardiac pumping function, potentially indicating heart failure or other cardiac pathologies [11, 12]. Dyskalemia, which refers to both hypo- and hyperkalemia, is often seen in patients with heart failure. It is associated with the underlying physiological mechanisms, medications used for therapy, and the presence of other medical conditions [13]. Hypokalemia is characterized by a blood potassium level below 3.5 mmol/L [14] , whereas hyperkalemia is characterized by a serum potassium level over 5 mmol/L [15]. Both abnormally low (hypo-) and abnormally high (hyper-) levels of potassium in the blood have been linked to a negative outcome in individuals with heart failure [16, 17]. Nevertheless, it remains uncertain if this correlation implies causation [18]. This study aims to Assess the initial potassium level as a predicator for low LVEF in patients diagnosed with NSTEMI.
2. Methods
A retrospective analysis was conducted on a cohort of 346 patients who were hospitalized to King Abdulaziz University Hospital with Non-ST Elevation Myocardial Infarction - Acute Coronary Syndrome (NSTEMI-ACS). We selected patients for participation in our study according to certain criteria for inclusion and exclusion. We analysed the duration of chest pain, the presence or absence of diabetes mellitus, the age of the patient below or above 60, the initial potassium and magnesium levels upon arrival to the emergency room, the ejection fraction determined by echocardiography within 24 hours after admission, the occurrence of electrical instability, and the treatment plan. The eligibility criteria for this study include patients who have been diagnosed with NSTEMI, as well as those who have a GRACE (Global Registry of Acute Coronary Events) score above 109 and a TIMI (Thrombolysis in Myocardial Infarction) score of 2 or higher. Individuals diagnosed with ST-segment elevation myocardial infarction (STEMI) or unstable angina are not eligible to participate. Additionally, those with a confirmed LVEF below 45% or who are currently prescribed angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARB), or diuretics for reasons unrelated to heart failure are also excluded. Furthermore, people who are receiving renal replacement therapy or those who have been diagnosed with severe mitral regurgitation (MR) based on echocardiography results are not included. In addition, individuals with a GRACE score less than 109 or a TIMI score less than 2 are not eligible to be included in the research. The purpose of these criteria is to guarantee that the group of people being studied consists of persons with NSTEMI who fulfill particular clinical and prognosis thresholds. This helps to make the research group more uniform and relevant.
3. Results
The data in table (1) shows that a lower TIMI score corresponds to a reduced risk of events, while a higher score implies a greater risk. Individuals with TIMI scores of 0 to 2 are classified as low risk, those with scores of 2 to 3 are categorized as medium risk, and those with scores of 3 to 4 are classified as high risk. Lower potassium levels are associated with a higher risk of cardiovascular events, as shown by the supplied criteria. Individuals with potassium levels below 4 are at moderate risk, those with levels below 3.5 are at medium risk, and those with levels below 3 are at high risk. A decreased left ventricular ejection fraction (LVEF) indicates diminished heart function and a higher likelihood of cardiovascular incidents. persons with LVEF levels below 50% are considered moderate risk, while those with values below 45% are categorized as medium risk, and persons with values below 40% are classified as high risk. A higher GRACE score signifies an increased likelihood of experiencing negative consequences. Individuals with GRACE scores below 109 are classified as low risk, while those with values over 109 but below 110 are considered medium risk, and those with scores above 110 are categorized as high risk.
Table 1: an indicator of TIMI-score, K level, LVEF ratio, and GRACE score
|
|
Low risk |
Medium risk |
High risk |
|
TIMI-score |
0 to 2 |
2 to 3 |
3 to 4 |
|
K level |
<4 |
<3.5 |
<3 |
|
LVEF |
<50% |
<45% |
<40% |
|
GRACE score |
<109 |
>109 |
>110 |
Table 2: NO of patients according to Layer for variables age and EF, K level, and pulmonary edema
|
No of patients |
patients case |
|
231 |
patients in the study |
|
117 |
patients with EF less than 45% |
|
114 |
patients with EF > 45% |
|
74 |
patients age more than 60 years |
|
38 |
patients K less than 3.5 |
|
28 |
patients K more than 5.0 |
|
63 |
patients K 3.5-4 |
|
73 |
Patients K 4-5 |
|
20 |
pulmonary edema |
Table 3: groups according to K level and sex
|
GROUP |
N OF THE Patients |
male |
female |
K LEVEL |
age>=60 |
age<60 |
|
Q1 |
48 |
31 |
17 |
K <3.5 |
36 |
12 |
|
Q2 |
73 |
49 |
24 |
K 3.5-4 |
60 |
13 |
|
Q3 |
83 |
56 |
27 |
K 4-5 |
64 |
19 |
|
Q4 |
27 |
15 |
12 |
K > 5 |
18 |
9 |
Table 4 displays risk factor points for both the TIMI (Thrombolysis in Myocardial Infarction) score and the GRACE (Global Registry of Acute Coronary Events) score. Continuous, intense, or expanding chest discomfort, resulting in 1 point. Severe symptoms in patients are associated with a greater risk. Continual symptoms: Chest discomfort lasting 20 minutes or more, which also scores 1 point. Indicating that the length of chest discomfort is a crucial element in evaluating risk. A creatinine level over 1.5 mg/dL is given 1 point. Increased creatinine levels suggest possible renal impairment, which may be a sign of worse results. A C-reactive protein concentration over 2.0 mg/dL results in the allocation of 1 point. High levels of C-reactive protein indicate inflammation in the body, which may be linked to a higher risk of cardiovascular issues. Troponin levels over 0.04 ng/ml result in 1 point being given for elevated troponin levels. Increased troponin levels suggest injury to the heart muscle, serving as a crucial indicator of acute coronary syndromes. Potassium levels below 3.5 mmol/L get 1 point. Decreased potassium levels may disturb regular heart function and perhaps exacerbate results in individuals with acute coronary syndromes.
Table 4: TIMI score & Grace score
|
Risk factor points |
point |
|
More severe symptoms (chest pain that is persistent, severe, or spreads to the arms, neck, or jaw) |
1 |
|
Persistent symptoms (chest pain lasting 20 minutes or longer) |
1 |
|
High creatinine levels (>1.5 mg/dL) |
1 |
|
Elevated C-reactive protein levels (>2.0 mg/dL) |
1 |
|
Elevated troponin levels (>0.04 ng/ml) |
1 |
|
Low potassium levels (<3.5 mmol/L) |
1 |
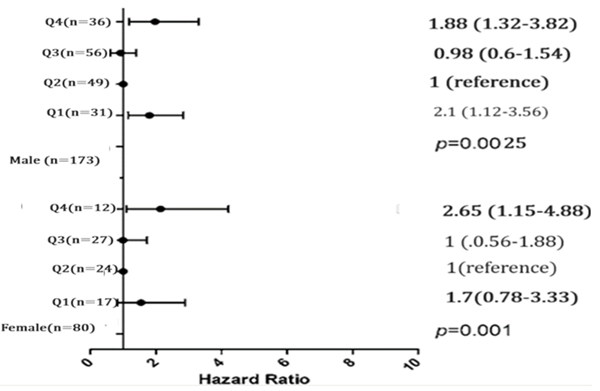
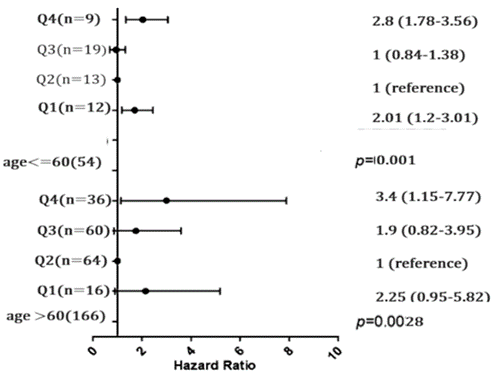
Table 5 displays the initial features of a population grouped by their initial potassium levels (K). The mean age of the whole population is 64.7 years. There is a substantial age difference between the potassium groups (P = 0.02). The age difference between the groups is minimal, ranging from 64.2 to 65.3 years. The table displays the distribution of males and females in each potassium group. Statistically significant gender distribution variations exist between the potassium groups, with a P-value of 0.0025 for males and 0.001 for females. There is a notable disparity in the occurrence of diabetes mellitus across the potassium groups (P < 0.001). The incidence varies from 2.5% to 3.4% across the different groupings. There is a notable disparity in the occurrence of hypertension across the potassium groups (P < 0.001). The prevalence varies from 2.2% to 6.9% across the different categories. There is a notable disparity in the prevalence of acute pulmonary problems between the two groups (P < 0.001). There is a notable disparity in serum creatinine levels across the potassium groups (P < 0.001). There is an inverse relationship between creatinine levels and potassium levels. There is a notable disparity in potassium levels across the groups (P = 0.02). There is a notable disparity in TIMI scores between the potassium groups with a statistical significance of P < 0.001. Elevated potassium levels correlate with increased TIMI scores. There is a notable disparity in Grace ratings across the two groups (P < 0.001). The same results across all categories suggest possible data discrepancies. There is a substantial variation in LVEF across the potassium groups (P < 0.001). Elevated potassium levels are usually associated with increased left ventricular ejection fraction (LVEF).
Table 5: Baseline characteristics according to baseline K
|
Characteristics |
TOTAL (N=231) |
K <3.5 (N=48) |
K 3.5-4 (N=73) |
K 4-5 (N(83) |
K > 5 (N=27) |
*P value |
|
age |
64.7 ± 10.6 |
65.3 ± 10.9 |
64.2 ± 10.2 |
64.8 ± 10.32 |
65.2 ± 10.1 |
0.02 |
|
male |
151 |
31 |
49 |
56 |
15 |
0.0025 |
|
female |
80 |
17 |
24 |
27 |
12 |
0.001 |
|
History of |
||||||
|
Diabetes mellitus |
46 (3.2) |
15(3.4) |
10(2.5) |
9(2.5) |
12 (3.2) |
<0.001 |
|
Hypertension |
150(6.9) |
32(5.6) |
44(2.33) |
38(6.5) |
10(2.2) |
<0.001 |
|
Acute pulmonary |
20 |
12 |
7 |
1 |
0 |
<0.001 |
|
Laboratory results |
||||||
|
Serum creatinine (mg/dL) |
94.3 ± 50.3 |
88.0 ± 28.9 |
60.0 ± 11.8 |
58.8 ± 13.9 |
56.8 ± 12.6 |
<0.001 |
|
Potassium, mmol/L |
3.95 ± 0.5 |
3.35 ± 0.5 |
3.95 ± 0.5 |
4.6± 0.5 |
5.23± 0.5 |
0.02 |
|
TIMI score |
2.2 ±0.88 |
5.4 ±0.92 |
4.9±0.68 |
3.02 ±0.65 |
2.0.1 ±0.44 |
<0.001 |
|
grace score |
2.2 ±0.88 |
2.2 ±0.88 |
2.2 ±0.88 |
2.2 ±0.88 |
2.2 ±0.88 |
<0.001 |
|
LVEF |
44.7 ± 0.4 |
43.7 ± 0.24 |
44.6 ± 0.6 |
45.1 ± 0.33 |
45.7 ± 0.45 |
<0.001 |
4. Discussion
Potassium is an essential electrolyte that plays a key role in regulating appropriate heart function (19). Changes in potassium levels may impact the excitability and contractility of the heart muscle, which may result in heart malfunction [19, 20]. Low potassium levels (hypokalemia) have been linked to irregular heartbeats and reduced heart muscle function, perhaps leading to a drop in LVEF [21]. On the other hand, elevated amounts of potassium, known as hyperkalemia, may also impact heart function, but the underlying processes are intricate and not fully understood [22]. This study aims to assess the initial K levels as a protentional indicator for low LVEF in patients presented to emergency room with NSTEMI-ACS. The study found that as the TIMI score rises, signifying a greater risk based on the scoring method, there is a proportional increase in the likelihood of adverse cardiovascular events. A lower TIMI score is associated with a decreased risk of events, while a higher score indicates a higher risk. These findings are contradicted to those of Ababneh MJ., et al. [23] who found that there is a significant relation between TIMI and heightened risk of major cardiovascular adverse events (MACE). The research found that the TIMI risk score often underestimated the risk in the study group. Yanqiao L, et al. [24] also found that GRACE demonstrated superior prediction accuracy compared to TIMI in East Asian NSTEMI patients for both in-hospital and long-term results. Using TIMI and GRACE scores sequentially is a simple and effective method for predicting outcomes in East Asian patients with NSTEMI. Our findings proved that lower potassium levels are associated with a higher risk of cardiovascular events. Ma Y, et al.,[25] found that Increased salt and decreased potassium consumption, as determined by several 24-hour urine samples, were linked in a proportional way to an elevated risk of cardiovascular issues. A decreased left ventricular ejection fraction (LVEF) indicates diminished heart function and a higher likelihood of cardiovascular incidents. These findings agrees with the findings of Jensen AM, et al.,[26] whose findings suggest that relatively subtle impairments of systolic function (detected based on LVEF or strain) are independently associated with incident HF and HF with reduced LVEF in late life.
Regarding comorbidities, Diabetes mellitus was much less common in the potassium groups than in the other groups (P < 0.001). Among the different groups, the rate ranges from 2.5% to 3.4%. The number of cases of high blood pressure varies a lot between the potassium groups (P < 0.001). The rates of occurrence range from 2.2% to 6.9% for each group. On contrast Tafesse E, [27] found that Patients with a higher Charlson Comorbidity Index (CCI) are more likely to develop hyperkalemia (HK) and are at a greater risk of experiencing negative clinical consequences related to abnormal blood potassium levels, necessitating regular clinical monitoring. Imbalances in potassium levels are a prevalent issue among electrolyte disorders [28, 29]. Research has shown that low potassium levels (<3.5 mmol/L) are associated with an increased occurrence of ventricular arrhythmias in cases of myocardial infarction [30, 31]. These studies emphasized the significance of potassium imbalances as a risk factor for ventricular fibrillation in myocardial infarction patients [32, 33]. However, they were conducted before the era of primary percutaneous coronary intervention (PPCI), involved a limited number of patients, and defined the outcome as cardiac arrest, which means that not all arrests may have been due to ventricular fibrillation [32, 34] Moreover, none of these investigations differentiated between individuals with ST-elevation myocardial infarction (STEMI) and those with non-STEMI [32]. Hyperkalemia results from an excess of potassium intake, poor potassium excretion, or transcellular changes [35, 36] Hyperkalemia is often caused by a combination of factors, including poor kidney function, pharmaceutical use, and high blood sugar levels [37]. Healthy persons may adjust to excessive potassium intake by increasing excretion,[38] therefore increased potassium consumption is usually not the only reason for hyperkalemia, and kidney failure is often present [39]. Hypokalemia occurs due to aberrant losses, transcellular changes, or inadequate intake [40]. Insufficient potassium intake is seldom the only reason for hypokalemia [41], since the kidney may reduce potassium output in response to reduced intake [42]. However, inadequate intake commonly plays a role in hypokalemia among hospitalized patients [43]. The clinical utility of potassium levels in predicting poor LVEF [44] relies on its capacity to accurately differentiate between individuals with low and normal LVEF [18, 44]. High discriminate ability of potassium levels increases their accuracy as predictors. The predictive accuracy of potassium levels may be affected by variables including age, existing health conditions, medication, and electrolyte imbalances [45]. Considering these components and how they interact might improve the prognostic precision of potassium levels for poor LVEF.
Conclusion:
The connection between potassium levels and low LVEF in NSTEMI patients may have predictive value. However, a thorough evaluation of its predictive accuracy necessitates a detailed examination of sensitivity, specificity, PPV, NPV, and AUC, in addition to taking into account clinical context and potential confounding factors. Additional study and validation are required to determine the exact prediction precision of potassium levels in this scenario.
References
- Fathima SN. An Update on Myocardial Infarction. Current Research and Trends in Medical Science and Technology 1 (2021).
- Mohebbi B. ST-segment elevation myocardial infarction. Practical Cardiology: Elsevier (2022): 395-411.
- Khan R, Akhter J, Munir U, et al. Frequency of non-ST segment elevation myocardial infarction (NSTEMI) In acute coronary syndrome with normal electrocardiogram (ECG): insights from a cardiology hospital in Pakistan. Cureus 12 (2020): 8758.
- Tziakas D, Chalikias G, Al-Lamee R, et al. Total coronary occlusion in non ST elevation myocardial infarction: Time to change our practice? International Journal of Cardiology 329 (2021): 1-8.
- Muzyk P, Twerenbold R, Morawiec B, et al. Use of cardiac troponin in the early diagnosis of acute myocardial infarction. Kardiologia Polska (Polish Heart Journal) 78 (2020): 1099-1106.
- Tilea I, Varga A, Serban RC. Past, present, and future of blood biomarkers for the diagnosis of acute myocardial infarction—promises and challenges. Diagnostics 11 (2021): 881.
- McLean RM, Wang NX. Potassium. Advances in food and nutrition research 96 (2021): 89-121.
- Kant S, Sellke FW, Feng J. Potassium and Cardiac Surgery (2021).
- Zhao G, Joca HC, Nelson MT, et al. ATP-and voltage-dependent electro-metabolic signaling regulates blood flow in heart. Proceedings of the National Academy of Sciences 117 (2020): 7461-7470.
- Creamer SA, Zhao D, Quill GM, et al., editors. Impact of Hypertension on Left Ventricular Pressure-Strain Loop Characteristics and Myocardial Work. International Workshop on Statistical Atlases and Computational Models of the Heart (2023): 108-118.
- Severino P, Maestrini V, Mariani MV, et al. Structural and myocardial dysfunction in heart failure beyond ejection fraction. Heart failure reviews 25 (2020): 9-17.
- Qin L, Liu X, Li Y. Correlation of serum BNP and ET-1 levels with cardiac pump function and ventricular remodeling in patients with heart failure. Cellular and Molecular Biology 66 (2020): 125-131.
- Savarese G, Xu H, Trevisan M, et al. Incidence, predictors, and outcome associations of dyskalemia in heart failure with preserved, mid-range, and reduced ejection fraction. JACC: Heart Failure 7 (2019): 65-76.
- Abensur Vuillaume L, Ferreira JP, Asseray N, et al. Hypokalemia is frequent and has prognostic implications in stable patients attending the emergency department. PloS one 15 (2020): e0236934.
- Esposito P, Conti NE, Falqui V, et al. New treatment options for hyperkalemia in patients with chronic kidney disease. Journal of Clinical Medicine 9 (2020): 2337.
- Aldahl M, Jensen A-SC, Davidsen L, et al. Associations of serum potassium levels with mortality in chronic heart failure patients. European Heart Journal 38 (2017): 2890-2896.
- Bowling CB, Pitt B, Ahmed MI, et al. Hypokalemia and outcomes in patients with chronic heart failure and chronic kidney disease: findings from propensity-matched studies. Circulation: Heart Failure 3 (2010): 253-260.
- Sfairopoulos D, Arseniou A, Korantzopoulos P. Serum potassium and heart failure: association, causation, and clinical implications. Heart Failure Reviews 26 (2021): 479-486.
- Severino P, D’Amato A, Pucci M, et al. Ischemic heart disease and heart failure: role of coronary ion channels. International Journal of Molecular Sciences 21(2020): 3167.
- Grandi E, Sanguinetti MC, Bartos DC, et al. Potassium channels in the heart: structure, function and regulation. The Journal of physiology 595 (2017): 2209-2228.
- Kihlgren M, Almqvist C, Amankhani F, et al. The U-wave: A remaining enigma of the electrocardiogram. Journal of Electrocardiology (2023).
- Ferreira JP, Butler J, Rossignol P, et al. Abnormalities of potassium in heart failure: JACC state-of-the-art review. Journal of the American College of Cardiology 75 (2020): 2836-5280.
- Ababneh MJ, Smadi MM, Al-Kasasbeh A, et al. Validity of TIMI Risk Score and HEART Score for Risk Assessment of Patients with Unstable Angina/Non-ST Elevation Myocardial Infarction Presented to an Emergency Department in Jordan. Open Access Emergency Medicine (2023): 465-471.
- Yanqiao L, Shen L, Yutong M, et al. Comparison of GRACE and TIMI risk scores in the prediction of in-hospital and long-term outcomes among East Asian non-ST-elevation myocardial infarction patients. BMC Cardiovascular Disorders 22 (2022): 4.
- Ma Y, He FJ, Sun Q, et al. 24-hour urinary sodium and potassium excretion and cardiovascular risk. New England Journal of Medicine 386 (2022): 252-263.
- Jensen AMR, Zierath R, Claggett B, et al. Association of left ventricular systolic function with incident heart failure in late life. JAMA cardiology 6 (2021): 509-520.
- Tafesse E, Hurst M, Sugrue D, et al. Serum potassium as a predictor of adverse clinical outcomes in patients with increasing comorbidity burden. European Heart Journal-Quality of Care and Clinical Outcomes 8 (2022): 61-69.
- Petrosino A, Bagordo D, Fürstenberg-Schaette A, et al. Common electrolyte abnormalities. Primer on Nephrology (2022): 263-297.
- Albeladi FI, Salem IMW, Albandar AA, et al. Electrolyte imbalance in infectious disease patients at King Abdulaziz Hospital, Jeddah. Journal of Taibah University Medical Sciences 17 (2022): 256-263.
- Farah R, Nassar M, Aboraya B, et al. Low serum potassium levels are associated with the risk of atrial fibrillation. Acta Cardiologica 76 (2021): 887-890.
- Mahmood Z. Serum potassium and calcium level in patients with post-myocardial infarction ventricular fibrillation. The Medical Journal of Basrah University 39 (2021): 47-53.
- Belkouche A, Yao H, Putot A, et al. The multifaceted interplay between atrial fibrillation and myocardial infarction: a review. Journal of clinical medicine 10 (2021): 198.
- Wongtanasarasin W, Meelarp N. Replacing Potassium in the Emergency Department May Not Decrease the Hospital Mortality in Mild Hypokalemia: A Propensity Score Matching Analysis. Medicina 59 (2023): 1912.
- Ravn Jacobsen M, Jabbari R, Glinge C, et al. Potassium Disturbances and Risk of Ventricular Fibrillation Among Patients With ST?Segment–Elevation Myocardial Infarction. Journal of the American Heart Association 9 (2020): e014160.
- Fordjour KN, Walton T, Doran JJ. Management of hyperkalemia in hospitalized patients. The American journal of the medical sciences 347 (2014): 93-100.
- Kim MJ, Valerio C, Knobloch GK. Potassium Disorders: Hypokalemia and Hyperkalemia. American Family Physician 107 (2023): 59-70A.
- Lindner G, Burdmann EA, Clase CM, et al. Acute hyperkalemia in the emergency department: a summary from a Kidney Disease: Improving Global Outcomes conference. European Journal of Emergency Medicine 27 (2020): 329-337.
- Preuss HG. Sodium, chloride, and potassium. Present knowledge in nutrition: Elsevier; 2020. p. 467-84.
- Yamada S, Inaba M. Potassium metabolism and management in patients with CKD. Nutrients 13 (2021): 1751.
- Blanchard A, editor Pathophysiologic approach in genetic hypokalemia. Annales d'Endocrinologie (2023).
- Tinawi M. Hypokalemia: a practical approach to diagnosis and treatment. Archives of Clinical and Biomedical Research 4 (2020): 48-66.
- Clase CM, Carrero J-J, Ellison DH, et al. Potassium homeostasis and management of dyskalemia in kidney diseases: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney international 97 (2020): 42-61.
- Fiaccadori E, Sabatino A, Barazzoni R, et al. ESPEN guideline on clinical nutrition in hospitalized patients with acute or chronic kidney disease. Clinical Nutrition 40 (2021): 1644-1668.
- Toledo CC, Vellosa Schwartzmann P, Miguel Silva L, et al. Serum potassium levels provide prognostic information in symptomatic heart failure beyond traditional clinical variables. ESC heart failure 8 (2021): 2133-2143.
- Furuland H, McEwan P, Evans M, et al. Serum potassium as a predictor of adverse clinical outcomes in patients with chronic kidney disease: new risk equations using the UK clinical practice research datalink. BMC nephrology 19 (2018): 1-16.