A Peculiar Concurrent Presentation of Spinal Tuberculosis In A Diagnosed Case of Neurofibromatosis Type 1 – An Atypical Case Report
Article Information
Vishnu Vikraman Nair1*, Vishal Kundnani2, Mukul Jain1, Sunil Shamjibhai Chodavadiya1, Jenil Patel1
1FELLOW in Spine Surgery, Department of Orthopaedics, Bombay hospital and medical research institute
2Consultant Spine Surgeon, Department of Orthopaedics, Bombay hospital and medical research institute
*Corresponding Author: Dr Vishnu Vikraman Nair, FELLOW in Spine Surgery, Department of Orthopaedics, Bombay hospital and medical research institute.
Received: 15 June 2023; Accepted: 20 June 2023; Published: 21 June 2023
Citation: Vishnu Vikraman Nair, Vishal Kundnani, Mukul Jain, Sunil Shamjibhai Chodavadiya, Jenil Patel. A Peculiar Concurrent Presentation of Spinal Tuberculosis In A Diagnosed Case of Neurofibromatosis Type 1 – An Atypical Case Report. Journal of Spine Research and Surgery 5 (2023): 46-50.
View / Download Pdf Share at FacebookAbstract
Spinal tuberculosis is a prevalent ailment observed in the Asian demographic, which can result in neurodeficit if not addressed during the initial phases. Neurofibromatosis is a hereditary disorder that results in the manifestation of dystrophic bony characteristics accompanied by the development of multiple spinal tumors. This study presents a unique case of a young female who had previously been diagnosed with Neurofibromatosis. Additionally, she exhibited symptoms of tubercular spondylodiscitis, resulting in kyphotic deformity and paraparesis. The present case report discusses the challenges encountered during the preoperative and intra-operative management of a patient presenting with the co-occurrence of neurofibromatosis and tuberculosis of the spine. Despite the advancements in imaging modalities, such as magnetic resonance imaging, and surgical techniques, the prompt diagnosis and management of spinal tuberculosis with Neurofibramatosis remains complex and demanding. The objective of this review is to examine the diagnosis, preoperative planning, and treatment of spinal tuberculosis in a patient of Neurofibromatosis type 1, utilizing studies that possess adequate literature, lucidly presented outcomes, and defensible conclusions.
Keywords
Spinal Tuberculosis; Decompression; Potts spine; Neurofibromatosis type 1
articles about Spinal Tuberculosis Research articles about Spinal Tuberculosis review articles about Spinal TuberculosisSpinal Tuberculosis PubMed articles Spinal Tuberculosis PubMed Central articles Spinal Tuberculosis 2024 articles Spinal Tuberculosis 2025 articles Spinal Tuberculosis Scopus articles Spinal Tuberculosis impact factor journals Spinal Tuberculosis Scopus journals Spinal Tuberculosis PubMed journals Spinal Tuberculosis medical journals Spinal Tuberculosis free journals Spinal Tuberculosis best journals Spinal Tuberculosis top journals Spinal Tuberculosis free medical journals Spinal Tuberculosis famous journals Spinal Tuberculosis Google Scholar indexed journals articles about Decompression Research articles about Decompression review articles about DecompressionDecompression PubMed articles Decompression PubMed Central articles Decompression 2025 articles Decompression 2026 articles Decompression Scopus articles Decompression impact factor journals Decompression Scopus journals Decompression PubMed journals Decompression medical journals Decompression free journals Decompression best journals Decompression top journals Decompression free medical journals Decompression famous journals Decompression Google Scholar indexed journals articles about Potts spine Research articles about Potts spine review articles about Potts spinePotts spine PubMed articles Potts spine PubMed Central articles Potts spine 2026 articles Potts spine 2027 articles Potts spine Scopus articles Potts spine impact factor journals Potts spine Scopus journals Potts spine PubMed journals Potts spine medical journals Potts spine free journals Potts spine best journals Potts spine top journals Potts spine free medical journals Potts spine famous journals Potts spine Google Scholar indexed journals articles about Neurofibromatosis type 1 Research articles about Neurofibromatosis type 1 review articles about Neurofibromatosis type 1Neurofibromatosis type 1 PubMed articles Neurofibromatosis type 1 PubMed Central articles Neurofibromatosis type 1 2027 articles Neurofibromatosis type 1 2028 articles Neurofibromatosis type 1 Scopus articles Neurofibromatosis type 1 impact factor journals Neurofibromatosis type 1 Scopus journals Neurofibromatosis type 1 PubMed journals Neurofibromatosis type 1 medical journals Neurofibromatosis type 1 free journals Neurofibromatosis type 1 best journals Neurofibromatosis type 1 top journals Neurofibromatosis type 1 free medical journals Neurofibromatosis type 1 famous journals Neurofibromatosis type 1 Google Scholar indexed journals articles about spondylodiscitis Research articles about spondylodiscitis review articles about spondylodiscitisspondylodiscitis PubMed articles spondylodiscitis PubMed Central articles spondylodiscitis 2028 articles spondylodiscitis 2029 articles spondylodiscitis Scopus articles spondylodiscitis impact factor journals spondylodiscitis Scopus journals spondylodiscitis PubMed journals spondylodiscitis medical journals spondylodiscitis free journals spondylodiscitis best journals spondylodiscitis top journals spondylodiscitis free medical journals spondylodiscitis famous journals spondylodiscitis Google Scholar indexed journals articles about spinal column Research articles about spinal column review articles about spinal columnspinal column PubMed articles spinal column PubMed Central articles spinal column 2029 articles spinal column 2030 articles spinal column Scopus articles spinal column impact factor journals spinal column Scopus journals spinal column PubMed journals spinal column medical journals spinal column free journals spinal column best journals spinal column top journals spinal column free medical journals spinal column famous journals spinal column Google Scholar indexed journals articles about mid dorsal Research articles about mid dorsal review articles about mid dorsalmid dorsal PubMed articles mid dorsal PubMed Central articles mid dorsal 2030 articles mid dorsal 2031 articles mid dorsal Scopus articles mid dorsal impact factor journals mid dorsal Scopus journals mid dorsal PubMed journals mid dorsal medical journals mid dorsal free journals mid dorsal best journals mid dorsal top journals mid dorsal free medical journals mid dorsal famous journals mid dorsal Google Scholar indexed journals articles about mid-back pain Research articles about mid-back pain review articles about mid-back painmid-back pain PubMed articles mid-back pain PubMed Central articles mid-back pain 2031 articles mid-back pain 2032 articles mid-back pain Scopus articles mid-back pain impact factor journals mid-back pain Scopus journals mid-back pain PubMed journals mid-back pain medical journals mid-back pain free journals mid-back pain best journals mid-back pain top journals mid-back pain free medical journals mid-back pain famous journals mid-back pain Google Scholar indexed journals articles about Spine disorder Research articles about Spine disorder review articles about Spine disorderSpine disorder PubMed articles Spine disorder PubMed Central articles Spine disorder 2032 articles Spine disorder 2033 articles Spine disorder Scopus articles Spine disorder impact factor journals Spine disorder Scopus journals Spine disorder PubMed journals Spine disorder medical journals Spine disorder free journals Spine disorder best journals Spine disorder top journals Spine disorder free medical journals Spine disorder famous journals Spine disorder Google Scholar indexed journals
Article Details
Introduction and Background
Infective spondylodiscitis is a medical condition characterized by inflammation of the intervertebral disc and contiguous vertebral bodies seen in endemic areas due to a pathogen called Mycobacterium tuberculosis. Spinal TB accounts to almost 50% of all extrapulmonary TB[1]. This condition typically manifests in the thoracolumbar region, although it may also occur in other regions of the spinal column. Spinal tuberculosis is a disease that is subject to constant evolution due to changing disease patterns, advancements in imaging, and treatment protocols. The emergence of drug resistance also poses a significant challenge in managing this disease. Neurofibramatosis on the other hand is a condition affecting the neural crest cells that is described as a spectrum of complex illnesses with likely hamartomatous origins that affect the neuroectoderm, mesoderm, and endoderm. The condition results in the development of non-malignant neoplasms on or beneath the dermis, as well as on the peripheral nervous system and other anatomical structures[2]. Neurofibromatosis (NF) follows an autosomal dominant inheritance pattern and is characterized by distinct clinical manifestations such as hyperpigmented spots, neurofibromas, Lisch nodules, skeletal and bony anomalies, and a predisposition to neoplastic growths[3]. Neurofibromatosis comprises two distinct subtypes, namely type 1 and type 2. The most prevalent type is NF 1, which exhibits a greater incidence of spinal tumors[4].
This study presents a unique case in which a patient with a history of NF1 was found to have spinal TB resulting in spinal cord compression and paraparesis.
Case Report:
A 32-year-old female patient presented to our clinic with severe mid-back pain of 10-day duration. She reported gait imbalance since the last 2-3 days, which had progressively worsened. On examination, she had severe tenderness in the mid dorsal spine at levels D7-D10, with weakness of MRC grade 3 in both ankle dorsiflexion and MRC grade 4 knee extension. Sensations were preserved at all dermatomes, and proprioception was normal. She also reported a positive history of constitutional symptoms including, weight loss and evening rise in temperature for the past 2-3 months. Past medical history and examination revealed that the patient was a known case of Neurofibromatosis Type 1, with features such as cafe-au-lait lesion on skin, but was otherwise asymptomatic. Patient was unable to walk due to buckling of knee and required support to walk more than 10 feet.
Investigations
Routine laboratory investigations including blood count and biochemistry were normal, but the total leukocyte count was raised to 22,000. Diagnostic imaging in the form of Magnetic Resonance Imaging (MRI) (Fig 1)and plain X-ray dorso-lumbar spine(Fig 2) was carried out, which showed presence of an infective disease process at D7, D8, D9, and D10 levels. There was an evidence of fluid collection in the pre-and paravertebral regions, with intraspinal anterior epidural extension noted at the D8-D9 level causing severe spinal cord compression.(Fig 3) There was also a non-compressive finding of a multiple meningoceles in the left neural foramina of D6-D11 levels with the largest meningocele measuring 7*6.5*5.3 cm in the left paravertebral region.(Fig 4) The possibility of tuberculosis was suspected, and a clinico-pathological correlation, including diagnostic aspiration of the prevertebral fluid collection, was recommended.

Figure 1: Plain MRI T-2 Image showing involvement of D10-D11 levels majorly

Figure 2: Plain Xray radiograph pf Dorsal spine in Anterio-posterior and Lateral view

Figure 3: MRI D-L spine showing extension of the epidural abcess into above and below levels from the involved vertebrae
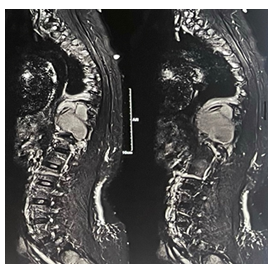
Figure 4: MRI films showing the paraspinal meningocele measuring 7*6.5*5.3 cm
Pre Operative Planning And Treatment
Given the presence of paraparesis and an infectious focus exerting pressure on the spinal cord at the D7-D10 level, it was determined that a surgical intervention involving decompression and stabilisation, as well as drainage of the epidural abscess, was warranted. A computed tomography (CT) (Fig 5)scan was performed to assess the viability of the pedicles, as pedicle destruction is a characteristic feature of Neurofibromatosis Type 1. The computed tomography scan indicated the complete destruction of the pedicles on the right side of the D8-D11 vertebrae and on the left side of the D9-D11 vertebrae. The pedicles located both above and below were observed to be dystrophic and narrow.
A computed tomography (CT) scan was performed, utilising a three-dimensional (3D) reconstruction, in order to preoperatively plan the trajectories of screws and determine the appropriate size of screws that could be utilised for pedicle screw fixation.
Following preoperative planning, the patient underwent decompression and fixation surgery through a conventional midline posterior approach, which involved transpedicular decompression of the spinal cord and drainage of the epidural abscess. Pedicle screw fixation was performed from the sixth thoracic vertebra to the first lumbar vertebra. However, the right-sided pedicles were omitted from the eighth to the eleventh thoracic vertebrae, and the left-sided pedicles were omitted from the ninth to the eleventh thoracic vertebrae due to the presence of dystrophic pedicles.(Fig 6).
According to the reports, the patient was diagnosed with Multidrug-resistant Tuberculosis based on a positive gene xpert report. Following the operation, the patient was subsequently referred to a Direct Observed Treatment Schedule (DOTS) for further medical management of Tuberculosis.
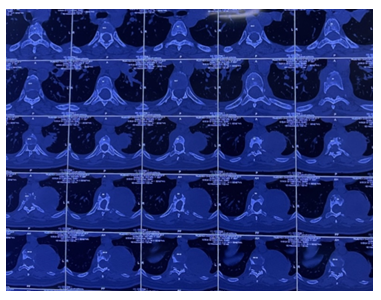
Figure 5: Axial Computed Tomography images showing dystrophic pedicles at multiple levels
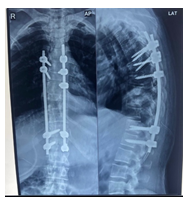
Figure 6: Post operative Xray showing planned pedicle screw instrumentation above and below the Involved levels to provide stabilisation
Discussion
We reported a rare case report of a young 32 year old female who is a known case of Neurofibromatosis Type 1 presenting with constitutional symptoms and paraparesis, managed surgically with decompression and stabilisation. In the literature review we have done there has been no reports of any cases of Potts spine seen in a patient with neurofibromatosis. So the endemicity of Tuberculosis in Indian subcontinent exposes us to rarest of the cases seen in the Tuberculosis spectrum. Southeast Asia is reported to exhibit the second-highest incidence rate, with a prevalence of 226 cases per 100,000 individuals[5]. Even though surgical treatment is not always advised, literature shows good functional outcomes in patients treated surgically. Few studies also show the clinical features that were observed to be linked with inadequate functional recuperation which encompass indications of spinal cord compression, such as neurogenic bowel and bladder, muscle spasms, and weakness, as well as other aetiology’s of cord compression, which included spinal deformity, thoracic spine involvement, vertebral collapse and abscess formation[6,7,8].
The precise prevalence of spinal deformities in individuals with NF1 remains uncertain, with estimates ranging from 2% to 69%[9]. However, scoliosis affecting the thoracic spine is the most frequently observed manifestation[9]. The occurrence of bone destruction and dystrophy is a frequent observation in individuals with NF1. The proposed pathophysiological mechanisms underlying this phenomenon include the localised infiltration or erosion of bone by neurofibromas, primary mesodermal dysplasia, osteomalacia, and endocrine disruptions[10].
Kyphosis leads to a greater degree of neurologic impairment compared to scoliosis due to the development of a pathological spinal flexion. This flexion results in excessive attenuation and deformation of the spinal cord parenchyma, ultimately giving rise to neurological symptoms[11]. Progressive kyphosis is a significant contributor to neurodeficit in cases of spinal tuberculosis also. Considering our case report the involvement of both NF1 with spinal tuberculosis puts our patient in a high risk of progressive neurodeficit and increased risk of paraplegia. The fundamental tenet of surgical intervention involves the execution of intervertebral debridement to achieve surgical decompression, which is subsequently followed by vertebral fixation. Two techniques for fixation, namely autologous bone grafts and titanium cage, have demonstrated remarkable functional outcomes in terms of JOA[12].
The process of segmental instrumentation may present difficulties at times due to the inadequate anchorage points for fixation caused by severely deformed vertebrae. Therefore, preoperative CT analysis is a crucial tool in the planning of a secure surgery with optimal hold of the pedicle screws. Excessive bleeding may be caused by the existence of paraspinal neurofibromas and plexiform venous channels in the soft tissues that envelop the spinal region which may also increase chances of postoperative hematoma formation[13].
To summarise, the condition of Neurofibromatosis presents significant obstacles throughout the process of diagnosis and development of treatment approaches. The presence of a secondary infection caused by Mycobacterium tuberculosis has presented a significant obstacle in devising a treatment regimen that is both safe and efficacious in achieving a successful recovery. The manifestation of progressive deformity is indicative of an imminent state of neurodeficit, which necessitates prompt and timely surgical intervention.
Conclusion
The present case report elucidates an infrequent manifestation of Potts spine with spinal cord compression in association with Neurofibromatosis Type 2. Timely identification and proper preoperative templating of the dystrophic pedicles are necessary in such instances to have a safely planned surgery. The patient underwent a diagnostic aspiration of prevertebral fluid collection and decompression and fixation surgery in order to prevent worsening of neurodeficit.
Source(s) of support:
None
Conflicting Interest (If present, give more details):
None
References
- Moorthy S, Prabhu NK. Spectrum of MR imaging findings in spinal tuberculosis. AJR Am J Roentgenol 179 (2002): 979-983.
- Crawford AH. Neurofibromatosis. In: Weinstein SL, editor. The pediatric spine: principles and practice. 2. Philadelphia: Lippincott Williams & Wilkins 14 (2001): 427-439.
- National Institutes of Health consensus Development Conference Neurofibromatosis: conference statement. Arch Neurol 45 (1988): 575-578.
- Carman Kb, Yakut A, Anlar B, et al. Spinal neurofibromatosis associated with classical neurofibromatosis type 1: genetic characterisation of an atypical case. BMJ Case Rep (2013): bcr2012008468.
- MacNeil A, Glaziou P, Sismanidis C, et al. Global epidemiology of tuberculosis and progress toward achieving global targets: 2017. MMWR Morb Mortal Wkly Rep 68 (2019): 263-266.
- Bhandari A, Garg RK, Malhotra HS, et al. Outcome assessment in conservatively managed patients with cervical spine tuberculosis. Spinal Cord 52 (2014): 489-493.
- Garg RK, Raut T, Malhotra HS, et al. Evaluation of prognostic factors in medically treated patients of spinal tuberculosis. Rheumatol Int 33 (2013): 3009-3015.
- Shetty AP, Bosco A, Rajasekaran S, et al. Does preserving or restoring lumbar lordosis have an impact on functional outcomes in tuberculosis of the lumbosacral region? Spine Deform 7 (2019): 356-363.
- Akbarnia BA, Gabriel KR, Beckman E, Chalk D. Prevalence of scoliosis in neurofibromatosis. Spine 17 (1992): S244–S248.
- Funasaki H, Winter RB, Lonstein JB, Denis F. Pathophysiology of spinal deformities in neurofibromatosis. J Bone Joint Surg [Am] 76A (1994): 692-700.
- Curtis BH, Fisher RL, Butterfield WL, et al. Neurofibromatosis with paraplegia: report of 8 cases. J Bone Joint Surg [Am] 51A (1969): 843-861.
- Liu Y, Chen Y, Yang L, et al. The surgical treatment and related management for post-tubercular kyphotic deformity of the cervical spine or the cervicothoracic spine. Int Orthop 36 (2012): 367-372.
- Hsu LCS, Lee PC, Leong JCY. Dystrophic spinal deformities in neurofibromatosis. Treatment by anterior and posterior fusion. J Bone Joint Surg [Br] 66B (1984): 495-499.
