A Novel Ultrasound-Guided Approach for the Management of an Anterior Paralabral Cyst of the Hip
Article Information
Michael O Bazzi1*, Michael A Downing2, David Civitarese3, James R Ross4, Joshua B Rothenberg5
1University of California, Irvine Physical Medicine and Rehabilitation Residency, California, United States
2Albany Medical Center Physical Medicine and Rehabilitation Residency, NY, United States
3Northwestern Physical Medicine and Rehabilitation Residency, Illinois, United States
4Orthopedic Sports Medicine, Baptist Health North Orthopedic Care, Boca Raton Regional Hospital, Florida, United States
5Sports Medicine, Baptist Health North Orthopedic Care, Boca Raton Regional Hospital, Florida, United States
*Corresponding Author: Michael O Bazzi, University of California, Irvine Physical Medicine and Rehabilitation Residency, United States.
Received: 03 June 2023; Accepted: 15 June 2023; Published: 27 June 2023
Citation: Michael O Bazzi, Michael A Downing, David Civitarese, James R Ross, Joshua B Rothenberg. A Novel Ultrasound-Guided Approach for the Management of an Anterior Paralabral Cyst of the Hip. Journal of Orthopedics and Sports Medicine. 5 (2023): 300-303.
View / Download Pdf Share at FacebookKeywords
Paralabral cysts; Hip; Joint capsule; Osteoarthritis; Inflammatory rheumatologic disorders
Physical medicine articles Physical medicine Research articles Physical medicine review articles Physical medicine PubMed articles Physical medicine PubMed Central articles Physical medicine 2023 articles Physical medicine 2024 articles Physical medicine Scopus articles Physical medicine impact factor journals Physical medicine Scopus journals Physical medicine PubMed journals Physical medicine medical journals Physical medicine free journals Physical medicine best journals Physical medicine top journals Physical medicine free medical journals Physical medicine famous journals Physical medicine Google Scholar indexed journals Rehabilitation articles Rehabilitation Research articles Rehabilitation review articles Rehabilitation PubMed articles Rehabilitation PubMed Central articles Rehabilitation 2023 articles Rehabilitation 2024 articles Rehabilitation Scopus articles Rehabilitation impact factor journals Rehabilitation Scopus journals Rehabilitation PubMed journals Rehabilitation medical journals Rehabilitation free journals Rehabilitation best journals Rehabilitation top journals Rehabilitation free medical journals Rehabilitation famous journals Rehabilitation Google Scholar indexed journals Orthopedic articles Orthopedic Research articles Orthopedic review articles Orthopedic PubMed articles Orthopedic PubMed Central articles Orthopedic 2023 articles Orthopedic 2024 articles Orthopedic Scopus articles Orthopedic impact factor journals Orthopedic Scopus journals Orthopedic PubMed journals Orthopedic medical journals Orthopedic free journals Orthopedic best journals Orthopedic top journals Orthopedic free medical journals Orthopedic famous journals Orthopedic Google Scholar indexed journals Sports medicine articles Sports medicine Research articles Sports medicine review articles Sports medicine PubMed articles Sports medicine PubMed Central articles Sports medicine 2023 articles Sports medicine 2024 articles Sports medicine Scopus articles Sports medicine impact factor journals Sports medicine Scopus journals Sports medicine PubMed journals Sports medicine medical journals Sports medicine free journals Sports medicine best journals Sports medicine top journals Sports medicine free medical journals Sports medicine famous journals Sports medicine Google Scholar indexed journals Paralabral cysts articles Paralabral cysts Research articles Paralabral cysts review articles Paralabral cysts PubMed articles Paralabral cysts PubMed Central articles Paralabral cysts 2023 articles Paralabral cysts 2024 articles Paralabral cysts Scopus articles Paralabral cysts impact factor journals Paralabral cysts Scopus journals Paralabral cysts PubMed journals Paralabral cysts medical journals Paralabral cysts free journals Paralabral cysts best journals Paralabral cysts top journals Paralabral cysts free medical journals Paralabral cysts famous journals Paralabral cysts Google Scholar indexed journals Connective tissue articles Connective tissue Research articles Connective tissue review articles Connective tissue PubMed articles Connective tissue PubMed Central articles Connective tissue 2023 articles Connective tissue 2024 articles Connective tissue Scopus articles Connective tissue impact factor journals Connective tissue Scopus journals Connective tissue PubMed journals Connective tissue medical journals Connective tissue free journals Connective tissue best journals Connective tissue top journals Connective tissue free medical journals Connective tissue famous journals Connective tissue Google Scholar indexed journals Joint capsule articles Joint capsule Research articles Joint capsule review articles Joint capsule PubMed articles Joint capsule PubMed Central articles Joint capsule 2023 articles Joint capsule 2024 articles Joint capsule Scopus articles Joint capsule impact factor journals Joint capsule Scopus journals Joint capsule PubMed journals Joint capsule medical journals Joint capsule free journals Joint capsule best journals Joint capsule top journals Joint capsule free medical journals Joint capsule famous journals Joint capsule Google Scholar indexed journals Shoulder articles Shoulder Research articles Shoulder review articles Shoulder PubMed articles Shoulder PubMed Central articles Shoulder 2023 articles Shoulder 2024 articles Shoulder Scopus articles Shoulder impact factor journals Shoulder Scopus journals Shoulder PubMed journals Shoulder medical journals Shoulder free journals Shoulder best journals Shoulder top journals Shoulder free medical journals Shoulder famous journals Shoulder Google Scholar indexed journals Osteoarthritis articles Osteoarthritis Research articles Osteoarthritis review articles Osteoarthritis PubMed articles Osteoarthritis PubMed Central articles Osteoarthritis 2023 articles Osteoarthritis 2024 articles Osteoarthritis Scopus articles Osteoarthritis impact factor journals Osteoarthritis Scopus journals Osteoarthritis PubMed journals Osteoarthritis medical journals Osteoarthritis free journals Osteoarthritis best journals Osteoarthritis top journals Osteoarthritis free medical journals Osteoarthritis famous journals Osteoarthritis Google Scholar indexed journals Inflammatory rheumatologic disorders articles Inflammatory rheumatologic disorders Research articles Inflammatory rheumatologic disorders review articles Inflammatory rheumatologic disorders PubMed articles Inflammatory rheumatologic disorders PubMed Central articles Inflammatory rheumatologic disorders 2023 articles Inflammatory rheumatologic disorders 2024 articles Inflammatory rheumatologic disorders Scopus articles Inflammatory rheumatologic disorders impact factor journals Inflammatory rheumatologic disorders Scopus journals Inflammatory rheumatologic disorders PubMed journals Inflammatory rheumatologic disorders medical journals Inflammatory rheumatologic disorders free journals Inflammatory rheumatologic disorders best journals Inflammatory rheumatologic disorders top journals Inflammatory rheumatologic disorders free medical journals Inflammatory rheumatologic disorders famous journals Inflammatory rheumatologic disorders Google Scholar indexed journals Hip labral tears articles Hip labral tears Research articles Hip labral tears review articles Hip labral tears PubMed articles Hip labral tears PubMed Central articles Hip labral tears 2023 articles Hip labral tears 2024 articles Hip labral tears Scopus articles Hip labral tears impact factor journals Hip labral tears Scopus journals Hip labral tears PubMed journals Hip labral tears medical journals Hip labral tears free journals Hip labral tears best journals Hip labral tears top journals Hip labral tears free medical journals Hip labral tears famous journals Hip labral tears Google Scholar indexed journals Femoroacetabular joint articles Femoroacetabular joint Research articles Femoroacetabular joint review articles Femoroacetabular joint PubMed articles Femoroacetabular joint PubMed Central articles Femoroacetabular joint 2023 articles Femoroacetabular joint 2024 articles Femoroacetabular joint Scopus articles Femoroacetabular joint impact factor journals Femoroacetabular joint Scopus journals Femoroacetabular joint PubMed journals Femoroacetabular joint medical journals Femoroacetabular joint free journals Femoroacetabular joint best journals Femoroacetabular joint top journals Femoroacetabular joint free medical journals Femoroacetabular joint famous journals Femoroacetabular joint Google Scholar indexed journals Iliopsoas muscle articles Iliopsoas muscle Research articles Iliopsoas muscle review articles Iliopsoas muscle PubMed articles Iliopsoas muscle PubMed Central articles Iliopsoas muscle 2023 articles Iliopsoas muscle 2024 articles Iliopsoas muscle Scopus articles Iliopsoas muscle impact factor journals Iliopsoas muscle Scopus journals Iliopsoas muscle PubMed journals Iliopsoas muscle medical journals Iliopsoas muscle free journals Iliopsoas muscle best journals Iliopsoas muscle top journals Iliopsoas muscle free medical journals Iliopsoas muscle famous journals Iliopsoas muscle Google Scholar indexed journals Obturator nerve articles Obturator nerve Research articles Obturator nerve review articles Obturator nerve PubMed articles Obturator nerve PubMed Central articles Obturator nerve 2023 articles Obturator nerve 2024 articles Obturator nerve Scopus articles Obturator nerve impact factor journals Obturator nerve Scopus journals Obturator nerve PubMed journals Obturator nerve medical journals Obturator nerve free journals Obturator nerve best journals Obturator nerve top journals Obturator nerve free medical journals Obturator nerve famous journals Obturator nerve Google Scholar indexed journals Sciatic nerve articles Sciatic nerve Research articles Sciatic nerve review articles Sciatic nerve PubMed articles Sciatic nerve PubMed Central articles Sciatic nerve 2023 articles Sciatic nerve 2024 articles Sciatic nerve Scopus articles Sciatic nerve impact factor journals Sciatic nerve Scopus journals Sciatic nerve PubMed journals Sciatic nerve medical journals Sciatic nerve free journals Sciatic nerve best journals Sciatic nerve top journals Sciatic nerve free medical journals Sciatic nerve famous journals Sciatic nerve Google Scholar indexed journals
Article Details
Main Focus of Article:
To share a novel ultrasound guided intervention for management of anterior paralabral cysts of the hip. This article also discusses the clinical presentation, diagnostic investigation, and traditional treatments for paralabral cysts of the hip.
1. Introduction
Paralabral cysts of the hip are viscous, fluid-filled sacs that arise from myxoid degeneration of connective tissue of a joint capsule. Paralabral cysts are most commonly described in association with shoulder joint pathology, however they can also arise within the hip joint, secondary to pathology such as labral tears, dislocation, psoas impingement, osteoarthritis, and inflammatory rheumatologic disorders [1]. These cysts are estimated in 1-4% of the general population and seen in up to 50-70% of patients with hip labral tears [2]. Cyst location at the femoroacetabular joint is generally seen at the anterosuperior position and typically lateral to the iliopsoas muscle [3,4]. Compression of local structures is rare, though femoral vein, obturator nerve, sciatic nerve, and femoral nerve involvement have been reported in the literature [5,6]. The classic patient presentation of a paralabral cyst includes anterior hip pain, limited range of motion (ROM) with internal/external rotation, pain with hip flexion, an occasional “snapping” sensation, positive Flexion Abduction External Rotation (FABER), Flexion Adduction Internal Rotation (FADIR), and Scour tests at the affected joint [2]. MRI and MRA are the gold-standard imaging modalities for cyst visualization and the diagnosis of associated labral tears [2]. However, ultrasound (U/S) is also useful for diagnostic and therapeutic purposes in cysts greater than 1.5 cm in size [2].
U/S-guided approaches in the management of paralabral cysts are more commonly reported in the shoulder joint [7]. Traditional treatment of hip paralabral cysts includes surgical excision of the cyst during arthroscopic labral debridement or repair [2,8]. There is a paucity of literature regarding U/S-guided intervention of paralabral cysts of the hip. However, ultrasound proves to be a useful modality as it allows clear visualization of the target structure along with the ability to identify the femoral neurovascular bundle to avoid potential injury. Thus far, customary non-surgical intervention has involved cyst aspiration with or without a subsequent combination injection of anesthetics with corticosteroids [5]. We introduce a novel U/S-guided cyst rupture technique, where the needle enters the skin from distal to proximal, increasing the conspicuity of needle visualization and making a technically more feasible procedure, and then pressurizing the hip paralabral cyst until rupture.
2. Case Report
A 50-year-old male with an unremarkable orthopedic past medical history was referred for management of his left hip anterior paralabral cyst. An MRI of the left hip, which was completed prior to his referral, demonstrated a tear of the left anterior labrum extending to the superior labrum associated with an anterior paralabral cyst measuring 3.6 × 2.1 cm. This paralabral cyst extended into the left iliopsoas muscles (Figure 1 and 2).
The patient described the pain as sharp, intermittent, 7/10, and located over his anterolateral left hip without radiation. His pain was aggravated with increased activity such as walking, crossing his left-leg over his right, ascending and descending stairs, prolonged standing, and rising from a seated position. Alleviating factors included frequent positional changes. He denied numbness, tingling, and weakness of the left lower extremity. He had previously attempted conservative treatment options without relief, including physical therapy, non-steroidal anti-inflammatory drugs (NSAIDs), and sonographically guided corticosteroid injections to the hip joint capsule. On physical examination, the patient was neurovascularly intact. Muscle strength was 5/5 for hip flexion, hip extension, hip abduction, hip adduction. Pain was elicited with passive internal and external rotation of the left hip joint. Physical examination was also remarkable for a positive anterior impingement sign with pain elicited on flexion, adduction, and internal rotation (FADIR). Ambulation exam revealed a non-antalgic gait.
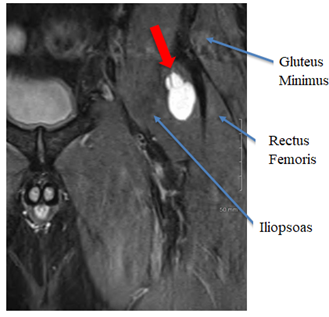
Figure 1: MRI Left Hip (Coronal View): This demonstrates the left hip paralabral cyst (red arrow) with extension into the left iliopsoas muscle belly.
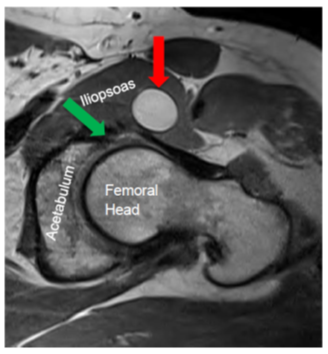
Figure 2: MRI Left Hip (Axial View): This demonstrates the left hip anterior paralabral cyst (red arrow) with associated anterior labral tear (green arrow).
We recommended an ultrasound-guided cyst aspiration and subsequent corticosteroid injection into the joint capsule, for which the patient agreed. The procedure was carried out via sterile technique. The patient was positioned supine with the left leg placed in slight internal rotation. Target structures were localized with a 5-2 MHz curve-linear transducer. Prior to the procedure, the probe was scanned medially, color doppler was employed, and neurovascular structures were identified. The probe was then scanned laterally until the cyst was identified, and color doppler remained on to ensure no vascular flow coming to or from the cystic structure. Color doppler was then turned off to increase the conspicuity of needle visualization. Thereafter, 0.5 cc of 1% lidocaine local anesthesia to the skin and subcutaneous tissues was delivered distal-to-proximal. Following local anesthesia, a new 20-gauge 3.5-inch needle was inserted from distal to proximal into the cyst. A syringe was attached, however no fluid was able to be aspirated (Figure 3). The procedure was then converted to a cyst rupture, in which the cyst was initially pressurized with 0.5 mL of 1% lidocaine when resistance was felt. Next, an additional 0.5 mL of 1% lidocaine was injected, causing the cyst to rupture (Figure 4). After the cyst rupture, a new 25 gauge 3.5-inch needle was inserted from distal to proximal to the hip joint capsule. A new 5 mL syringe containing 3 mL of 1% lidocaine, 1 mL of 4 mg/mL dexamethasone, and 1 mL of 40 mg/mL Kenalog was injected with a confirmatory arthrogram effect. An anatomic illustration is provided (Figure 5).
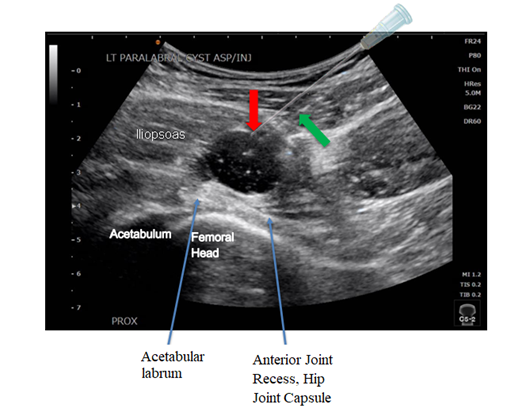
Figure 3: Ultrasound demonstrating needle trajectory (green arrow) and insertion into hypoechoic anterior paralabral cyst for needle fenestration (red arrow). A transparent needle illustration [9] is seen directly adjacent to the actual needle trajectory for ease of viewing.
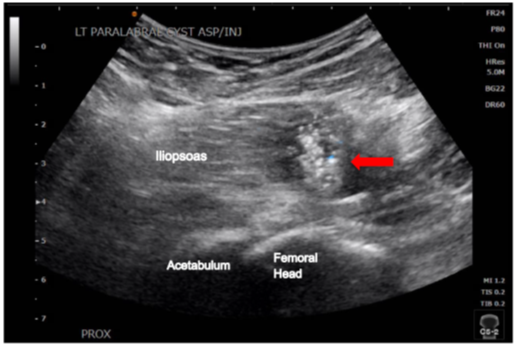
Figure 4: Ultrasound of anterior paralabral cyst status-post cyst rupture (red arrow).
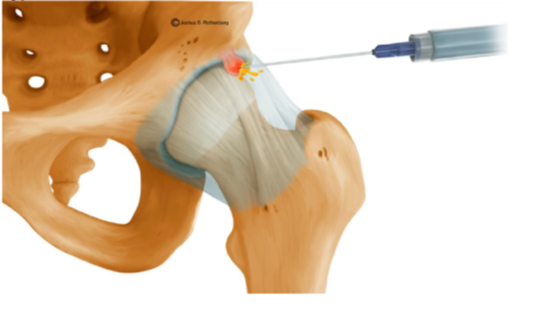
Figure 5: Anatomic illustration demonstrating cyst rupture of an anterior paralabral cyst of the hip joint.
The patient reported immediate pain relief following the procedure. No procedural complications were experienced. At six-week follow-up, the patient expressed complete resolution of his pain. He maintained being pain-free eight months post procedure. He reported being able to complete his activities of daily living without consequential pain or immobility at the end of each day. He endorsed being able to perform a Figure 4 position, ascend and descend steps, transition from sitting to standing, and remain standing for an extended duration without pain.
3. Discussion
Initial treatment of hip paralabral cysts and associated labral tears, excluding full-thickness tears, is conservative management [10] including physical therapy, NSAIDs, cyst aspiration, and corticosteroid injections (CSI). If less invasive therapies fail to produce an acceptable functional outcome, arthroscopic cyst decompression or excision with labral repair is typically pursued [5,8]. As demonstrated in this case study, U/S-guided intervention of a paralabral cyst may be a satisfactory treatment alternative that can provide immediate pain relief and functional improvement in particular cases.
In general, high-level evidence examining ultrasound-guided therapy for paralabral cysts of the hip is scarce. There are documented cases regarding U/S-guided intervention of hip paralabral cysts utilizing aspiration with or without steroid delivery [4,11]. However, difficulties in aspiration due to cyst viscosity, and high cyst recurrence rates are commonly reported [5,7,8]. It has been reported that cysts can reoccur in up to 50% of hip paralabral cyst aspirations – with or without CSI [6]. Risk factors for cyst recurrence include large cyst size, extracapsular extension, and ovoid shape (as opposed to flatter shapes) [7].
To the best of the authors’ knowledge, this is the first case study examining intentional hip paralabral cyst rupture via pressurized lidocaine delivery under ultrasound guidance. We believe this procedure may provide an alternative solution in combating paralabral cyst recurrence regardless of the cyst’s associated risk factors. The anterior paralabral cyst in our patient exhibited the previously mentioned risk factors for recurrence (large ovoid size of 3.6 × 2.1 cm and extracapsular extension into the iliopsoas), yet the patient remained symptom-free at six-week and eight-month follow-up post cyst rupture. The authors believe the cyst rupture to be the alleviating factor as the patient had failed a previous sonographically-guided cortisone injection alone.
Posing an analogous solution at a different anatomic location are studies examining intentional synovial cyst rupture of lumbar facet joints under fluoroscopic guidance. In certain studies, most patients reported immediate symptomatic improvement, and many avoided surgical interventions. However, the long-term benefits of intentional cyst rupture in lumbar facet joints are controversial [12,13].
The benefits of this intervention include safety, timeliness, potential avoidance of surgery, cost-effectiveness, and immediate clinical improvement. This technique is easily deployable for physicians familiar with ultrasound-guided interventions and may be useful in managing cysts in the hip and other anatomical locations, such as paralabral cysts in the shoulder or ganglion cysts in the wrists, hands, or feet. However, our report does have limitations. No follow-up was conducted beyond eight months, and no clinical examination was performed after six weeks post-intervention. Furthermore, despite this intervention’s safety, it carries risks similar to other needle-driven procedures, including infection, bleeding, localized nerve injury, and pain. These risks could be amplified in a patient with a large body habitus due to difficulty visualizing critical anatomy. Cyst rupture and injectate delivery also leads to localized volume expansion, posing a theoretical risk of neurovascular compression. A potential limitation to this approach is the location and size of the paralabral cyst, as it may be located near vital vascular structures.
Notably, the patient in this case did not experience any complications, and the procedure was well tolerated. The cyst was easily visualized under ultrasound and accessible with a needle in an anterolateral location, avoiding proximity to the femoral neurovascular bundle. However, not all cysts occur in the same, easily-accessible location; they could be more medial, where the proximity to the femoral neurovascular bundle would dissuade the provider. Therefore, practitioners should carefully scan these cysts pre-procedurally and note their location throughout the procedure to avoid neurovascular damage.
Regarding future considerations, this case study has raised the hypothesis that reoccurrence rates following cyst fenestration and rupture may be lower than mere aspiration alone. Thus, U/S-guided intentional cyst rupture could be a minimally invasive alternative to arthroscopic surgery in cases that do not involve full-thickness labral tears. However, control trials examining this modality are needed to effectively evaluate its efficacy and the likelihood of hip paralabral cyst recurrence.
References
- Scott E, Westermann R, Rosneck J. A posterior labral cyst associated with an anterior labral tear of the hip. Skeletal Radiol 47 (2018): 849-852.
- Batta N, Roberts D. Paralabral cyst of the hip. Reference article, Radiopaedia.org (2022).
- Magerkurth O, Jacobson JA, Girish G, et al. Paralabral cysts in the hip joint: findings at MR arthrography. Skeletal Radiol 41 (2012): 1279-1285.
- Hsiao MY, Wu CH, Lin CW, et al. Sonographic Diagnosis and Treatment of Posterior Paralabral Cyst in the Hip Joint. Pain Medicine 18 (2016): 994-995.
- Shin KY, Park SJ, Lee WS. Paralabral Cyst of the Hip Compressing Common Femoral Vein Treated with Sono-guided Cyst Aspiration Followed by Arthroscopic Labral Debridement: A Case Report. Hip Pelvis 29 (2017): 194-198.
- John H, Avneesh C, Mina G, et al. Acetabular paralabral cysts demonstrating perineural propagation. The British Journal of Radiology 95 (2022): 1136.
- Chong Y, Kwon JW, Song Y, et al. CT-guided aspiration and steroid injection of symptomatic paralabral cysts of the hip. Jpn J Radiol 33 (2015): 229-232.
- Keun-Ho L, Youn-Soo P, Seung-Jae L. Arthroscopic Treatment of Symptomatic Paralabral Cysts in the Hip. Orthopedics 36 (2013): e373-e376.
- Database Center for Life Science (DBCLS) (https://commons.wikimedia.org/wiki/File:Needle_togopic.png), "Needle togopic", https://creativecommons.org/licenses/by/3.0/legalcode
- Karadsheh M. Hip Labral Tear. OrthoBullets (2021). https://www.orthobullets.com/knee-and-sports/3097/hip-labral-tear
- Chang KV, Wu WT, Lin WT, et al. A Female Patient with Right Anterior Hip Pain: A Paralabral Cyst of the Hip. J Med Ultrasound 28 (2019): 273-274.
- Martha JF, Swaim B, Wang DA, et al. Outcome of percutaneous rupture of lumbar synovial cysts: a case series of 101 patients. The Spine Journal 9 (2009): 899-904.
- Eshraghi Y, Desai V, Cajigal Cajigal C, Tabbaa K. Outcome of Percutaneous Lumbar Synovial Cyst Rupture in Patients with Lumbar Radiculopathy. Pain Physician 19 (2016): E1019-1025.
