A Comparative Study on Efficacy of Azithromycin and Minocycline in the Treatment of Acne Vulgaris
Article Information
Farzana Afroz1*, Rashidul Hasan2, Rajib Shahriar3
1Associate Professor and Head, Department of Dermatology, Medical College for Women and Hospital, Dhaka, Bangladesh
2Associate Professor & Head, Department of Dermatology, US Bangla Medical College & Hospital, Narayanganj, Bangladesh
3Lieutenant Colonel, Department of Neurosurgery, Combined Military Hospital, Dhaka
*Corresponding author: Dr. Farzana Afroz, Associate Professor and Head, Department of Skin and Venereal Diseases, Medical College for Women and Hospital, Dhaka, Bangladesh.
Received: 05 June 2023; Accepted: 12 June 2023; Published: 21 June 2023
Citation: Farzana Afroz, Rashidul Hasan, Rajib Shahriar. A Comparative Study on Efficacy of Azithromycin and Minocycline in the Treatment of Acne Vulgaris.Journal of Biotechnology and Biomedicine. 6 (2023): 265-269.
View / Download Pdf Share at FacebookAbstract
Background: Acne is a chronic inflammatory condition of the pilosebaceous units that is also a multifactorial skin lesion. Dermatologists treat acne vulgaris, one of the most prevalent skin conditions, which primarily affects teens but can occur at any age.
Objective: The aim of the study to compare the efficacy of azithromycin and minocycline in the treatment of acne vulgaris.
Methodology: This cross-sectional study was conducted at tertiary care hospital Dhaka District from June 2021 to July 2022. A total of 120 patients diagnosed with acne regardless of age and sex. Data collection was done after approval of protocol using a semi-structured questionnaire through face-to-face interview. Data were analyzed using a computer program SPSS 25.0 version. Result: The mean (±SD) of the patients. The mean (±SD) age of the total sample was 27.26(±4.97). In Azithromycin group it was 25.97(±3.86), In Minocycline group 23.87(±7.84). The minimum age of the total sample was 16 years, maximum age was 45. Among all the patients 65% were female. The reduction in the percentage, in the number of inflammatory lesions, non-inflammatory and total lesions of post six weeks was better with azithromycin group as compared to minocycline.
Conclusion: Patients with acne who received azithromycin and minocycline separately in the current study, showed improvements in a number of criteria measuring the severity of the lesion.
Keywords
Acne Vulgaris; Azithromycin; Minocycline
Acne Vulgaris articles Acne Vulgaris Research articles Acne Vulgaris review articles Acne Vulgaris PubMed articles Acne Vulgaris PubMed Central articles Acne Vulgaris 2023 articles Acne Vulgaris 2024 articles Acne Vulgaris Scopus articles Acne Vulgaris impact factor journals Acne Vulgaris Scopus journals Acne Vulgaris PubMed journals Acne Vulgaris medical journals Acne Vulgaris free journals Acne Vulgaris best journals Acne Vulgaris top journals Acne Vulgaris free medical journals Acne Vulgaris famous journals Acne Vulgaris Google Scholar indexed journals Azithromycin articles Azithromycin Research articles Azithromycin review articles Azithromycin PubMed articles Azithromycin PubMed Central articles Azithromycin 2023 articles Azithromycin 2024 articles Azithromycin Scopus articles Azithromycin impact factor journals Azithromycin Scopus journals Azithromycin PubMed journals Azithromycin medical journals Azithromycin free journals Azithromycin best journals Azithromycin top journals Azithromycin free medical journals Azithromycin famous journals Azithromycin Google Scholar indexed journals Minocycline articles Minocycline Research articles Minocycline review articles Minocycline PubMed articles Minocycline PubMed Central articles Minocycline 2023 articles Minocycline 2024 articles Minocycline Scopus articles Minocycline impact factor journals Minocycline Scopus journals Minocycline PubMed journals Minocycline medical journals Minocycline free journals Minocycline best journals Minocycline top journals Minocycline free medical journals Minocycline famous journals Minocycline Google Scholar indexed journals Dermatologists† articles Dermatologists† Research articles Dermatologists† review articles Dermatologists† PubMed articles Dermatologists† PubMed Central articles Dermatologists† 2023 articles Dermatologists† 2024 articles Dermatologists† Scopus articles Dermatologists† impact factor journals Dermatologists† Scopus journals Dermatologists† PubMed journals Dermatologists† medical journals Dermatologists† free journals Dermatologists† best journals Dermatologists† top journals Dermatologists† free medical journals Dermatologists† famous journals Dermatologists† Google Scholar indexed journals pathogenetic mechanisms articles pathogenetic mechanisms Research articles pathogenetic mechanisms review articles pathogenetic mechanisms PubMed articles pathogenetic mechanisms PubMed Central articles pathogenetic mechanisms 2023 articles pathogenetic mechanisms 2024 articles pathogenetic mechanisms Scopus articles pathogenetic mechanisms impact factor journals pathogenetic mechanisms Scopus journals pathogenetic mechanisms PubMed journals pathogenetic mechanisms medical journals pathogenetic mechanisms free journals pathogenetic mechanisms best journals pathogenetic mechanisms top journals pathogenetic mechanisms free medical journals pathogenetic mechanisms famous journals pathogenetic mechanisms Google Scholar indexed journals erythematous papules articles erythematous papules Research articles erythematous papules review articles erythematous papules PubMed articles erythematous papules PubMed Central articles erythematous papules 2023 articles erythematous papules 2024 articles erythematous papules Scopus articles erythematous papules impact factor journals erythematous papules Scopus journals erythematous papules PubMed journals erythematous papules medical journals erythematous papules free journals erythematous papules best journals erythematous papules top journals erythematous papules free medical journals erythematous papules famous journals erythematous papules Google Scholar indexed journals pustules articles pustules Research articles pustules review articles pustules PubMed articles pustules PubMed Central articles pustules 2023 articles pustules 2024 articles pustules Scopus articles pustules impact factor journals pustules Scopus journals pustules PubMed journals pustules medical journals pustules free journals pustules best journals pustules top journals pustules free medical journals pustules famous journals pustules Google Scholar indexed journals bacterial† articles bacterial† Research articles bacterial† review articles bacterial† PubMed articles bacterial† PubMed Central articles bacterial† 2023 articles bacterial† 2024 articles bacterial† Scopus articles bacterial† impact factor journals bacterial† Scopus journals bacterial† PubMed journals bacterial† medical journals bacterial† free journals bacterial† best journals bacterial† top journals bacterial† free medical journals bacterial† famous journals bacterial† Google Scholar indexed journals Minocycline articles Minocycline Research articles Minocycline review articles Minocycline PubMed articles Minocycline PubMed Central articles Minocycline 2023 articles Minocycline 2024 articles Minocycline Scopus articles Minocycline impact factor journals Minocycline Scopus journals Minocycline PubMed journals Minocycline medical journals Minocycline free journals Minocycline best journals Minocycline top journals Minocycline free medical journals Minocycline famous journals Minocycline Google Scholar indexed journals inflammatory† articles inflammatory† Research articles inflammatory† review articles inflammatory† PubMed articles inflammatory† PubMed Central articles inflammatory† 2023 articles inflammatory† 2024 articles inflammatory† Scopus articles inflammatory† impact factor journals inflammatory† Scopus journals inflammatory† PubMed journals inflammatory† medical journals inflammatory† free journals inflammatory† best journals inflammatory† top journals inflammatory† free medical journals inflammatory† famous journals inflammatory† Google Scholar indexed journals
Article Details
Introduction
Dermatologists treat acne vulgaris, one of the most prevalent skin conditions, which primarily affects teens but can occur at any age. By definition, acne is a chronic inflammatory condition of the pilosebaceous units that is also a multifactorial skin lesion [1]. Seborrhea, comedones, erythematous papules and pustules, less frequently nodules, deep pustules or pseudocysts, and ultimately scarring in a small number of them are among the various clinical manifestations. Increased sebum production, follicular hyper keratinization, Propionibacterium acne (P. acne) colonization, and inflammation-related byproducts are the four basic pathogenetic mechanisms of acne [2-5]. Acne may negatively impair a person's mental and emotional well-being, which could result in social phobias, social disengagement, and clinical depression [6]. It often manifests as non-inflammatory lesions, inflammatory lesions, or a combination of both, usually affecting the face but occasionally also affecting the back and chest. Both closed and open comedowns make up a non-inflammatory lesion. Inflammatory lesion present in the form of erythematous macules, papules and pustules in majority of cases [7]. Follicular differentiation, excessive sebum production, Propionibacterium acnes, and inflammation are the key pathophysiology's involved in the development of acne [8]. In recent years, due to better understanding of the pathogenesis of acne, new therapeutic modalities are designed. Oral and topical treatments are both part of the general treatment for acne vulgaris [9]. Azelaic acid, Tretinoin, and Benzoyl peroxide are examples of topical therapies. Acnevulgaris is a chronic inflammatory disorder of the pilosebaceous unit that affects predominantly adolescents and young adults. It is characterized by noninflammatory, open or closed comedones and inflammatory papules, pustules, and nodules. It results from androgen-induced increased sebum production, altered keratinization, inflammation, and bacterial colonization of hair follicles byPropionibacterium acnes. [10] Itis a complex disease with multifactorial pathogenesis and considerable variation in severity.Acnedevelops in the pilosebaceous unit, composed of epidermal cells lining the hair follicle and the sebaceous gland. Acnerepresents obstruction and inflammation of the sebaceous follicles, a subtype of pilosebaceous units [11]. Gels are chosen over creams and lotions because they are typically more stable and active, and because water-based gels are less irritating [12,13]. Antibiotics used in oral therapy include Minocycline, erythromycin, azithromycin, trimethoprim, and minocycline, among others. Among them, azithromycin and Minocycline are currently widely utilized in therapeutic settings [14,15]. In the past, minocycline was thought to be more effective than other medications at treating inflammatory acne, especially when it came to Propionibacterium acnes, which is resistant to many antibiotics [16]. The aim of the study was to compare the efficacy of azithromycin and minocycline in the treatment of acne vulgaris.
Methodology
This cross-sectional study was conducted at tertiary care hospital Dhaka District from June 2021 to July 2022. A total of 120 patients diagnosed with acne regardless of age and sex. Patient who were willing to participate in the study were included in the study. Pregnant and lactating women with acne and the patients who failed to give consent were excluded from the study. The Jerry KL Tan. -developed and verified sign and symptom score system was used to grade acne cases. severity of acne was evaluated considering the number of non-inflammatory lesions, inflammatory lesions and total lesions as follows: Severity was graded as 0(None), 1 (Mild), 2 (Moderate) and 3 (Severe). Non-Inflammatory lesions: 0 (absent), 1 (100) Inflammatory lesions: 0 (absent), 1 (50) Total lesions count: 0 (absent), 1 (125). Total cases were divided into 2 groups, each group contained 60 patients. Patients of Group 1 were given Azithromycin Group 2 were given Minocycline. After a period of 6 weeks, each patient was followed up to evaluate number of non-inflammatory lesions, inflammatory lesions and total lesions count as mentioned above. The efficacy of either drug was also measured with the efficacy parameters stated above. The detail of the study was explained to each eligible respondent and consent was taken. After collection, the data were checked and cleaned, followed by editing, compiling, coding and categorizing according to the objectives and variable to detect errors and to maintain consistency, relevancy and quality control. Collected data were edited and analyzed according to the objectives and variables by IBM software- Statistical package for Social Science (SPSS 25) version. Ethical clearance was taken from the IRB of the institution.
Results
|
Age groups |
n=120 |
% |
|
≤20 |
50 |
41.66 |
|
20-29 |
59 |
49.17 |
|
30-39 |
9 |
7.5 |
|
40+ |
2 |
1.6 |
|
Here, 49.17% of the patients were aged between 20-29 years, 41.66% were ≤20, 7.5% were 30-39 and 1.6% were 40+. |
||
Table 1: Distribution of the patients by age group
|
Study group |
Mean±SD |
Minimum age |
Maximum age |
|
Total sample |
27.26±4.97 |
18 |
45 |
|
Azithromycin group (n=60) |
25.97±3.86 |
18 |
45 |
|
Minocycline group(n=60) |
23.87±7.84 |
20 |
45 |
|
Table-2 shows the mean (±SD) of the patients. The mean (±SD) age of the total sample was 27.26(±4.97). In Azithromycin group it was 25.97(±3.86), In Minocycline group 23.87(±7.84). The minimum age of the total sample was 18 years, maximum age was 45. |
|||
Table 2: Distribution of the patients by Mean, Minimum and Maximum age.
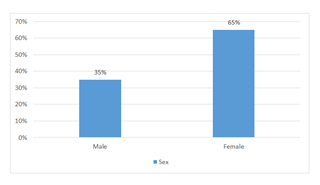
Figure 1: Distribution of the patients by sex.
According to distribution of the patients by sex, 35% patients were male, 65% patients were female.
|
Education |
n=120 |
% |
|
Primary |
10 |
8.33 |
|
Secondary |
80 |
66.67 |
|
Graduate |
30 |
25 |
|
Table-3 shows 66.67% patients completed secondary level of education, 8.33% completed primary level of education and 25% were graduate. |
||
Table 3: Distribution of the patients by Education.
|
Lesion types |
Azithromycin |
Minocycline |
P value |
Post 6 months |
Post 12 months |
|
|
(n=60) |
(n=60) |
treatment with azithromycin |
treatment with Minocycline |
|||
|
n(%) |
n(%) |
|||||
|
Non- inflammatory lesions |
0 (None) |
- |
- |
0.528 |
- |
- |
|
1-19 (mild) |
24 (40) |
20 (33.3) |
58.33 |
55 |
||
|
20-100(moderate) |
36 (60) |
40 (66.67) |
56.67 |
48 |
||
|
>100(severe) |
- |
- |
- |
- |
||
|
Inflammatory lesions |
0 (None) |
- |
1 (1.6) |
.443* |
1.6 |
1.6 |
|
1-14 (mild) |
25 (41.6) |
29 (48.33) |
60 |
55.33 |
||
|
15-50(moderate) |
35 (58.3) |
30 (50) |
40 |
38.33 |
||
|
>50(severe) |
- |
- |
- |
- |
||
|
Total lesions |
0 (None) |
- |
- |
.718* |
- |
- |
|
1-29 (mild) |
11 (18.33) |
9 (15) |
70 |
63.33 |
||
|
30-125(moderate) |
46(76.67) |
48(80) |
23.3 |
21.67 |
||
|
>125(severe) |
3 (5) |
3 (5) |
1.6 |
- |
Table-4 shows the reduction in the percentage, in the number of inflammatory lesions, non inflammatory and total lesions of post 6 months was better with azithromycin group as compared to Minocycline.
Table 4: Comparison of clinical characteristics of acne in azithromycin and Minocycline treated groups before treatment and post 1 month of treatment
Discussion
A self-limiting inflammatory condition of the pilosebaceous unit, acne vulgaris can have a chronic history. The hypersensitivity of the sebaceous glands to the normally circulating dehydroepiandrosterone (DHEA) causes it to develop during adolescence and is brought on by Propionibacterium acnes. It is a common skin disorder which can present with inflammatory and non-inflammatory lesions chiefly on the face but can also occur on the upper arms, trunk, and back. Here, it was a Prospective longitudinal study from January 2021- Decembe2021 at Medical College for Women and Hospital, Department of dermatology. Total 60 patients were participated. Patients of Group 1 were given Azithromycin Group 2 were given Minocycline. The mean (±SD) of the patients. The mean (±SD) age of the total sample was 27.26(±4.97). In Azithromycin group it was 25.97(±3.86), In Minocycline group 23.87(±7.84). The minimum age of the total sample was 16 years, maximum age was 45. Among all the patients 65% were female and 35% were male. A previous study showed at age 18, males were more likely than women to have acne, but by the time they reached the age of 23, women were more likely to have clinical acne as the frequency of acne in men gradually decreased [17]. In this study about 66.67% patients completed secondary level of education, 8.33% completed primary level of education and 25% were graduate. Here, we have studied the efficacy of two drugs used routinely in clinical practice named Azithromycin and Minocycline. The reduction in the percentage, in the number of inflammatory lesions, non-inflammatory and total lesions of post 1 month was better with azithromycin group as compared to Minocycline. Another study showed, A macrolide antibiotic with a wide therapeutic range is azithromycin. By interfering with their ability to make proteins, it stops bacteria from expanding. It prevents mRNA from being translated by binding reversibly to the bacterial ribosome's 50S subunit. Its anti-bacterial, immunomodulatory, and anti-inflammatory effects make it useful in the treatment of acne. Diarrhea, nausea, and abdominal pain are typical side effects, as well as palpitations, angina, dyspepsia, flatus, vomiting, melena, jaundice, vaginal monilia, vaginitis, nephritis, vertigo, headaches, and fatigue [18]. Because it was considered to be superior to other choices, minocycline was the antibiotic that was most frequently used to treat acne. Minocycline prescriptions for acne have decreased significantly during the past ten years. However, the recent authorization of an extended-release version (Solodyn) in the United States raises the possibility that its use will rise once more [19].
Limitations of the study
The present study was conducted in a very short period due to time constraints and funding limitations. The small sample size was also a limitation of the present study.
Conclusion
Patients with acne who received azithromycin and Minocycline separately in the current study, showed improvements in a number of criteria measuring the severity of the lesion. The reduction in the percentage, in the number of inflammatory lesions, non-inflammatory and total lesions of post 6 months was better with azithromycin group as compared to Minocycline. Studies have also demonstrated that azithromycin has a decreased frequency of negative effects [20].
Recommendation
This study can serve as a pilot to much larger research involving multiple centers that can provide a nationwide picture, validate regression models proposed in this study for future use and emphasize points to ensure better management and adherence.
Acknowledgements
The wide range of disciplines involved in a comparative study on efficacy of azithromycin and minocycline in the treatment of acne vulgaris research means that editors need much assistance from referees in the evaluation of papers submitted for publication. I would also like to be grateful to my colleagues and family who supported me and offered deep insight into the study.
Declaration
Funding
None funding sources.
Conflict of interest
The authors state that the publishing of this paper does not include any conflicts of interest.
Ethical approval
The study was approved by the informed consent of the participant patients.
References
- Simpson NB, Cunliffe WJ. Disorders of the sebaceous glands. In: Burns T, Breathnach S, Cox N, Griffiths C, editors.Rook's Text book of Dermatology.7th ed. 43 (2004): 43.1-43.75.
- Gollnick HP, Zouboulis CC, Akamatsu H, et al. Pathogenesis and pathognesis-related treatment of acne.J Dermatol 18 (1991): 489-499.
- Leyden JJ. New understanding of the pathogenesis of acne.J Am Acad Dermatol 32 (1995): 515-525.
- Plewig G, Kligman AM.Acne and Rosacea.3rd ed. New York: Springer-Verlag (2000).
- Cunliffe WJ, Gollnick HP.Acne: Diagnosis and management.1st ed. London: Martin Dunitz Ltd (2001).
- Dawson AL, Dellavalle RP. Acne Vulgaris. BMJ 346 (2013).
- Layton AM. A review on the treatment of acne vulgaris. Int J Clin Pract 60 (2006): 64-67.
- Harper JC. An update on the pathogenesis and management of acne vulgaris. J Am Acad Dermatol (2004): 5136-5138.
- Rathi KS. Acne Vulgaris Treatment: The current scenario. IJD 56 (2011): 7-13.
- Thiboutot D, Gollnick H, Bettoli V, et al. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol 60 (2009): 1-50.
- Packman AM, Brown RH, Dunlap FE, et al. Treatment of acne vulgaris: Combination of 3% erythromycin and 5% benzoyl peroxide in a gel compared to clindamycin phosphate lotion.Int J Dermatol 35 (1996): 209-211.
- Yang DJ, Quan LT, Hsu S. Topical antibacterial agents. In: Wolverton SE, editor.comprehensive dermatologic drug therapy.2nd ed. Philadelphia: Saunders Elsevier (2007): 525-546.
- Fyrand O, Jakobsen HB. Water-based versus alcohol-based benzoyl peroxide preparations in the treatment of acne vulgaris.Dermatologica 172 (1986): 263-267.
- Harrison PV. A comparison of Minocycline and minocycline in the treatment of acne vulgaris. Clin Exp Dermatol 139 (2003): 459-464.
- Bardazzi F, Savoia F, Parente G, et al. Azithromycin, a new therapeutic strategy for acne in adolscents. Dermatol Online J 13 (2007): 4.
- Ochsendorf F. Minocycline in acne vulgaris: benefits and risks. American journal of clinical dermatology 11 (2010): 327-341.
- Cunliffe WJ, Gould DJ. Prevalence of facial acne vulgaris in late adolescence and in adults. Br Med J 1 (1979): 1109-1110.
- Scheinfeld NS, Tutrone WD, Torres O, et al. Macrolides in Dermatology. Clinics in Dermatology 21 (2003): 40-49.
- Garner SE, Eady A, Bennett C, et al. Minocycline for acne vulgaris: efficacy and safety. Cochrane Database of Systematic Reviews 8 (2012).
- Kus S, Yucelten D, Aytug A. Comparison of efficacy of azithromycin vs. Minocycline in the treatment of acne vulgaris. Clinical and Experimental Dermatology 30 (2005): 215-220.
