A Combined Strategy of Vaginal Hysterectomy by Electrosurgery with Post Hysterectomy Check Laparoscopy in Benign Indications Associated with Known or Suspected Concomitant Pelvic Disease: A Retrospective Study
Article Information
Ramkrishna Purohit1*, Jay Gopal Sharma1, Devajani Meher1, Mohammed Mahmoud Samy2, Rupam Sarkar1
1Department of Obstetrics and Gynaecology, Purohit General Hospital, Odisha, India
2Department of Obstetrics and Gynaecology, Ainshams University, Cairo, Egypt
*Corresponding Author: Dr. Ramkrishna Purohit, Director, Department of Obstetrics and Gynaecology, Purohit General Hospital, Shakti Nagar, Bargarh, pin-768028, Odisha, India
Received: 20 July 2021; Accepted: 28 July 2021; Published: 07 August 2021
Citation:
Ramkrishna Purohit, Jay Gopal Sharma, Devajani Meher, Mohammed Mahmoud Samy, Rupam Sarkar. A Combined Strategy of Vaginal Hysterectomy by Electrosurgery with Post Hysterectomy Check Laparoscopy in Benign Indications Associated with Known or Suspected Concomitant Pelvic Disease: A Retrospective Study. Obstetrics and Gynecology Research 4 (2021): 166-179.
View / Download Pdf Share at FacebookAbstract
Purpose: A vaginal hysterectomy (VH) may be preferred when possible. However, VH is less than the ideal in benign cases with known or suspected concomitant pelvic disease and a laparoscopic approach of the hysterectomy may be favoured. The laparoscopic hysterectomy requires more surgical skills. The aim of the study is to demonstrate a combined strategy of vaginal hysterectomy by bipolar sealer -shear with post-hysterectomy check laparoscopy (VHPHCL) over lapa-roscopic assisted vaginal hysterectomy (LAVH) in cases with known or suspected concomitant pelvic disease.
Patients and methods: In a retrospective study in a private setup, outcomes of cases who underwent VHPHC operation were compared with cases of LAVH operation using statistical analysis and tests of the recorded data from December 2019 through January 2021.
Results: Total 574 cases underwent the hysterectomy for the benign non-prolapsed uterus below 16 weeks size. 426(74.21%) of them had no known or suspected concomitant pelvic disease 134(23.34%) cases under-went VHPHCL, and 14(2.43%) cases underwent LAVH operations. Found that, the frequency of laparoscopic surgery significantly got reduced to 17.91% after vaginal hysterectomy in the combined VHPHCL strategy compared to100% in LAVH strategy. Thus, the laparoscopic operation time significantly decreased in VHPHCL strategy compared to LAVH strategy mins (12.20 ± 5.88 (5-40) mins (95% CI=11.20-13.21) vs 34.28 ± 15.06(15-60) mins (95% CI=25.58-42.98) p-value 0.0001. Similarly, the mean total VHPHCL operation time was significantly decreased compared to mean total LAVH time (88.95 ± 28.26(50-200) mins (95% CI=84.12-93.78) vs 122.64 ± 37.82(50-190) mins (95% CI=100.80-144.48) p-value 0.0001. The VHPHCL strategy was completed with low (8-10mm of Hg) intraabdominal pressure and two abdominal ports in most cases. There was no vault dehiscence or major complicatio
Keywords
Thin Bipolar Shear in Vaginal Hysterectomy; Thick Bi-Clamp in Vaginal Hysterectomy; Post-Hysterectomy Check Laparoscopy; Suspected Extrauterine Pelvic Pathologies; Primary Trocar Insertion Under Transvaginal Endoscopic Guidance
Thin Bipolar Shear in Vaginal Hysterectomy articles Thin Bipolar Shear in Vaginal Hysterectomy Research articles Thin Bipolar Shear in Vaginal Hysterectomy review articles Thin Bipolar Shear in Vaginal Hysterectomy PubMed articles Thin Bipolar Shear in Vaginal Hysterectomy PubMed Central articles Thin Bipolar Shear in Vaginal Hysterectomy 2023 articles Thin Bipolar Shear in Vaginal Hysterectomy 2024 articles Thin Bipolar Shear in Vaginal Hysterectomy Scopus articles Thin Bipolar Shear in Vaginal Hysterectomy impact factor journals Thin Bipolar Shear in Vaginal Hysterectomy Scopus journals Thin Bipolar Shear in Vaginal Hysterectomy PubMed journals Thin Bipolar Shear in Vaginal Hysterectomy medical journals Thin Bipolar Shear in Vaginal Hysterectomy free journals Thin Bipolar Shear in Vaginal Hysterectomy best journals Thin Bipolar Shear in Vaginal Hysterectomy top journals Thin Bipolar Shear in Vaginal Hysterectomy free medical journals Thin Bipolar Shear in Vaginal Hysterectomy famous journals Thin Bipolar Shear in Vaginal Hysterectomy Google Scholar indexed journals Thick Bi-Clamp in Vaginal Hysterectomy articles Thick Bi-Clamp in Vaginal Hysterectomy Research articles Thick Bi-Clamp in Vaginal Hysterectomy review articles Thick Bi-Clamp in Vaginal Hysterectomy PubMed articles Thick Bi-Clamp in Vaginal Hysterectomy PubMed Central articles Thick Bi-Clamp in Vaginal Hysterectomy 2023 articles Thick Bi-Clamp in Vaginal Hysterectomy 2024 articles Thick Bi-Clamp in Vaginal Hysterectomy Scopus articles Thick Bi-Clamp in Vaginal Hysterectomy impact factor journals Thick Bi-Clamp in Vaginal Hysterectomy Scopus journals Thick Bi-Clamp in Vaginal Hysterectomy PubMed journals Thick Bi-Clamp in Vaginal Hysterectomy medical journals Thick Bi-Clamp in Vaginal Hysterectomy free journals Thick Bi-Clamp in Vaginal Hysterectomy best journals Thick Bi-Clamp in Vaginal Hysterectomy top journals Thick Bi-Clamp in Vaginal Hysterectomy free medical journals Thick Bi-Clamp in Vaginal Hysterectomy famous journals Thick Bi-Clamp in Vaginal Hysterectomy Google Scholar indexed journals Post-Hysterectomy Check Laparoscopy articles Post-Hysterectomy Check Laparoscopy Research articles Post-Hysterectomy Check Laparoscopy review articles Post-Hysterectomy Check Laparoscopy PubMed articles Post-Hysterectomy Check Laparoscopy PubMed Central articles Post-Hysterectomy Check Laparoscopy 2023 articles Post-Hysterectomy Check Laparoscopy 2024 articles Post-Hysterectomy Check Laparoscopy Scopus articles Post-Hysterectomy Check Laparoscopy impact factor journals Post-Hysterectomy Check Laparoscopy Scopus journals Post-Hysterectomy Check Laparoscopy PubMed journals Post-Hysterectomy Check Laparoscopy medical journals Post-Hysterectomy Check Laparoscopy free journals Post-Hysterectomy Check Laparoscopy best journals Post-Hysterectomy Check Laparoscopy top journals Post-Hysterectomy Check Laparoscopy free medical journals Post-Hysterectomy Check Laparoscopy famous journals Post-Hysterectomy Check Laparoscopy Google Scholar indexed journals Suspected Extrauterine Pelvic Pathologies articles Suspected Extrauterine Pelvic Pathologies Research articles Suspected Extrauterine Pelvic Pathologies review articles Suspected Extrauterine Pelvic Pathologies PubMed articles Suspected Extrauterine Pelvic Pathologies PubMed Central articles Suspected Extrauterine Pelvic Pathologies 2023 articles Suspected Extrauterine Pelvic Pathologies 2024 articles Suspected Extrauterine Pelvic Pathologies Scopus articles Suspected Extrauterine Pelvic Pathologies impact factor journals Suspected Extrauterine Pelvic Pathologies Scopus journals Suspected Extrauterine Pelvic Pathologies PubMed journals Suspected Extrauterine Pelvic Pathologies medical journals Suspected Extrauterine Pelvic Pathologies free journals Suspected Extrauterine Pelvic Pathologies best journals Suspected Extrauterine Pelvic Pathologies top journals Suspected Extrauterine Pelvic Pathologies free medical journals Suspected Extrauterine Pelvic Pathologies famous journals Suspected Extrauterine Pelvic Pathologies Google Scholar indexed journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance articles Primary Trocar Insertion Under Transvaginal Endoscopic Guidance Research articles Primary Trocar Insertion Under Transvaginal Endoscopic Guidance review articles Primary Trocar Insertion Under Transvaginal Endoscopic Guidance PubMed articles Primary Trocar Insertion Under Transvaginal Endoscopic Guidance PubMed Central articles Primary Trocar Insertion Under Transvaginal Endoscopic Guidance 2023 articles Primary Trocar Insertion Under Transvaginal Endoscopic Guidance 2024 articles Primary Trocar Insertion Under Transvaginal Endoscopic Guidance Scopus articles Primary Trocar Insertion Under Transvaginal Endoscopic Guidance impact factor journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance Scopus journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance PubMed journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance medical journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance free journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance best journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance top journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance free medical journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance famous journals Primary Trocar Insertion Under Transvaginal Endoscopic Guidance Google Scholar indexed journals remnantpathology articles remnantpathology Research articles remnantpathology review articles remnantpathology PubMed articles remnantpathology PubMed Central articles remnantpathology 2023 articles remnantpathology 2024 articles remnantpathology Scopus articles remnantpathology impact factor journals remnantpathology Scopus journals remnantpathology PubMed journals remnantpathology medical journals remnantpathology free journals remnantpathology best journals remnantpathology top journals remnantpathology free medical journals remnantpathology famous journals remnantpathology Google Scholar indexed journals laparoscopy articles laparoscopy Research articles laparoscopy review articles laparoscopy PubMed articles laparoscopy PubMed Central articles laparoscopy 2023 articles laparoscopy 2024 articles laparoscopy Scopus articles laparoscopy impact factor journals laparoscopy Scopus journals laparoscopy PubMed journals laparoscopy medical journals laparoscopy free journals laparoscopy best journals laparoscopy top journals laparoscopy free medical journals laparoscopy famous journals laparoscopy Google Scholar indexed journals intraoperative articles intraoperative Research articles intraoperative review articles intraoperative PubMed articles intraoperative PubMed Central articles intraoperative 2023 articles intraoperative 2024 articles intraoperative Scopus articles intraoperative impact factor journals intraoperative Scopus journals intraoperative PubMed journals intraoperative medical journals intraoperative free journals intraoperative best journals intraoperative top journals intraoperative free medical journals intraoperative famous journals intraoperative Google Scholar indexed journals postoperative articles postoperative Research articles postoperative review articles postoperative PubMed articles postoperative PubMed Central articles postoperative 2023 articles postoperative 2024 articles postoperative Scopus articles postoperative impact factor journals postoperative Scopus journals postoperative PubMed journals postoperative medical journals postoperative free journals postoperative best journals postoperative top journals postoperative free medical journals postoperative famous journals postoperative Google Scholar indexed journals transvaginal articles transvaginal Research articles transvaginal review articles transvaginal PubMed articles transvaginal PubMed Central articles transvaginal 2023 articles transvaginal 2024 articles transvaginal Scopus articles transvaginal impact factor journals transvaginal Scopus journals transvaginal PubMed journals transvaginal medical journals transvaginal free journals transvaginal best journals transvaginal top journals transvaginal free medical journals transvaginal famous journals transvaginal Google Scholar indexed journals
Article Details
1. Introduction
The vaginal hysterectomy may bepreferredwhen possible [1, 2].Thisroutemaynot be idealincaseswith known concomitant pelvic pathologies such as ovarian cyst, adnexal cyst, hydrosalpinx, broad ligament fibroids, or suspected concomitant pelvic pathologies such as adhesions, endometriosis in chronic pelvic pain, dysmenorrhea, pelvic inflammatory disease, previous pelvic operation [3-5]. These casesconventionally favour a laparoscopic approach to thehysterectomy such as LAVH or TLH [3]. The laparoscopic hysterectomy requires more surgical skills, and longer operation time than VH. To reduce the amount of laparoscopic work inthese cases, thisstudy,performed vaginal hysterectomy plus a post-hysterectomy laparoscopicsurvey of the pelvistofind,if any remnant concomitant pelvic pathology following VH.The remnantpathology was surgically treated by laparoscopy at the same time to fulfil the requirement of the patient.Therefore, theaimof this study is to demonstrate the feasibilityof a combined strategy of vaginalhysterectomyby bipolar sealer-shearwith post-hysterectomy check laparoscopy (VHPHCL) in cases with known or suspected concomitant benign pelvic pathology to simplify the laparoscopic surgery.
2. MaterialandMethods
A retrospective study was conducted in a private set up at Purohit General Hospital. From among cases of the hysterectomy for non-prolapsed benign indications, consecutive cases of VHwithPHCL (VHPHCL) performed during the period between December 2019 through January 2021 were studied. In addition, consecutive cases of the laparoscopic hysterectomy (LH) for benign indications during this period were studied. Theupperlimit ofuterussizefor all was that of 16 weeksof gestation. This study received approval from the Purohit General Hospital institutional ethics committee onDt.17.2.2021before theinclusionof the firstcase(Referenceno- 02/2021/PGHIEC). Each included candidatesignedthe written informed consent beforeundergoingtheVHPHCL and laparoscopic hysterectomy procedures. The outcome measures. Preoperative clinical characteristics, frequency of the requirement of laparoscopic surgery, laparoscopic operation time, total operation time, intraoperative and postoperative complications among others were recorded of cases who underwent VHPHCL or LH strategy. The outcomes of the VHPHCL strategy were compared with outcomes of LH using statistical analysis.
2.1 Statistical analysis
Statistical analysis was done by descriptive and inferential statistics using chi-square test and z-test to derive the difference between two means. SPSS 27.0 version and GraphPad Prism 7.0 version were used in the analysis, and p<0.05 was considered as the level of significance (p<0.05).
2.2 Operation procedure
2.2.1 Four gynaecologic surgeons performed operations:
2.2.1.1 Vaginalhysterectomywith post-hysterectomy
checklaparoscopy (VHPHCL): Vaginal hysterectomy was started using Purohit technique of vaginal hysterectomy [6]. No infiltration of normal salinemixed vasopressorssolution like adrenaline or vasopressin wasdone.The vaginocervical junction ofthe vaginal wall was incised circumferentially by bipolar shear (Figure 1) in place of the monopolar electrode [6]. A bipolar shear (cutter)isan open sealer cum divider forceps of 5mm diameter with18 cmlong triangular Maryland insert (a short version of laparoscopic forceps). Its curved inner jaw width is 0.5 -0.7mm (Xcellancemedical technologies, Mumbai, India) (Figure2). The bipolar cutter coagulates with light pressure and divides tissuegradually on increasing pressure on the handle-lever. Lateral pedicles were exposed using right-angle forceps.All the tissues including adhesions, from the cardinaluterosacral to the upper pedicles were exposed by right angleforceps, stretchedbetween the prongs of a right-angleforceps, coagulatedclose to theedgeof the uterus, and divided bybipolarshear/cutter between its prongs [6] (Figure 3). Ordinary bipolar forceps for coagulation and scissors cut in Purohit technique of vaginal hysterectomy [6], have been replaced by a single bipolar cutter. In add-ition, thebipolarcutterwasusedinplaceof the electro-surgicalbipolarvessel sealing(EBVS)clamp. Smaller steps were preferable to larger steps.Thus, the bipolar shear workedin averynarrowavailablespace with no exchange of instruments. A skeletonized uterine artery stretched between prongs of right-angle forceps was coagulated three times along its exposed length before it was divided close to the uterus [6] (Figure 4). Large fibroid uteri were decompressed using intrauterine and sub-serosal morcellation techniques with an aim to expose lateral pedicles. In cases with the previous caesarean section, a posteroanterior approach was used to dissect ureterovesical adhesions to avoid bladder injury [7, 8]. The bipolar cutter is applied close to the edge of the uterine wall to detach adhesions. In cases faced with the obliterated posterior cul-de-sac, cardinal-uterosacral-uterine arteries were to separate extraper-itionally, and then, the anteroposterior approach was used to dissect recto-uterine adhesions to avoid rectum injury [9]. The thin tip jaw of the bipolar cutter (Figure 2) releases lateral attachments of the uterus step-by-step in smaller bites. There are four applications of the right -angle forceps:when the tip of right-angle forceps is applied from the posterior aspect of the tissues (posterior application) (Figure 3), from the anterior aspectoftissue (anterior application) (Figure 5),from the lateralaspectoftissue(lateral left and right applications) (Figure 6).The target tissues were spread, coagulated, and divided by bipolar cutter between prongs of right-angle forceps (Figure 3).The uterus is separatedfrom the body usingthesebasicapplications.
Following the vaginal hysterectomy,adhered adnexa if any to the pelvic sidewall was mobilized down towards the surgeon by transvaginal mobilization technique using tactile feel before an attempt of salpingo-oophorectomy (SO) [10]. The vaginally visible adh-esion, if any was lysed between prongs of right-angle forceps using the bipolar cutter.Deaver’s retractor and fiber-optic light were used occasionally to improve the visibility of deeper fields.Indicated salpingo-oophore-ctomy or opportunistic salpingectomy was done by the bipolar cutter.Larger adnexal cysts were decompressed by suction aspiration before adnexectomy [10]. Indicated ovarian cystectomy was done to preserve the ovary.Haemostasis wasachieved. No clamp or suture was used up to thisstage.Then, the vaginally invisible upperpart of the pelvis wassurveyedby post- hyste-rectomy check laparoscopy tofind,if any remnant extrauterine pathology, and treated surgically.For pneumoperitoneum, the distalend ofaRyle’stube (keepingallholesabove thevault)wasplaced in- situ on the right side of the pelvis. The vaginal vault was closed horizontally by Allisforceps one on each side of the Ryle’s tube. Carbon dioxide gas waspassedthrough theRyle’stubetocreatepneumoperitoneum to avoid transabdominalVeres'sneedle insertion.Then, the primary intraumbilicaltrocar wasinsertedfor laparo-scopy. At laparoscopy, remnant pelvic pathology, if any was treated surgically.A laparoscopic sealer-divider forceps (a long version of the vaginal bipolar cutter, figure 2), and having the same jaws were used for laparoscopic procedures. The excised specimen, if any wasremovedvaginally.Finally, the vault was closed vaginally. Patientswere followed up to sixweeks after theoperation.
2.2.2 Primary trocar insertion under transvaginal endoscopic guidance: Inthe caseswith a long previous anterior abdominal wall scar extendingup to and above the umbilicus, and multiple previous laparotomies, a telescope withthe cannula wasinserted through the open vaginal vault. The vault was clamped by Alli’s forceps on both sides of cannula, then, the abdomen wasinflatedwithCO2 gasthrough side channel.In the Trendelenburg position, the anterior abdominal wall was inspected intraperitoneally to locatean adhesion-free safe site (Figure 7)for the insertion of the primarytrocar to avoid the visceral injury.
2.2.3 Laparoscopic hysterectomy: Laparoscopic assisted vaginal hysterectomy (LAVH) was conducted. The uterus was lysed from the anterior abdominal wall in cases of ventrofixed uterus [8]. Lysis of other pelvic adhesions was done. Upper pedicles were separated from the uterus up to the level of the uterine artery. Adnexectomy was done in indicated cases. The uterine arteries and lower attachments were separated vaginally by procedures similar to VH described above. The vault was closed vaginally. Similar to VHPHCL strategy, the long bipolar shear was used in the laparoscopic phase, and the short bipolar shear with the right angle forcep was used in the vaginal phase. Harmonic shear was also used occasionally for lysis of ventrofixed uterus from the anterior abdominal wall.

Figure 1: Showing the incision of the vaginal wall by bipolar sealer-shear(BS), CX-cervix.
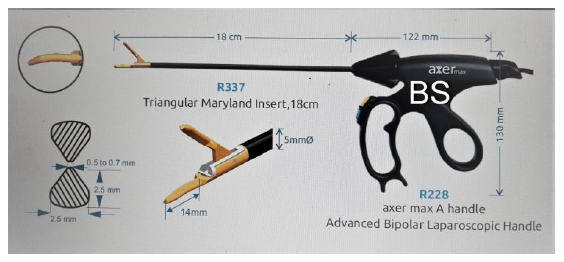
Figure 2: Showing self-explanatory different dimensions of the open bipolar sealer-shear(BS) including that of triangular curve jaws.
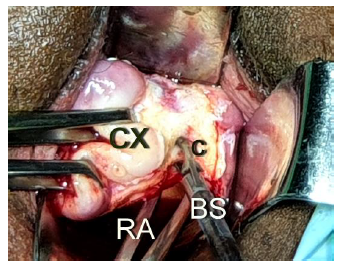
Figure 3: Showing the technique to stretch the cardinal-uterosacral ligament(C) from the posterior aspect between the prongs of a right-angle forceps(RA), to coagulate close to the edge of the uterus, and to divide by bipolar cutter(BS) between prongs of the right-angle forceps.
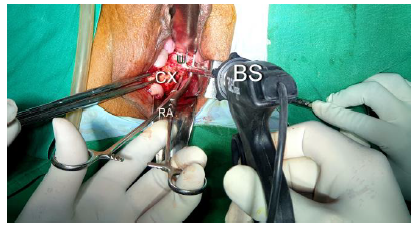
Figure 4: Showing the skeletonized left uterine artery(U), stretched between prongs of right-angle forceps(RA) from the posterior aspect, coagulated, and divided by bipolar sealer-shear(BS) close to the uterus.
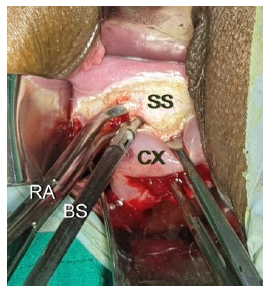
Figure 5: Showing the lateral application of the right -angle forceps(RA) to stretch and spread the supravaginal septum(SS) for the bipolar sealer-shear(BS).

Figure 6: Showing the anterior application of the right -angle forceps(RA) to stretch the anterior cul-de-sac peritoneum for the bipolar sealer-shear(BS).
3. Result
Total number of hysterectomy cases during the study period for benign non prolapsed uterus up to 16 weeks size was 574.426 (74.21%) cases had no known or suspected concomitant pelvic disease thus, underwent VH. Other cases had known or suspected concomitant pelvic disease; 134of 574 (23.34%) cases underwent VHwithPHCL, and 14(2.43%) of 574 cases underwent LAVH operations. There was no case of abdominal hysterectomy or total laparoscopic hysterectomy (TLH). The meanageofVHPHCL caseswas42.70 ± 5.01(34-50)years (95%CI=41.84-43.55).The mean age of LAVH cases was 44.92 ± 5.99(34-55) years (95% CI=41.46-48.38). Table 1 shows the preoperative clinical characteristic of the patients underwent VHPHCL and LAVH. Associated chronicpelvicpain, dysmenorrhea, pelvicinflammatory diseases, previous pelvicoperations, broad ligament fibroid, rudime-ntaryhorn ofthe uterus,or adnexaldiseases (parao-variancyst, ovarian cyst or hydrosalpinx) were theindicationsofVHPHCL. Associated chronic pelvic pain, dysmenorrhea, pelvic inflammatory disease, adnexal diseases and ventrofixed uterus (fixed adhesion of uterus to the anterior abdominal wall) (Table no1) following previous CS were the indications of LAVH [7, 8].
Table 2Shows different procedures performed during the VHPHCL. In the VHPHCL strategy, the vaginal hysterectomy was completed in all cases including cases with large uteri, previous CS, and obliterated the posterior cul-de-sac. None of the cases with previous CS had incidental detection of ventrofixed uterus. After the vaginal hysterectomy, adhered adnexa was mobilized from the pelvic sidewall andadhesiolysiswas done in 15(11.19%)cases, ovarian cystectomy was done in three (2.23%)cases. Indicatedsalpingo-oophorectomy (unilateral/bilateral) was done in 16 (11.94%)cases.Indicated salpingo-oophorectomy failed in one(0.74%). Opportunistic salpingectomy failed in five (3.73%)cases.These are due to vaginally unreach-ed upper pelvic adhesions. Table 3Shows type of lapa-roscopicproceduresperformed atPHCL and LAVH. In LAVH, 100% of cases needed laparoscopic separation of lateral pedicles and adhesions bilaterally from the uterus up to the level of uterine artery. There was no failure of hysterectomy, salpingo- oophorectomy or opportunistic salpingectomy. In the VHPHCL strategy, on the contrary, significantly, only 24(17.91%)of 134casesneededalaparoscopicsurgery after vaginal hysterectomy. The other 110(82.08%)casesdid not need anylaparoscopicprocedure, as most of the concomitant pathologies were treated surgically vaginally in these cases before going for laparoscopy. Only a checklaparoscopyor a lavage was enough tocompletethelaparoscopy (PHCL)in thesecases. In contrast to the thick lateral pedicles of the uterus and tough ventrofixed adhesions of the uterus faced in LAVH, the remnant adhesions in this 17.91% cases at PHCL weremostly soft omentaladhesionsto the lateralpelvicwall, bladderor otherpelvicorgans and easily lysed.In addition, only 4.47% the cases of failed vaginal salpingectomy and adnexectomy needed excisi-on procedures in the form of salpingectomy and adnex-ectomy at PHCL. Observed that the stumps produced using a bipolar cutter in bothVHPHCLand LAVH, finally left with the patient, physically appeared similar.
Table 4Shows the outcomes ofthe strategyofthe VHPHCL and LAVH. Interestingly,significantly, PHCLwas performed mostly using 2 ports in 97.76% cases than usually 3 ports in all LAVH procedures. The bipolar cutter coagulates anddividesanatomy in both procedures,butneeded less number ofportsand few instruments exchange in PHCL compared to LAVH. Significantly, itrequiredlow (8-10mm of Hg) intra-abdominal pressure in 82.08% to perform the laparo-scopicprocedures in theupperpart of the pelvis in PHCL compared to the requirement of standard (12-14mm of Hg) intraabdominal pressure in all of LAVH. Interestingly, the mean laparoscopic operationtime in PHCL was significantly less than that of laparoscopic operation time of LAVH (12.20 ± 5.88(5-40) mins (95% CI=11.20-13.21) vs 34.28 ± 15.06(15-60) mins (95% CI=25.58-42.98) p-value 0.0001. The laparoscopic time was minimum when the less laparoscopic procedure was needed, and increased with the increasing amount of laparoscopic surgery in both PHCL and LAVH. The mean total VHPHCL operation time was significantly less than mean total LAVH time (88.95 ± 28.26(50-200) mins (95% CI=84.12-93.78) vs 122.64 ± 37.82(50-190) mins (95% CI=100.80-144.48) p-value 0.0001. There was no failed VHPHCL or failed LAVH or subsequent laparotomic conversion. Postoperative hemoglobin fall was significantly less after VHPHCL than after LAVH (0.71 ± 0.42(0.1-2.6) Gm% (95% CI=0.64-0.79) vs 1.25 ± 0.72(0.3-2.8) Gm% (95% CI=0.83-1.67). No thermal injury to anyorgan or no major intraoperative complicationwasseenduring vaginal and laparo-scopicprocedures in both VHPHCL and LAVH. No vault dehiscence or major postoperative complication was seen following division of the vagina from the uterus by the bipolar cutter in both procedures. There was no significant difference in mean specimen uterine weight and mean hospital stay for both VHPHCL and LAVH.
|
Characteristics |
VHPHCL |
LAVH |
p-value |
||
|
N=134 |
% |
N=14 |
% |
||
|
Nulliparous |
04 |
2.98 |
0 |
0 |
|
|
Chronic pelvic pain |
46 |
34.32 |
3 |
21.4 |
0.056,NS |
|
Dysmenorrhea |
78 |
58.20 |
3 |
21.4 |
0.0001,S |
|
Uterine bleeding |
82 |
61.19 |
8 |
47.14 |
0.064,NS |
|
Previous Caesarean section |
35 |
26.11 |
10 |
71.42 |
0.0001,S |
|
1cs |
08 |
5.97 |
2 |
14.28 |
0.09,NS |
|
2cs |
22 |
16.41 |
8 |
47.14 |
0.0001,S |
|
3cs |
05 |
3.73 |
0 |
0 |
|
|
Previous pelvic laparotomy |
06 |
4.47 |
0 |
0 |
|
|
Uterus length more than 10 cm |
42 |
31.34 |
6 |
42.85 |
0.10,NS |
|
Uterus size of 12 -16 weeks |
35 |
26.11 |
6 |
42.85 |
0.01,S |
|
Fibroid uterus including broadligament fibroids |
54 |
40.29 |
5 |
25.71 |
0.05,NS |
|
Adenomyosis uterus |
49 |
36.56 |
4 |
28.57 |
0.29,NS |
|
Pelvic inflammatory disease |
21 |
15.67 |
1 |
7.14 |
0.07,NS |
|
Adnexal diseases including paraovarian cyst, ovarian cyst, hydrosalpinx |
22 |
16.41 |
1 |
7.14 |
0.07,NS |
|
Rudimentary horn of uterus with hematometra |
1 |
0.74 |
0 |
0 |
|
|
Ventrofixed uterus following previous CS |
0 |
0.00 |
8 |
57.14 |
|
Footnotes-some cases had more than one characteristic, S-significant, NS-not significant
Table 1: Preoperative characteristics of cases underwent VHPHCL and LAVH.
|
Operation procedures |
N=134 |
% |
|
VH with or without debulking |
134 |
100 |
|
Failed VH |
0 |
0 |
|
Posteroanterior approach in cases with previous CS |
35 |
26.11 |
|
Anteroposterior approach in cases with obliterated posterior cul-de-sac |
05 |
3.73 |
|
Transvaginal mobilization of adhered adnexa and vaginal adhesiolysis |
15 |
11.19 |
|
Ovarian cystectomy |
03 |
2.23 |
|
Salpingo-oophorectomy (uni or bilateral) |
16 |
11.94 |
|
Failed vaginal salpingo oophorectomy (left) |
01 |
0.74 |
|
Failed vaginal salpingectomy (uni or bilateral) |
05 |
3.73 |
Foot note: some cases had more than one procedure.
Table 2: Different surgical procedures performed during vaginal hysterectomy of VHPHCL.
|
Procedures |
PHCL |
LAVH |
p-value |
||
|
N=134 |
% |
N-14 |
% |
||
|
Laparoscopic procedure needed |
24 |
17.91 |
14 |
100 |
0.0001,S |
|
Laparoscopic procedure not needed |
110 |
82.08 |
|||
|
Adhesiolysis at PHCL -of omentum from antero- lateral pelvic wall |
10 |
7.46 |
10 |
71.42 |
0.0001,S |
|
iliac fossa, round ligament, bladder |
08 |
5.97 |
|||
|
- of sigmoid colon from lateral pelvic wall |
01 |
0.74 |
|||
|
-of rectum from appendix |
01 |
0.74 |
|||
|
Endometriotic spots coagulated |
01 |
0.74 |
|||
|
Laparoscopic salpingectomy |
05 |
3.73 |
11 |
78.57 |
0.0001,S |
|
Laparoscopic Adnexectomy |
01 |
0.74 |
3 |
21.42 |
0.0001,S |
|
Lysis of ventrofixed uterus from anterior abdominal Wall at LAVH |
0 |
0 |
8 |
57.14 |
|
Foot notes-few cases needed more than one procedure, S-significant.
Table 3: Different laparoscopic procedures performed at PHCL and LAVH.
|
Outcomes |
VHPHCL |
LAVH |
p-value |
||
|
N=134 |
% |
N=14 |
% |
||
|
Three laparoscopic ports needed |
3 |
2.23 |
14 |
100 |
0.0001,S |
|
Two laparoscopic ports needed |
131 |
97.76 |
0 |
0 |
|
|
Intraabdominal pressure: |
|||||
|
8-10mm Hg |
110 |
82.0 |
0 |
0 |
|
|
12-14mm Hg |
24 |
17.91 |
14 |
100 |
0.0001,S |
|
Age |
42.70 ± 5.01 (34-50) yrs |
(95% CI=41.84-43.55) |
44.92 ± 5.99 (34-55) yrs |
(95% CI=41.46-48.38) |
|
|
Mean VH time in minutes |
76.23 ± 24.62 (40-160) |
(95% CI=72.51-81.28) |
122.64 ± 37.82 (50-190) |
(95% CI=100. 80-144.48) |
0.0001,S |
|
Mean laparoscopy time in minute |
12.20 ± 5.88(5-40) |
(95% CI=11.20-13.21) |
34.28 ± 15.06 (15-60) |
(95% CI=25.58-42.98) |
0.0001,S |
|
Mean total Operation time in minute |
88.95 ± 28.26 (50-200) |
(95% CI=84.12-93.78) |
122.64 ± 37.82 (50-190) |
(95% CI=100. 80-144.48) |
0.0001,S |
|
Mean specimen uterus weight in gram |
179.32 ± 96. 80 (60-620) |
(95% CI =162.78-195.86) |
164.14 ± 131.20 (48-500) |
(95% CI=88.38-239.90) |
0.59,NS |
|
Mean 24 hours Hb fall in gram% |
0.71 ± 0.42(0.1-2.6) |
(95% CI=0.64-0.79) |
1.25 ± 0.72(0.3-2.8) Gm%. |
(95% CI=0.83-1.67) |
0.0001,S |
|
Mean Hospital stays in day |
2.08 ± 0.30 (2-6) days |
(95% CI=2.03-2.13) |
2.14 ± 0.36(2-3) days |
(95% CI=1.93-2.35) |
0.48,NS |
|
Failed planned hysterectomy and laparotomic conversion |
0 |
0 |
0 |
0 |
|
|
Ureter, Bladder, rectum injury |
0 |
0 |
0 |
0 |
|
|
Fever |
03 |
2.23 |
0 |
0 |
|
|
Paraesthesia of left lower limb recovered spontaneously by 5th day |
01 |
0.74 |
0 |
0 |
|
|
Vault infection in 2nd week |
02 |
1.49 |
0 |
0 |
|
|
Vault granulation at 6 weeks |
01 |
0.74 |
0 |
0 |
|
|
Any other |
00 |
0 |
0 |
0 |
|
Footnote. S-significant, NS-not significant
Table 4: Outcomes of VHPHCL and LAVH.
4. Discussion
For greater benefits, thevaginalhysterectomyshould bepreferredas the leastinvasivemethod of the hyster-ectomy for benign indications [1, 2]. It was possible in 74.21% in this study. Thisroutemaynot be ideal in caseswith known (such as ovarian cyst, adnexal cyst, hydrosalpinx, broad ligament fibroids, rudimentary horn of the uterus)or suspected concomitant pelvic pathologies (such as adhesions, endometriosis) in cases with chronic pelvic pain and dysmenorrhea (Table1) [3, 4]. The secasesconventionally favour a laparoscopic approach to thehysterectomy such as LAVH or TLH [3]. These cases constituted 23.34% in this study. The laparoscopic hysterectomy obviously requires more skill than VH.The present operating surgeons were experie-nced in vaginal hysterectomy by electrosurgery. Thus, in the place of the conventional laparoscopic hysterectomy (LAVH or TLH)in these cases, they performed the vaginal hysterectomy, and then, post-hysterectomy check laparoscopy (VHPHCL).The whole purpose was to complete the least invasive VH with additional procedures by bipolar sealer-shear before going for minimally invasive laparoscopy, to reduce the amount of laparoscopic work. When VHPHCL was not feasible in cases with ventrofixed uterus following previous CS [7, 8], or patient-surgeon decided for a laparoscopic hysterectomy, LAVH was done. It constituted 2.43% of the total cases in this study.
The outcomes of VHPHCL were compared with outcomes of LAVH in this study. In the laparo-vaginal LAVH strategy, conventionally, the laparoscopic lysis of the upper pelvic adhesions needed before the start of the hysterectomy [11]. On the contrary, in the present vagino-laparoscopic VHPHCL strategy, the upper pelvic adhesions are dissected laparoscopically after VH at PHCL. Thus, there was no need for pre-hysterectomy laparoscopic survey or surgery [9] in any case who underwent VHPHCL contrary to that in LAVH [11]. The frequency of laparoscopic surgery significantly got reduced to 17.91% after vaginal hysterectomy in the combined VHPHCL strategy compared to 100% in the LAVH strategy. Only the ventrofixation adhesions could not be reached and dissected vaginally, thus, VHPHCL was contraindicated [7, 8] therefore, LAVH was indicated and performed to separate the uterus from the anterior abdominal wall (Table 3). Technical challenges using thick electrosurgical bipolar vessel sealing(EBVS)clamp [12],and conventionalclamp-cut-sutureligation technique incaseswith narrow lateral spaces resulted in failedVH [13], subsequent laparoscopic or laparotomic conversion, and ureteric injury in previous studies [12, 13].In thisstudy, utilization of the thin tip bipolar sealer-divider with thehelpof right-angle forceps (Figure 1, 2) among others, resulted in no failed VH in allVHPHCL cases or no failed completion of avaginal phase of LAVH.The thin tip forcepsincreasedaccessto narrowlateralspace with almost no thermal injury tolateralstructures such as ureter in LAVH or VHPHCL procedures in thisstudy. There was no major risk of laparoscopy during PHCL of VHPHCL strategy in this study, and was mainly is due to minimal laparoscopic surgery following maximum vaginal surgery during VH. The Ryle’s tube inflation avoided Veres’s needle insertion in all cases of PHCL. Primary trocar insertion under transvaginal endoscopic guidance in selected risky cases of previous multiple anterior abdominal wall scars avoided port insertion trauma to viscera in this study. Except few minor complications, there were no major complications in VHPHCL and LAVH strategies in this study.
The urinary tract injuries during VH and LH as reported by a similar recent retrospective cohort study [14], in patients with large uteri below 515 grams (about 16 weeks) can be avoided by the present combined VHPHCL strategy. The concern of prolonged laparoscopic time in performing laparoscopic hysterectomy by previous studies [1, 14], can be addressed by the present combined VHPHCL strategy. The total laparoscopic time was significantly shorter in PHCL compared to the laparoscopic time of LAVH (Table 4) in this study. It is also established by a randomized controlled trial and systematic review thatVHby electrosurgery consumes less time compared
toLH, andVHusing sutures [2, 12, 15], a finding, similar to our findings.As a result, the combined VHPHCL operation time of this study is significantly shorter than the LAVH operation time (Table 4). In addition, it required low intraabdominal pressure in most cases to expose remnant pathologies in the upper part of pelvis, and is expected to reducepostoperative abdominal and shoulder pain [16] (Table 4). Also, the PHCL required mostly two ports and few accessory instruments, compared to three ports and many accessory instruments in LAVH (Table 4) and expected to reduce the cost of the accessories. Therefore, in benign cases with known or suspected concomitant pathologies, a VHPHCL strategy has many benefits over LAVH.
5. Conclusion
A combined strategy of the vaginal hysterectomy by the bipolar shear with a post-hysterectomycheck laparoscopy can be performed in place of LAVH in most of the candidates of the hysterectomy for abenign indication with known or suspected concomitant benign pelvic diseases.
Contribution to authorship
All authors qualified for authorship.
Disclosure of interests
All authors have nothing disclosure of interest to declare.
Funding
No external funding was received for the study.
Acknowledgements
The authors would like to thank Vijay Babar for statistical assistance in the planning of the study.
References
- Aarts JW, Nieboer TE, Johnson N, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst. Rev 2015 (2015)
- Evelien M Sandberg , Andries R H Twijnstra , Sara R C Driessen, et al . Total Laparoscopic Hysterectomy Versus Vaginal Hysterectomy: A Systematic Review and Meta-Analysis. J Minim Invasive Gynecol 24 (2017): 206-217.
- Anderson Ted L, Brown Jubilee. Laparoscopic and robotic -assisted hysterectomy. In: Handa V L, Van Le Linda, eds: Telinde’s Operative Gynaecology. 12th ed. Philadelphia: Wolters Kluwer (2015): 387-403.
- John Steege. Persistent or chronic pelvic pain. Telinde’s Operative Gynaecology (2008): 648-648.
- Kovac S R. Vaginal hysterectomy. In: Rock JA, Thompson JD, eds. Telinde’s Operative Gynaecology. 10th ed; Philadelphia: Lippinvott Williams and Wilkins (2008): 744-745.
- Purohit RK. Purohit technique of vaginal hysterectomy: a new approach. BJOG 110 (2003): 1115-1119.
- Purohit R, Sharma JG, Meher D, et al. A laparovaginal strategy to avoid bladder injury during laparoscopic-assisted vaginal hysterectomy in cases with ventrofixed uterus following previous caesarean section. Int J Womens Health 10 (2018): 579-587.
- Purohit RK, Sharma JG, Singh S, et al. Vaginal Hysterectomy by Electrosurgery for Benign Indications Associated with Previous Caesarean Section. J Gynecol. Surg 29 (2013): 7-12.
- Purohit R, Sharma JG, Meher D, et al. Completion of vaginal hysterectomy by electro surgery using anteroposterior approach in benign cases faced with obliterated posterior cul-de-sac. Int J Women’s Health 10 (2018): 529-536.
- Purohit R, Joshi S, Sharma JG, et al . Adnexectomy During Vaginal Hysterectomy for Benign Indications Using Bipolar Hemostasis of Lateral Pedicles and Transvaginal Adnexa Mobilization. J GYNECOL SURG 31 (2015): 86.
- Fred M Howard. Laparoscopic hysterectomy. In: Rock JA, WJ Howard, editors. Telinde’s Operative Gynecology, 10th Edition; Philadelphia: Lippinvott Williams and Wilkins (2008): 763-765.
- Allam IS, Makled AK, Gomaa IA, et al. Total laparoscopic hysterectomy, vaginal hysterectomy and total abdominal hysterectomy using electrosurgical bipolar vessel sealing technique: a randomized controlled trial. Arch Gynecol Obstet 291 (2015): 1341-1345.
- Ornella Sizzi, Pierluigi Paparella, Claudio Bonito, et al. Laparoscopic Assistance After Vaginal Hysterectomy and Unsuccessful Access to the Ovaries or Failed Uterine Mobilization: Changing Trends. JSLS 8 (2004): 339-346.
- Sybil Sailofsky, Christina Darin, Anood Alfahmy, et al. Comparison of Surgical Outcomes After Total Laparoscopic Hysterectomy or Total Vaginal Hysterectomy for Large Uteri. Obstet Gynecol 137 (2021): 445-453.
- Jamie Kroft, Amanda Selk, et al. Energy-based vessel sealing in vaginal hysterectomy: a systematic review and meta-analysis. Obstet Gynecol 118 (2011): 1127-1136.
- Radosa J C, Radosa M P, Schweitzer P A, et al. Impact of Different Intraoperative CO 2 Pressure Levels (8 and 15 mmHg) During Laparoscopic Hysterectomy Performed Due to Benign Uterine Pathologies on Postoperative Pain and Arterial pCO 2: A Prospective Randomised Controlled Clinical Trial BJOG 126 (2019): 1276-1285.
