A Case Report of Unusual Appearance of Multifocal Nodular Fatty Liver Infiltration with Hemosiderosis in A Patient with Leukemia, the Challenge in Diagnosis
Article Information
El Khaldi M1, Al Hussaini M2, Abu Shattal M1, Abu Jazar H3, Swaidan M4*
1Department of Diagnostic Radiology, King Hussein Cancer Center, Jordan
2Department of Pathology, King Hussein Cancer Center, Jordan
3Bone Marrow Transplantation and Medical Oncology departments, King Hussein Cancer Center, Jordan
4Independent researcher, Jordan
*Corresponding Author: Dr. Swaidan M, Consultant radiologist, Independent researcher, Jordan
Received: 18 January 2021; Accepted: 05 February 2021; Published: 01 March 2021
Citation: El Khaldi M, Al Hussaini M, Abu Shattal M, Abu Jazar H, Swaidan M. A Case Report of Unusual Appearance of Multifocal Nodular Fatty Liver Infiltration with Hemosiderosis in A Patient with Leukemia, the Challenge in Diagnosis. Archives of Clinical and Medical Case Reports 5 (2021): 226-233.
View / Download Pdf Share at FacebookAbstract
Hepatic steatosis is a frequent finding in computed tomography (CT) and magnetic resonance imaging (MRI). Chemotherapy is a predisposing factor for both fatty liver infiltration and hemosiderosis. Unusual appearance and behavior of multiple focal nodular fatty infiltration is rare to encounter and when associated with history of malignancy and/or infection presents a dilemma that a confident diagnosis might not be rendered by MRI thus a diagnostic biopsy would be needed to resolve the uncertainty in diagnosis. We present a patient with second relapse of acute myelogenous leukemia (AML) who developed fungal pulmonary infection while receiving salvage chemotherapy. Progressive target-shaped focal liver lesions which demonstrated characteristic fatty signal intensity on MRI were seen along with features of hemosiderosis of the liver parenchyma. Target and non-target liver tru-cut biopsies had to be performed to reach the final diagnosis of focal fatty infiltration and to rule out the differential diagnosis of liver abscesses and leukemia infiltration.
Keywords
Focal fatty infiltration; Target lesions; Magnetic resonance; Computed tomography; Leukemia; Abscess
Focal fatty infiltration articles; Target lesions articles; Magnetic resonance articles; Computed tomography articles; Leukemia articles; Abscess articles
Focal fatty infiltration articles Focal fatty infiltration Research articles Focal fatty infiltration review articles Focal fatty infiltration PubMed articles Focal fatty infiltration PubMed Central articles Focal fatty infiltration 2023 articles Focal fatty infiltration 2024 articles Focal fatty infiltration Scopus articles Focal fatty infiltration impact factor journals Focal fatty infiltration Scopus journals Focal fatty infiltration PubMed journals Focal fatty infiltration medical journals Focal fatty infiltration free journals Focal fatty infiltration best journals Focal fatty infiltration top journals Focal fatty infiltration free medical journals Focal fatty infiltration famous journals Focal fatty infiltration Google Scholar indexed journals Target lesions articles Target lesions Research articles Target lesions review articles Target lesions PubMed articles Target lesions PubMed Central articles Target lesions 2023 articles Target lesions 2024 articles Target lesions Scopus articles Target lesions impact factor journals Target lesions Scopus journals Target lesions PubMed journals Target lesions medical journals Target lesions free journals Target lesions best journals Target lesions top journals Target lesions free medical journals Target lesions famous journals Target lesions Google Scholar indexed journals Magnetic resonance articles Magnetic resonance Research articles Magnetic resonance review articles Magnetic resonance PubMed articles Magnetic resonance PubMed Central articles Magnetic resonance 2023 articles Magnetic resonance 2024 articles Magnetic resonance Scopus articles Magnetic resonance impact factor journals Magnetic resonance Scopus journals Magnetic resonance PubMed journals Magnetic resonance medical journals Magnetic resonance free journals Magnetic resonance best journals Magnetic resonance top journals Magnetic resonance free medical journals Magnetic resonance famous journals Magnetic resonance Google Scholar indexed journals PET/CT articles PET/CT Research articles PET/CT review articles PET/CT PubMed articles PET/CT PubMed Central articles PET/CT 2023 articles PET/CT 2024 articles PET/CT Scopus articles PET/CT impact factor journals PET/CT Scopus journals PET/CT PubMed journals PET/CT medical journals PET/CT free journals PET/CT best journals PET/CT top journals PET/CT free medical journals PET/CT famous journals PET/CT Google Scholar indexed journals Computed tomography articles Computed tomography Research articles Computed tomography review articles Computed tomography PubMed articles Computed tomography PubMed Central articles Computed tomography 2023 articles Computed tomography 2024 articles Computed tomography Scopus articles Computed tomography impact factor journals Computed tomography Scopus journals Computed tomography PubMed journals Computed tomography medical journals Computed tomography free journals Computed tomography best journals Computed tomography top journals Computed tomography free medical journals Computed tomography famous journals Computed tomography Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Leukemia articles Leukemia Research articles Leukemia review articles Leukemia PubMed articles Leukemia PubMed Central articles Leukemia 2023 articles Leukemia 2024 articles Leukemia Scopus articles Leukemia impact factor journals Leukemia Scopus journals Leukemia PubMed journals Leukemia medical journals Leukemia free journals Leukemia best journals Leukemia top journals Leukemia free medical journals Leukemia famous journals Leukemia Google Scholar indexed journals Abscess articles Abscess Research articles Abscess review articles Abscess PubMed articles Abscess PubMed Central articles Abscess 2023 articles Abscess 2024 articles Abscess Scopus articles Abscess impact factor journals Abscess Scopus journals Abscess PubMed journals Abscess medical journals Abscess free journals Abscess best journals Abscess top journals Abscess free medical journals Abscess famous journals Abscess Google Scholar indexed journals
Article Details
1. Introduction
Patients suffering from leukemia are prone to many short term and long term complications both from the disease and its treatment. We describe in this case report the challenges of reaching the diagnosis of a benign condition exhibiting odd behavior which required exposing the patient to biopsy to rule out more serious differential diagnosis.
2. Case Report
A 33-year-old female patient diagnosed with acute myelogenous leukemia (AML) on December 2013 (at the age of 26). She was treated with 7+3 chemotherapy protocol with Cytarabine and Idarubicin followed by high dose Cytarabine consolidation. The patient was in remission from May 2014 until January 2015 when she developed disease relapse in the bone marrow for which she was induced with Mitoxantron and Etoposide followed by allogenic peripheral hematopoietic stem cell transplantation in March 2015. The patient remained in remission until May 2020 when she was diagnosed with extramedullary myeloid sarcoma of the sacroiliac joints and of the stomach proven by biopsy. Salvage chemotherapy was started in June 2020.
Treatment was complicated in June 2020 with febrile neutropenia secondary to atypical chest infection. This was diagnosed by non-enhanced chest computed tomography (CT) scan. On the lower cuts of the chest CT scan performed in June (not shown) there were multiple target shaped liver lesions. They demonstrated a hypoattenuating rim with central iso-attenuation to the liver parenchyma. When compared to a previous follow up contrast-enhanced abdominal CT scan performed on 64 slice brilliance PHILIPS machine in 2017, the lesions had increased in size and number, which were previously reported as tiny liver cysts, and a diagnosis of fungal liver abscesses versus leukemic infiltration of the liver was suggested.
Since the patient was already receiving both chemotherapy and anti-fungal treatment for the chest infection, no further intervention at that time was undertaken. On a follow up non-enhanced chest CT scan in October 2020 using 256 iCT PHILIPS machine (Figure 1) the liver lesions remained stable after four months of treatment.
Further investigation of the liver focal lesions by magnetic resonance imaging (MRI) was performed on a Philips Ingenia 3T machine using Multihance as the intravenous contrast (IV) (Figure 2).
There was global loss of hepatic parenchymal signal intensity on long TE sequences attributed to hemosiderosis with more than 30 scattered hepatic lesions measuring up to 1.7 cm. The lesions demonstrated central iso-intense signal intensity on T2 weighted images (WI) with peripheral hyperintense signal. On T1 WI the lesions appeared hyperintense with signal drop on the out-of-phase sequence indicating the presence of fat within the lesions. The post-contrast fat saturated images showed persistent non-enhancing peripheral hypointense rim with similar enhancement of the central parts of the nodules to the liver parenchyma on the sequential images up to 90 minutes post injection of hepatobiliary specific contrast (Gd-BOPTA MultiHance from Bracco). There was no evidence of diffusion restriction within the nodules. Although the fat signal intensity is atypical for liver abscess and for leukemic infiltration of the liver, neither diagnosis could be ruled out completely. Thus, ultrasound guided target and non-target tru-cut liver biopsy was performed in December 2020, which confirmed focal steatosis of the liver from the target biopsy and a background of grade 2-3 hemosiderosis from the non-target biopsy (Figure 3).
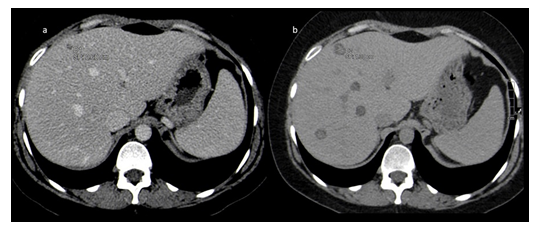
Figure 1: (a) CT scan with intravenous (IV) contrast (venous phase) on 6 March 2017 shows small hypoattenuating liver lesion measures 0.6 cm. (b) CT scan without IV contrast on 21 October 2020 shows mild increased liver attenuation due to iron overload and progression in size of the hypoattenuating liver nodule from 6 mm to 13 mm. New lesions also present.
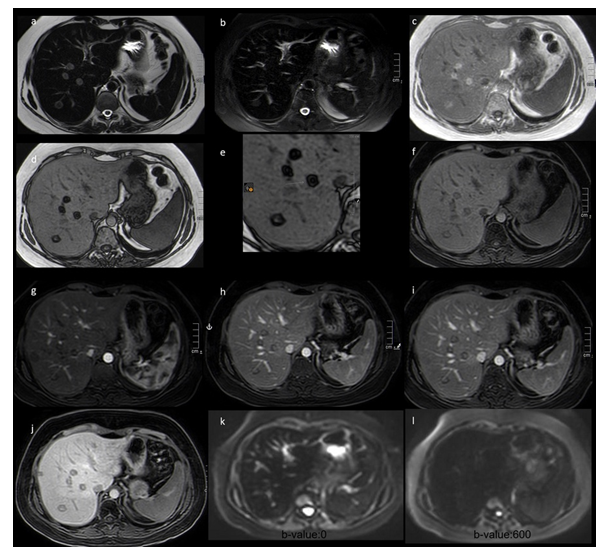
Figure 2: Abdomen MRI pre and post IV injection of 10 ml hepatobiliary specific contrast (Gd-BOPTA MultiHance Bracco). (a) Single shot fast spin echo T2 weighted image (TE: 235) shows diffuse low signal intensity of the liver parenchyma due to iron overload (hemosiderosis) and peripherally hyperintense with central iso intense liver nodules compared to the surrounding liver parenchyma. (b) Single shot fast spin echo T2 weighted Fat saturated image shows diffuse low signal intensity of the liver parenchyma due to iron overload (hemosiderosis) and liver steatosis with poorly defined faintly hyperintense focal areas corresponding to the lesions shown by CT scan. (c) 3d Gradient echo T1 weighted image in-phase (TE: 2.37) shows hyperintense nodules compared with surrounding liver parenchyma. (d and e) 3d Gradient echo T1 weighted image out-of-phase (TE: 1.19) Demonstrates hypointense liver nodules indicating signal drop which confirms the presence of fat within the nodules. They are target shaped (arrow). (f) DIXON water-only 3d Gradient echo T1 weighted image pre contrast shows iso-hypointense liver nodules. (g) DIXON water-only 3d Gradient echo T1 weighted image 20 seconds post injection of IV contrast shows hypointense liver nodules. (h) DIXON water-only 3d Gradient echo T1 weighted image 75 seconds post injection of IV contrast shows iso-hypointense liver nodules. (i) DIXON water-only 3d Gradient echo T1 weighted image 2 minutes post injection of IV contrast shows iso-hypointense liver nodules. (j) DIXON water-only 3d Gradient echo T1 weighted image 90 minutes post injection of IV hepatobiliary specific contrast (Multihance) shows iso-hypointense liver nodules. (k and l) Diffusion weighted images of b-values:0 and 600 respectively demonstrate no diffusion restriction.
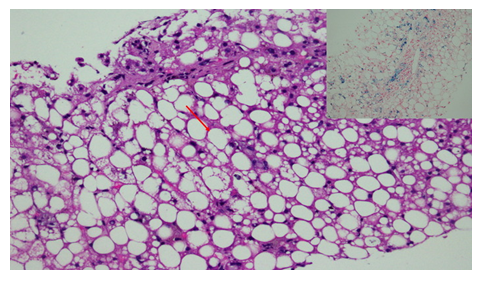
Figure 3: The hepatocytes show ballooning of the cytoplasm due to the presence of variably-sized fat droplets (arrow), (H&E X40). The inset shows iron deposition within the hepatocytes (blue color), Perls’s special stain (X40).
There was no evidence of infection or leukemic infiltration. The patient received external beam radiotherapy to the stomach and to the sacroiliac joints, which was completed on November2020, and is being prepared for the second allogeneic peripheral hematopoietic stem cell transplantation.
3. Discussion
We present the radiological findings on CT scan and MRI for the liver of a complicated case known to have extramedullary relapse of AML complicated by fungal pulmonary infection while on salvage chemotherapy showing target shaped liver lesions, which have progressed in size, and number compared to a CT scan done 3 years earlier. The lesions demonstrated MRI characteristics indicating the presence of fatty tissue within the peripheral parts of the lesions, which resulted in the target appearance. The central parts of the lesions showed imaging characteristics and enhancement pattern similar to the adjacent liver parenchyma. On the other hand, the liver parenchyma showed findings indicating hemosiderosis which is attributed to previous frequent blood transfusions. The peculiar shape of the lesions, the interval progression, although appears to be slow, and the clinical findings including the relapsed AML and active pulmonary fungal infection, caused a great deal of uncertainty to reach a confident diagnosis which resulted in undergoing ultrasound guided tru-cut target and non-target liver biopsies to reach a final diagnosis of multifocal nodular fatty liver infiltration with hemosiderosis of the liver.
In our case, the patient is under treatment for relapsed leukemia for the second time in the form of biopsy proven extramedullary myeloid sarcoma involving the sacroiliac joints and the gastric wall, as well as pulmonary fungal infection complicating chemotherapy treatment. Both of these conditions can involve the liver, and produce lesions that radiologically can be among the differential diagnosis.
The top differential diagnosis of progressive focal hypoattenuating liver lesions on CT scan in a febrile leukemic patient would be liver abscesses versus leukemia infiltration. Extramedullary tumor relapse (chloroma) in AML is more common after allogenic bone marrow transplantation, similar to the status of our patient, occurring in up to 21% of cases [1]. AML rarely involves the liver [2], and tends to have nonspecific radiological appearance [3]. When present, this is usually in the form of solitary or multiple well-defined masses, which may measure several centimeters in diameter. A much less frequent appearance is peribiliary infiltration [1].
The two major types of hepatic steatosis are nonalcoholic fatty liver disease and alcoholic fatty liver disease. Other etiologies include metabolic, nutritional, drug induced due to chemotherapy and steroids, and hepatitis C viral infection. Fatty liver infiltration is usually diffuse, but is occasionally focal. The etiology of focal type of the fatty infiltration is not well understood. However, it is suggested to be related to an alternative vascular supply that is distinct from the rest of the liver, which is not from the portal vein or the hepatic artery [4]. This however shows certain anatomical predilection within the liver, namely the gallbladder fossa, subcapsular region, adjacent to the portal vein, or falciform ligament [5]. In one study the multifocal type of fatty infiltration occurred in 22% of the patients with fatty hepatic steatosis [6]. When the focal fatty liver infiltration occurs in other than the characteristic anatomical landmarks within the liver, a confident diagnosis would be rather difficult especially in the context of malignancy and infection.
We could find only a single previous publication by Ichikawa et al. [7] describing target-shaped appearance of the focal fatty infiltration on CT scan but without mention of the same appearance on MRI. Liver MRI is very useful in identifying the fatty signal within the lesions which normally would be very helpful in suggesting the diagnosis. However, in the case of our patient, although the fatty component was demonstrated by the MRI, the dilemma of ruling out the differential diagnosis of leukemic liver infiltration and liver abscesses warranted performing a biopsy.
Focal fatty liver infiltration was described to progress to diffuse pattern [6], nonetheless progression in size and number of the focal lesions was not previously described to the best of our knowledge. In context with the clinical history of this patient, whether the progression could be related to previous chemotherapy or bone marrow transplantation, could not be confirmed and would need further study.
4. Conclusion
We describe an unusual radiological appearance of multifocal nodular fatty liver infiltration associated with hemosiderosis demonstrating target appearance of the lesions on CT scan and MRI and progression in size and number over the course of 3 years. Although fatty infiltration could be demonstrated by MRI, certain challenging cases, such as ours, may still require performing biopsy for confirming the diagnosis.
References
- Jan Fritz, Wichard Vogel, Roland Bares, et al. Radiologic Spectrum of Extramedullary Relapse of Myelogenous Leukemia in Adults. AJR 189 (2007): 209-218.
- Emily Mathewsa, Timothy Laurieb, Kenneth O’Riordanb, et al. Liver Involvement with Acute Myeloid Leukemia. Case Rep Gastroenterol 2 (2008): 121-124.
- Anderanik Tomasian, Kumar Sandrasegaran, Khaled M. Elsayes, et al. Hematologic Malignancies of the Liver: Spectrum of Disease. RadioGraphics 35 (2015): 71-86.
- Heather M. Patton, Joel E. Lavine. Review, Focal Fatty Liver: More Than Just a Radiographic Curiosity? Gastroenterology & Hepatology 3 (2007).
- Ilkay S Idilman, Ilknur Ozdeniz, Musturay Karcaaltincaba. Hepatic Steatosis: Etiology, Patterns and Quantification. Semin Ultrasound CTMRI 37 (2016): 501-510.
- Abdulla Y. El-Hassan, Ezzeldin M. Ibrahim, Fatma A, et al. Fatty infiltration of the liver: analysis of prevalence, radiological and clinical features and influence on patient management. The British Journal of Radiology 65 (1992): 114-115.
- Ichikawa T, Oh-I S, Kaira K, et al. Education and Imaging. Hepatobiliary and pancreatic. Multifocal nodular hepatic steatosis associated with the metabolic syndrome. J Gastroenterol Hepatol 22 (2007): 1693.
