A Case Report of Severe Mitral Regurgitation Due to Flail Posterior Mitral Leaflet
Article Information
Laura Piggott*, Ashling Ní Chinnéide, Laura Worthington, Paul Shiels
Cardiology Department, Midlands Regional Hospital, Tullamore, Ireland
*Corresponding Author: Laura Piggott, Cardiology Department, Midlands Regional Hospital, Tullamore, Ireland
Received: 03 August 2020; Accepted: 13 August 2020; Published: 24 September 2020
Citation: Laura Piggott, Ashling Ní Chinnéide, Laura Worthington, Paul Shiels. A Case Report of Severe Mitral Regurgitation Due to Flail Posterior Mitral Leaflet. Cardiology and Cardiovascular Medicine 4 (2020): 579-583.
View / Download Pdf Share at FacebookKeywords
Mitral valve repair; Mitral valve prolapse; Cardiac rehabilitation
Article Details
Case Presentation
Mitral valve regurgitation (MR) is recognised as the second most common valvular heart disease. We present a 62-year-old gentleman who presented to our emergency department with acute onset shortness of breath, notably worse on exertion or lying down. Background of known mitral valve prolapse and high body mass index. Patient had been engaging in intensive exercise programme prior to initial presentation. Transthoracic and transoesophageal echocardiography showed severe MR and flail P2. Patient referred and transferred to tertiary centre for mitral valve repair.
This case demonstrates the importance of consideration for monitored cardiac rehabilitation and fitness regimes in patients with multiple cardiac risk factors and known valvular heart disease.
- Importance of cardiac rehabilitation is important in the context of valvular heart disease
- Community intensive exercise programmes come with own risks
Introduction
This article reports the case of a gentleman with severe mitral regurgitation secondary to P2 rupture on a background of intensive exercise with known mitral valve disease who was successfully treated with open mitral valve repair.
Timeline
|
Timeline |
Events |
|
20th January 2020 |
Presentation with acute onset shortness of breath, orthopnoea and fatigability |
|
3rd February 2020 |
Referred to tertiary centre for angiogram and mitral valve repair |
|
7th February 2020 |
Mitral valve repair for P2 rupture |
|
11th February 2020 |
Post operative echocardiogram shows functioning MV repair. Max PG 3mmHg. Trace regurgitation. Preserved systolic function. Upper normal left heart chambers. |
|
14th February 2020 |
Discharged |
Case Presentation
A 62-year-old gentleman presented with acute onset shortness of breath, orthopnoea and fatiguability due to cardiogenic pulmonary oedema. Symptoms began on finishing work out routine in the gym as part of ongoing intensive exercise programme, having lost 40kg over the last 12 months, now weighing 120kg. His medical background history is significant for CVA 2007, atrial fibrillation, raised BMI and hypertension and mitral valve prolapse (MVP) as found during routine review. On clinical examination at presentation, he was afebrile, blood 123/79, heart rate 107, respiratory rate 25 with oxygen saturations of 82% on room air. On cardiovascular examination a 3/6 pansystolic murmur was noted with a point maximal impulse at fifth left intercostal space midclavicular line. The jugular venous pressure was elevated with pitting oedema to the mid-shin region bilaterally. Coarse inspiratory crepitations were noted bibasally. He had no other remarkable physical findings on examination.
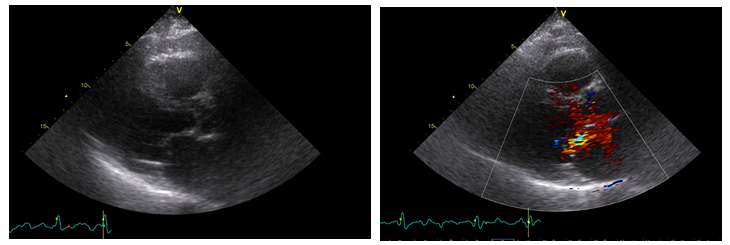
Electrocardiogram on presentation showed atrial fibrillation with a rate of 100 beats per minute. Chest radiography revealed pulmonary oedema, bilateral pleural effusions and a raised cardiothoracic ratio, confirmed on CT imaging. Subsequent transthoracic echocardiogram (TTE) showed overall good left ventricular function, ejection fraction >55%, progression of mitral valve regurgitation with anteriorly directed incompetence. Further, a transoesophgeal echocardiogram (TOE) revealed a flail posterior mitral valve leaflet, visible ruptured chordae tendinae and severe mitral regurgitation with jet extending into pulmonary veins.
Patient symptomatically improved with furosemide infusion, monitored in coronary care unit and was referred to tertiary centre for mitral valve repair. Angiogram revealed no flow limiting disease.
Discussion
Mitral regurgitation (MR) is the second most common valvular heart disease [1]. There are two well-established subdivisions of mitral regurgitation; primary, degenerative MR and secondary MR which may be due to a dilation or ischaemia [1,2]. Mitral valve prolapse (MVP) is a common disorder afflicting 2- 3% of the general population [3]. The structure and linked function of the mitral valve is complex and unlike the aortic valve its innate mechanical function cannot be easily replicated via valvular replacement, valve repair is the preferred treatment option.1 It confers various benefits such as lower impairment of left ventricular function, lack of need for anticoagulation, lower complication and post-operative mortality rates and overall better long-term results [4]. The surgical repair involves multiple steps including annuloplasty and shortening or repair of tendinous chords in addition to prolapse and leaflet resection as seen in our case.
Cardiac rehabilitation (CR) is a service available to patients diagnosed with heart disease that offers education and support in cardiovascular risk reduction strategies, health education, physical activity and stress management [5]. It is now recommended in international guidelines as an intervention in heart failure and postmyocardial infarction and stable coronary heart disease [6-8]. There is evidence that cardiac rehabilitation programmes reduce mortality, morbidity and hospital admissions. In addition, improvements in patient quality of life, exercise tolerance and well-being have been reported [5]. There are no current guidelines or recommended rehabilitation for patients with valvular heart disease such as mitral regurgitation.
It could be hypothesized that this patients acute pulmonary oedema and decompensation were secondary to a ruptured P2 leaflet secondary to intensive gym workout on a background of known MR. This highlights the importance for the need for recommended safe exercise programmes and work out intensities for community weight loss programmes in those with known valvular heart disease going forward. In addition to exercise training, cardiac rehabilitation programme could be recommended in this patient cohort to include psychological and education-based interventions. Alternative modes of CR inpatient or outpatient ambulatory delivery could include approved home-based exercise programmes and e-health programs using e.g. the Internet and mobile phones [9].
Conflict of Interest:
None declared.
References
- Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. European Heart Journal 38 (2017): 2739-2791.
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary. Journal of the American College of Cardiology 63 (2014): 2438.
- Devereux RB, Jones EC, Roman MJ, et al. Prevalence and correlates of mitral valve prolapse in a population-based sample of American Indians: the Strong Heart Study. The American Journal of Medicine 111 (2001): 679-685.
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 135 (2017): e1159-e1195.
- Rehabilitation B. The BACPR standards and core components for cardiovascular disease prevention and rehabilitation. 2nd edition 2012 (accessed 21 June 2018).
- Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation 124 (2011): 2951-2960.
- Kulik A, Ruel M, Jneid H, et al. Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation 131 (2015): 927-964.
- Roffi M, Patrono C, Collet J-P, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevationTask force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of cardiology (ESC). European Heart Journal 37 (2016): 267–315
- Bethell HJ. Cardiac rehabilitation: from Hellerstein to the millennium. International Journal of Clinical Practice 54 (2000): 92-97.